About Authors:
*Govind shukla1, Ms.Shivani prashar2, Ms. M.sarika3, Dr. Sunil Yadav4
1M.Pharm(Ph.D), Product Manager
2Sr. Product Executive, Shrey Nutraceuticals Pvt. Ltd. NewDelhi
3Product Analyst, Lactonova India Hyderabad
4Medical officer-in–charge, BPHC Bamore JHANSI U.P.
*govindbbd@gmail.com
Abstract
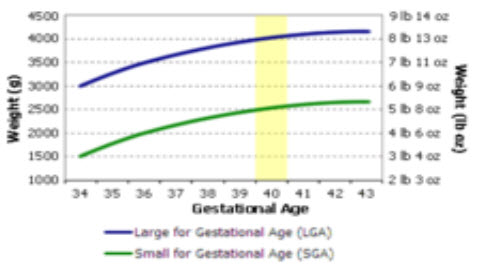
Nutrition before and during pregnancy has a profound effect on the development of infants. This is a rather critical time for healthy fetal development as infants rely heavily on maternal stores and nutrient for optimal growth and health outcome later in life. Prenatal nutrition addresses nutrient recommendations before and during pregnancy. Birth weight of the newborn at delivery reflects the sufficiency and the quality of maternal nutrient for the fetus during pregnancy. Prenatal nutrition has a strong influence on birth weight and further development of the infant.The present paper reviews the role of prenatal nutrition in pregnancy.
REFERENCE ID: PHARMATUTOR-ART-2006
Introduction
In a precursory study into the link between nutrition and pregnancy in 1950 women who consumed minimal amounts over the eight week period had a higher mortality or disorder rate concerning their offspring than women who ate regularly, attributed to the fact that the children born to well-fed mothers had less restriction within the womb.[1]
Not only have physical disorders been linked with poor nutrition before and during pregnancy, but neurological disorders and handicaps are a risk that is run by mothers who are malnourished, a condition which can also lead to the child becoming more susceptible to later degenerative disease(s).[2] 23.8% of babies are estimated to be born with lower than optimal weights at birth due to lack of proper nutrition.[3]
It is very important that expecting mothers should change their personal habits like smoking, alcohol, caffeine, using certain medications and street drugs as soon as they know they are pregnant or even when they are planning to conceive. All these can affect the development of the organs like brain, which happen in early stages of pregnancy. They can cause irreparable damage to the growing foetus.[4]
The expecting mothers should be very calm and peaceful, also focussed on what they should do for a healthy pregnancy.
Nutrition requirement before pregnancy
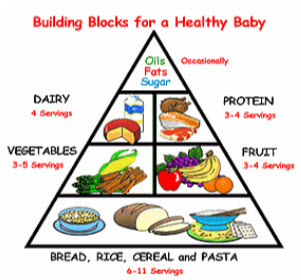
Pre-natal nutrition
As with most diets, there are chances of over-supplementing, however, as general advice, both state and medical recommendations are that mothers follow instructions listed on particular vitamin packaging as to the correct or recommended daily allowance (RDA).
* Protein is needed for the buildup of muscles, uterus, breasts, blood supply, and baby’s tissues. Low protein intake is related to smaller-than-average weight babies who may have health problems. Pregnant and breastfeeding women need around 71 grams of protein per day.
* Folate is a vitamin that is required to build protein tissues. Low folate levels are linked to birth defects, such as spina bifida. These defects form early in pregnancy, often before women know they are pregnant. The dietary reference intake for folate is 400 micrograms per day before pregnancy, 600 micrograms per day during pregnancy, and 500 micrograms per day while breastfeeding.
* Calcium is needed for strong bones. Pregnant and breastfeeding women 19 and older need around 1,000 milligrams per day or 1,300 milligrams per day for women under 19 years of age. Low zinc levels during pregnancy can cause long labor and small babies who may have health problems. The dietary reference intake for zinc is 11 milligrams per day or 12 milligrams per day for women under 19 years of age. Women who are breastfeeding need about the same amount (12 milligrams per day or 13 milligrams per day for women under 19).
