{ DOWNLOAD AS PDF }
 ABOUT AUHTORS
ABOUT AUHTORS
Nesar Ahmad*,Zafar Khan, Noorul Hasan, Abdul Basit, Seikh Zohrameena
Department of Pharmacology,
Faculty of Pharmacy,
Integral University, Lucknow, UP, India
*nesar50@gmail.com
ABSTRACT
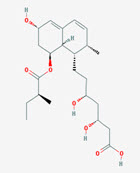
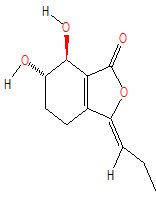
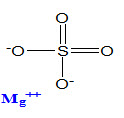
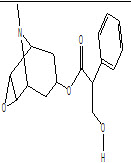
Stroke is a destructive experience which can result in permanent disability in brain. There is no permanent drug which can improve the blood flow at infracted area and also improve the neurological deficit. Due to the lack of treatments available for stroke, many researchers will investigate the suitable plants or drugs for the treatment of this disease. Numerous medicinal plants and herbal drugs are available to treat stroke, some of the plants are Ginkgo biloba, Fructus Chebulae, Pomegranate, Rosa laevigata, Garlic, Leonurus heterophyllus, Olive, Grape, Allium cepa, drugs such as Pravastatin, Senkyunolide I, Phloretin, Mgso4, HAMI 3379, Oleoylethanolamie, scopolamine and mecamylamine, Nitric Oxide, N-nitro-L-arginine methyl ester (L-NAME), 3,5,6,7,8,3’,4’-Heptamethoxy flavones, Rosiglitazone, Puerarin, the activity was estimated by parameters like superoxide dismutase (SOD) activity, Hemispheric swelling index (cerebral edema), H2O2 induced cell injury, OGD-R induced cell injury, superoxide dismutase and glutathione peroxidises, mitochondrial membrane potential, Western blotting assay, ROS scavenging assays, Superoxide anion scavenging assay, Hydroxyl radical scavenging assay, H2O2 scavenging assay, Singlet oxygen scavenging assay, Peroxyl radical scavenging assay, Peroxynitrite anion scavenging assay, myeloperoxidase (MPO) activity, blood–brain barrier integrity, cerebral infarct size, in Situ Apoptosis Detection, Western blotting, SOD, GSH, glutathione peroxidase, and MDA levels, Reverse transcription polymerase chain reaction (RT-PCR), Lactate dehydrogenase activity assay, Determination of caspase activity, acetylcholinesterase (AChE) activity, Determination of choline acetyltransferase activity (ChAT), Cell viability, Oxygen glucose deprivation/reperfusion assay, Flow cytometry, Immunohistochemistry. The present review focused on different medicinal plants and drugs that have been tested in Stroke in animal models.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2494
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 5, Issue 5 Received On: 14/02/2017; Accepted On: 23/02/2017; Published On: 01/05/2017 How to cite this article: Ahmad N, Khan Z, Hasan N, Basit A, Zohrameena S;Neuroprotective agents, Natural Plant Herbs & Drugs in Ischemic Stroke: A Review; PharmaTutor; 2017; 5(5); 29-36 |
INTRODUCTION
Stroke, the major cause of death and disability, is regarded as the important problem in developing countries [1]. Frequent incidences of cerebral ischemia are seen in age-related disorders, hypoxic–ischemic brain injury, carotid artery pathologies, asphyxiation and shock etc. It is a devastating event that is associated with great morbidity (Madl and Holzer, 2004). In certain clinical situations such as transient global cerebral ischemia anticipates or even induced iatrogenically during cardiac or thoracic surgery. Permanent ligation of bilateral common carotid arteries is a well known model used to study cerebral ischemia (Choe et al., 2001). Bilateral common carotid artery occlusion (BCCAO) causes moderate and most likely permanent reduction of cortical and cerebral blood flow in diverse areas of brain (Jeon et al., 2004).Despite the importance of stroke and the advances of technologies nowadays. The prophylactic protection against stroke with neuroprotective agents has gained much attention. Cerebral ischemia is characterized by a rapid onset of neurological injury due to interruption of blood flow to the brain [2]. This injury has been reported to be associated with the action and interaction of many factors such as excitatory amino