* Iron deficiency is common in pregnant women. Both mother and baby need iron for their developing blood supplies. A developing baby also stores iron for use after birth. This increases the mother’s iron needs. It is practically impossible to get enough iron from food. All pregnant women need around 27 milligrams per day. The need for iron declines after birth but women who are breastfeeding still require about 10 milligrams a day.
- Magnesium and zinc supplementation for the binding of hormones at their receptor sites.
- Regular vitamin D supplementation decreases the chances of deficiencies in adolescence. More importantly, it is known to reduce the likelihood of rickets with pelvic malformations which make normal delivery impossible.
- Regular vitamin B12 supplementation, again is known to reduce the chances of infertility and ill health.
- Omega-3 fatty acids increase blood flow to reproductive organs and may help regulate reproductive hormones.[5] Consumption is also known to help prevent premature delivery and low birth weight.[6] The best dietary source of omega-3 fatty acids is oily fish. Some other omega-3 fatty acids not found in fish can be found in foods such as flaxseeds, walnuts, pumpkin seeds, and enriched eggs.[5]
- The DHA intake from an average diet during pregnancy is only 80 mg DHA per day, based on a paper in the Journal of Nutrition, 2005 (Denomme et al. 135: 206-211).
- A minimum 300 mg DHA daily is suggested based on a 1999 NIH body of experts recommending needed levels to support fetal brain development and visual acuity benefits. Most notably, the last trimester is the most critical period for DHA during pregnancy for the baby's brain growth in the womb.
- DHA (Docosahexaenoic acid, an omega-3 long chain polyunsaturated fatty acid) is found in every cell in our bodies. It is critical for brain,eye and central nervous system development and functioning. During pregnancy, developing babies rely on their mothers to get needed DHA. Since DHA is derived from the foods we eat, the content of DHA in a mother's diet determines the amount of DHA passed on to her developing baby. Unfortunately, the majority of pregnant womens fail to get the recommended amount of DHA in their diets and DHA is not found in most prenatal vitamins.
* A 2003 study published in the journal Pediatrics showed children whose mothers took a DHA supplement during pregnancy scored higher on intelligence tests at four years of age than children of mothers not taking DHA supplements.
* A 2004 study published in Child Development found that babies whose mothers had high blood levels of DHA at delivery had advanced attention spans into their second year of life. During the first six months of life these infants were two months ahead of babies whose mothers had lower DHA levels.
* Other research studies suggest breastfed babies have IQs of six to 10 points higher than formula-fed babies. Medical and nutritional experts attribute this difference to the DHA infants receive while nursing. (Obstetrics & Gynecology, 2003).
* In a trial of women receiving DHA supplementation during the third trimester, the average length of gestation increased six days (Obstetrics & Gynecology, 2003).
* Research has found low levels of DHA in mother's milk and in the red blood cells of women with postpartum depression. (Journal of Affective Disorders, 2002). Some scientists believe increasing levels of maternal DHA may reduce the risk of postpartum depression.
Nutrition requirement of mothers during pregnancy
The conception and the subsequent weeks afterwards is the time when it is at its most vulnerable, as it is the time when the organs and systems develop within. The energy used to create these systems comes from the energy and nutrients in themother's circulation, and around the lining of the womb, such is the reason whycorrect nutrient intake during pregnancy is so important.
Foetal development during pregnancy
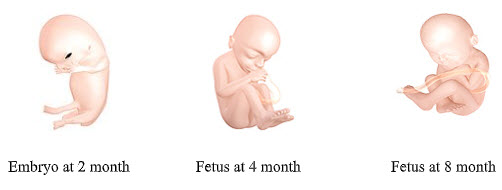
Gestation is the period of embryo development from conception to birth.Gestation is about 40 weeks in humans and is divided into three trimesters, each spanning 3 months..Gestational stages, on the other hand, are based on physiological fetal development, which include blastogenesis, embryonic stage and fetal stage.
Blastogenesisis the stage from fertilization to about 2 weeks. The fertilized egg or the zygote becomes a blastocyst where the outer layer and the inner cell mass differentiate to form placenta and the fetus respectively. Implantation occurs at this stage where the blastocyst becomes buried in the endometrium.
Embryonic stage is approximately from 2 weeks to 8 weeks. It is also in this stage where the blastocyst develops into an embryo, where all major features of human are present and operational by the end of this stage.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Fetal stage is from 9 weeks to term. During this period of time, the embryo develops rapidly and becomes a fetus. Pregnancy becomes visible at this stage.
During the early stages of pregnancy, since the placenta is not yet formed, there is no mechanism to protect the embryo from the deficiencies which may be inherent in the mother's circulation. Thus, it is critical that an adequate amount of nutrients and energy is consumed. Additionally, the frequent consumption of nutritious foods helps to prevent nausea, vomiting, and cramps.[7] Supplementing one's diet with foods rich in folic acid, such as oranges and dark green leafy vegetables, helps to prevent neural tube birth defects in the baby. Consuming foods rich in iron, such as lean red meat and beans help to prevent anemia and ensure adequate oxygen for the baby.[8] A necessary step for proper diet is to take a daily prenatal vitamins, that ensure their body gets the vitamins and minerals it needs to create a healthy baby. These vitamins contain folic acid, iodine, iron, vitamin A, vitamin D, zinc and calcium.[9]
Recommended Food hygiene during pregnancy
It is advised for pregnant women to pay special attention to food hygiene during pregnancy in addition to avoiding certain foods in order to reduce the risk of exposure to substances that may be harmful to the developing fetus. This can include food pathogens and toxic food components, alcohol, and dietary supplements such as vitamin A.[6]
Dietary vitamin A is obtained in two forms which contain the preformed vitamin (retinol), that can be found in some animal products such as liver and fish liver oils, and as a vitamin A precursor in the form of carotenes, which can be found in many fruits and vegetables.[6] Intake of retinol, in extreme cases, has been linked to birth defects and abnormalities. However, regular intake of retinol is not seen as dangerous. It is noted that a 100 g serving of liver may contain a large amount of retinol, so it is best that it is not eaten daily during pregnancy, something which is also the same with alcohol intake in binge drinking.
Excessive amounts of alcohol have been proven to cause fetal alcohol syndrome. The World Health Organization recommends that alcohol should be avoided entirely during pregnancy, given the relatively unknown effects of even small amounts of alcohol during pregnancy.[10]
Pregnant women are advised to pay particular attention to food hygiene and to avoid certain foods during pregnancy in order to minimize the risk of food poisoning from potentially harmful pathogens such as listeria, toxoplasmosis, and salmonella. Pregnant women are therefore advised to avoid foods in which high levels of the bacteria have been found, such as in soft cheeses. Listeria are destroyed by heat and therefore pregnant women are advised to reheat ready-prepared meals thoroughly. Pregnant women should also wash their fruit and vegetables very thoroughly in order to minimize risk. Salmonella poisoning is most likely to come from raw eggs or undercooked poultry.[6] Maternal obesity has a significant impact on maternal metabolism and offspring development.[11] Insulin resistance, glucose homeostasis, fat oxidation and amino acid synthesis are all disrupted by maternal obesity and contribute to adverse outcomes.[11]Modification of lifestyle is an effective intervention strategy for improvement of maternal metabolism and the prevention of adverse outcomes.[11]
Recommended prenatal nutrients during pregnancy
|
Nutrient |
Recommendation(Extra = Above RDA) |
Maximum/Total amount |
|
Energy |
Increase by 200 kcal (840 kJ) per day in last trimester only. |
RDA |
|
Proteins |
Extra 6 g per day |
51 g per day |
|
Thiamin |
Increase in line with energy; increase by 0.1 mg per day |
0.9 mg per day |
|
Riboflavin |
Needed for tissue growth; extra 0.3 mg per day |
1.4 mg per day |
|
Niacin |
Regular supplementation/diet of substance. No increase required. |
RDA |
|
Folate |
Maintain plasma levels; extra 100 µg per day |
300 µg per day |
|
Vitamin C |
Replenish drained maternal stores; extra 120 mg per day |
50 mg per day |
|
Vitamin D |
Replenish plasma levels of vitamin 10 µg per day. |
RDA |
|
Calcium |
Needs no increase |
RDA |
|
Iron |
Extra 3 mg per day needed |
RDA |
|
Magnesium, zinc, and copper |
Normal supplementation or consumption. |
RDA |
|
Iodine |
Extra 100 µg per day. |
250 µg per day[12][13][14][15] |
Folate requirement in in pre-and peri-conception.