acids, calcium overloading, and oxidative stress damage, periphery depolarization of infarction, neuroinflammation, and apoptosis [3–5]. However, accumulative lines of evidence in this decade point out to the crucial role of oxidative stress. It has been reported that the reduction of cerebral blood flow and the reperfusion period induce the elevation of oxidative stress and lipid peroxidation [6–9]. Interestingly, both in vitro and in vivo data have demonstrated that this injury can be protected by polyphenolics including flavonoids [7, 8, 10–13]. Ginkgo biloba belonging to the family Ginkgoaceae which can improve cerebral oxygen supply, decrease cerebral oxygen extraction rate and consumption, and reduce cerebral oxygen metabolic rate[14].Fructus Chebulae decreases the cerebral infarct volume and extent of hemisphere swelling[15]. Pomegranate decrease brain levels of NF-κB p65, TNF-α, caspase-3 and increased brain levels of IL-10, and cerebral ATP roduction[16]. Pravastatin drug which used for the proportion of viable neuronal cells after ischemia was greater in the pravastatin vs. control group, with greater expression of apoptotic cells in the control vs. pravastatin group. Bax protein expression was significantly decreased; Bcl-2 expression was increased, but not significantly [17]. Puerarin is a drug which is used for treatment significantly improved the phosphorylation level of AKT in dose-dependent, reduced the infarct volume, the number of Nissl body, and cleaved caspase-3 and GFAP positive cells increased [18].
Natural plants Herbs & drug used as a neuroprotection in ischemic stroke
|
Name of plant Herbs |
Dose |
Model |
Parameters |
Result |
|
Ginkgo biloba
|
1 mg/kg |
Hypoperfusin in elderly patients |
CaO2, SjvO2 and CEO2, Glua, Laca, superoxide dismutase (SOD) activity. |
Ginkgo biloba extract can improve cerebral oxygen supply, decrease cerebral oxygen extraction rate and consumption, and reduce cerebral oxygen metabolic rate [14]. |
|
Fructus Chebulae
|
300, 500 mg/kg. |
MCAO, 90min, reperfusion 24hr |
Hemispheric swelling index (cerebral edema), H2O2 induced cell injury, OGD-R induced cell injury.
|
Fructus Chebulae extract increases the PC12 cell survival against OGD-R and H2O2. Fructus Chebulae also decreases the cerebral infarct volume and extent of hemisphere swelling [15].
|
|
Pomegranate
|
250, 500 mg/kg. |
BCCAO, 60 min, Reperfusion 60 min |
Determination of brain nitric oxide, superoxide dismutase and glutathione peroxidises, glutathione reductase, brain cytokines. |
Reduction in brain contents of MDA, and NO, in addition to enhancement of SOD, GPX, and GRD. Pomegranate extract decreased brain levels of NF-κB p65, TNF-α, caspase-3 and increased brain levels of IL-10, and cerebral ATP roduction. Comet assay showed less brain DNA damage [16]. |
|
Rosa laevigata
|
50, 100 and 200 mg/kg |
MCAO reperfusion 24hr |
DAPI staining, TUNEL assay, Determination of mitochondrial membrane potential, Western blotting assay, Immunohistochemisty |
Prevented I/R-induced disability and histological damage, significantly decreased DNA fragmentation, up-regulated the expression of Bcl-2, and down-regulated the expressions of p53, 37 Apaf1, Fas, FasL, Bax, Bid, cytochrome C and active Caspase-3. Moreover, decreased the expressions of NF-jB, iNOS, MMP-9, COX-2, TNF-a, IL-1b, IL-4, IL-6, and down-regulated the levels of p-JNK, p-ERK and in MAPK pathways [19]. |
|
Garlic
|
360 mg/kg. i.p. |
MCAO for 2hr |
ROS scavenging assays, Superoxide anion scavenging assay, Hydroxyl radical scavenging assay, H2O2 scavenging assay, Singlet oxygen scavenging assay, Peroxyl radical scavenging assay, Peroxynitrite anion scavenging assay |
Extracts decreased mRNA expression of NR1- and NR2B-NMDA-receptor subunits and prevented ischemia-induced reduction in mitochondrial potential and in ATP synthesis. Antioxidants present in garlic extracts may regulate ROS concentrations during ischemia, favour pro-survival pathways, and attenuate mitochondrial dysfunction [20].