Folic acid, which is the synthetic form of the vitamin folate, is extremely critical both in pre-and peri-conception.[6] Deficiencies in folic acid may cause neural tube defects; women who had 4 mg of folic acid in their systems due to supplementing 3 months before childbirth significantly reduced the risk of NTD within the fetus. This is now advocated by the UK department of health, recommending 400 µg per day of folic acid.
The development of every human cell is dependent on an adequate supply of folic acid. Folic acid governs the synthesis of the precursors of DNA, which is the nucleic acid that gives each cell life and character. Folic acid deficiency results in defective cellular growth and the effects are most obvious on those tissues which grow most rapidly.[16]
Leafy green vegetables, such as cabbage, broccoli and greens are all good sources of naturally occurring form of folic acid, folate.
Along with neural tube development, folate affects DNA synthesis in multiple ways. Folate is involved in the construction of purines and pyrimidines, the building blocks of nucleic acids.[17] Folate is also necessary to make s-adenosylmethionine (SAM), which acts as a methyl donor in the synthesis of DNA.[17] Because of its role in these important mechanisms, fetal DNA would be significantly altered if a maternal folate deficiency is present. One possible outcome is DNA mutation, which could prevent normal gene expression. For example, a tumor-suppressing gene might be turned off, altering normal immune function in preventing cancer growth.[17] Thompson et al.[18] examined the relationship between maternal supplementation of folate and iron during pregnancy and incidences of acute lymphoblastic leukemia (ALL) in their children. Increased rates of ALL were found in children whose mothers did not take iron and folate supplements. Iron alone did not seem to reduce the risk of developing ALL, however iron in combination with folate was shown to have a protective effect in decreasing the risk for ALL. Thompson and his associates (2001), concluded that maternal folate supplementation throughout pregnancy plays an important role in reducing the risk for childhood ALL.[18]
Water,an important aspect of nutrition throughout pregnancy.
During pregnancy, one's mass increases by about 12 kg.[19] Most of this added weight (6 to 9 L) is water[19] because the plasma volume increases, 85% of the placenta is water[20] and the fetus itself is 70-90% water. This means that hydration should also be considered an important aspect of nutrition throughout pregnancy. To ensure healthy hydration during pregnancy, the European Food Safety Authority recommends an increase of 300 mL per day compared to the normal intake for non-pregnant women, taking the total adequate water intake (from food and fluids) to 2,300 mL, or approximately 1,850 mL/ day from fluids alone.[21]
Proper nutrition is important after delivery to help the mother recover, and to provide enough food energy and nutrients for a woman to breastfeed her child. Women having serum ferritin <= 70 µg/L may need iron supplements to prevent iron deficiency anaemia during pregnancy and postpartum.[22][23]
During lactation, water intake needs increase to compensate for the loss of water through milk production. Milk is made of 88% water, and the European Food Safety Authority therefore recommends that breastfeeding women increase their water intake by about 700 mL/day, giving an adequate volume of 2,700 mL/day (from food and drink), or approximately 2,200 mL/day from fluids.[21]
Practical Recommendations for Pregnant Mothers
The following general tips can be helpful to pregnant women. It would be beneficial to maintain adequate physical activity to meet energy needs from the food consumed. Eating a balanced diet would be optimal for healthy pregnancy results. To prevent problems like dehydration and constipation, it is important to drink enough fluids, especially water, to support blood volume increases during pregnancy. It is recommended to accompany regular meals with a daily prenatal vitamin supplement that has sufficient folic acid and iron content.
If the fetus is predicted to have low birth weight, it would be ideal to increase caloric intake, which can be done by having extra Food Guide Servings daily. If the fetus is predicted to have high birth weight, smaller and more frequent meals should be consumed to allow better weight management. Moderate sugar intake, such as fruit juices, is also suggested. It is essential to limit food and beverages with high calories and salt content.
References
1.Rasmussen KM (1992). "The influence of maternal nutrition on lactation". Annual Review of Nutrition 12: 103–17.
2.Barasi EM (2003). Human Nutrition - A Health Perspective. London: Arnold.
3."WHO | 10 facts on nutrition". World Health Organization. 2011-03-15. who.int/features/factfiles/nutrition/en/. Retrieved 2011-08-07.
4. Laura Riley. Stephanie Karpinske. ed. Pregnancy: The Ultimate Week-by-Week Pregnancy Guide. Meredith Books. pp. 21–22.
5.Murkoff, Heidi (May, 20 2010). "Foods that make you fertile". Everyday Health. everydayhealth.com/pregnancy/getting-pregnant/foods-that-make-you-fertile.aspx. Retrieved 2010-11-30.
6.CS (2006). "Nutrition in pregnancy". British Nutrition Foundation 31: 28–59.
7."Common Pregnancy Concerns". OPregnancy. 3 March 2009.
8."Pregnancy Diet Plan". pregnancydietplan101.com. Retrieved April 22, 2011.
9. Laura Riley (2006-02-02). Stephanie Karpinske. ed. Pregnancy: The Ultimate Week-by-Week Pregnancy Guide. Meredith Books. pp. 21–22.
10."Framework for alcohol policy in the WHO European Region". World Health Organisation.
11.Nelson SM, Matthews P, Poston L (2010). "Maternal metabolism and obesity: modifiable determinants of pregnancy outcome". Hum. Reprod. Update 16 (3): 255–75.
12. Zimmermann MB (2007). "The adverse effects of mild-to-moderate iodine deficiency during pregnancy and childhood: a review". Thyroid 17 (9): 829–35..
13.Pérez-López FR (2007). "Iodine and thyroid hormones during pregnancy and postpartum". Gynecol. Endocrinol. 23 (7): 414–28..
14.Glinoer D (2007). "Clinical and biological consequences of iodine deficiency during pregnancy". Endocr Dev. Endocrine Development 10: 62–85..
15.Milman N, Bergholt T, Eriksen L et al. (2005). "Iron prophylaxis during pregnancy -- how much iron is needed? A randomized dose- response study of 20-80 mg ferrous iron daily in pregnant women". Acta Obstet Gynecol Scand 84 (3): 238–47.
16.Hibbard BM (August 1964). "The role of folic acid in pregnancy". An International Journal of Obstetrics and Gynaecology 71 (4): 529–42..
17.Ball, George F. M. (2004). Vitamins: Their Role in the Human Body. London: Blackwell.
18.Thompson, J.R, Fitz Gerald, P., Willoughby, M.L.N., & Armstrong, B.K. (2001). "Maternal folate supplementation in pregnancy and protection against acute lymphoblastic leukaemia in childhood". Lancet 358 (9297): 1935–1940. doi:10.1016/S0140-6736(01)06959-8.
19.Institute of Medicine (IOM). Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press, 2004.
20.Beall MH, van den Wijngaard JPHM, van Gemert MJC, Ross MG. Amniotic Fluid Water Dynamics. Placenta 2007.
21.EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA); Scientific Opinion on Dietary reference values for water. EFSA Journal 2010; 8:1459-1507.
22.Milman N, Byg KE, Bergholt T, Eriksen L, Hvas AM (2006). "Body iron and individual iron prophylaxis in pregnancy--should the iron dose be adjusted according to serum ferritin?". Ann. Hematol. 85 (9): 567–73..
23.Sethi V, Kapil U (2004). "Iodine deficiency and development of brain". Indian J Pediatr 71 (4): 325–9.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