|
|
Leonurus heterophyllus
|
3.6, 7.2, 14.4 mg/kg |
MCAO for 2 hr, reperfusion 24hr |
Measurement of myeloperoxidase (MPO) activity, Measurement of NO metabolite in the brain, The apoptosis ratio of nerve fiber in the brains mensurate, |
LHAE significantly decreasing neurological deficit scores, reducing the infarct volume and MPO content. LHAE at 14.4 mg/kg significantly decreased the NO level. In addition, LHAE significantly decreased the apoptosis ratio of nerve fiber [21]. |
|
Olive
|
50, 75 and 100 mg/kg |
MCAO for 30 min, reperfusion 24hr |
Behavioural Parameter- Normal motor function, failure to extend forepaw; loss of righting reflex; no spontaneous motor activity. Biochemical parameters, Lipid profiles, Assessment of brain water content, blood–brain barrier integrity |
Oral administration of olive leaf extract reduces infarct volume, brain edema, blood–brain barrier permeability, and improves neurologic deficit scores [22].
|
|
Grape
|
30 mg/ml |
BCCAO for 5 min, reperfusion 4 days |
Behavioural parameters-Assessment of locomotor activity, Biochemical parameters- Assessment of neurons, astrocytes and microglial cells, DAPI staining to assess nuclear DNA damage, 8-OHdG immunohistochemistry to identify oxidized DNA |
GPE resulted in hyperlocomotion, extensive DND, oxidative and fragmented DNA damage, and an increase in reactive astrocytes and microglial cells in the hippocampal CA1 region[23]. |
|
Allium cepa
|
100 and 200 mg/kg |
BCCAO for 10 min, reperfusion 24 hr |
Behavioural parameters-Elevated plus maze, Inclined beam walking test, Lateral push test Biochemical parameters- Estimation of thiobarbituric acid reactive substance (TBARS), Assessment of cerebral infarct size,
|
A. cepa bulb markedly reduced cerebral infarct size and attenuated impairment in short-term memory and motor coordination. marked decrease in mitochondrial TBARS [24].
|
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
|
Drug |
Dose |
Model |
Parameters |
Result |
|
Pravastatin
|
1 mg/kg |
BCCAO for 8 min. |
In Situ Apoptosis Detection, Western blotting. |
The proportion of viable neuronal cells after ischemia was greater in the pravastatin vs. control group, with greater expression of apoptotic cells in the control vs. pravastatin group. Bax protein expression was significantly decreased whereas, Bcl-2 expression was increased, but not significantly[17]. |
|
Senkyunolide I
|
36 and 72 mg/kg |
MCAO |
Neurological function assessment, Measurement of brain water content, Detection of reporter gene activity |
SEI administration significantly ameliorated the neurological deficit, reduced the infarct volume and brain edema, reversed the cerebralmorphologicdamage,decreasedthelevels of MDA and increased the activities of superoxide dismutase [25]. |
|
Phloretin
|
20, 40, and 80 mg/kg |
MCAO |
Determination of SOD, GSH, glutathione peroxidase, and MDA levels, Reverse transcription polymerase chain reaction (RT-PCR), Western blot analysis |
Phloretin significantly reduced infarct volume, brain edema, and ameliorated neurological scores. SOD, GSH and GSH-Px activities were greatly decreased, and MDA levels significantly increased. However, phloretin pretreatment dramatically suppressed these oxidative stress processes. Furthermore, phloretin up regulated Nrf2 mRNA and protein expression [26]. |
|
Mgso4
|
1 mmol/kg |
BCCAO for 10-min reperfusion 72 hr |
Mitochondrial isolation and AFM measurement, Nissl staining |
The MgSO4 reduced the perimeter of ischemic mitochondria. The length, width and area were significantly different. Besides, the adhesion force of isolated mitochondria from the MgSO4 group was close[27].
|
|
HAMI 3379 |
0.025, 0.05, 0.1, 0.2 and 0.4 mg/kg |
MCAO for 60 min,24 or 72 hr reperfusion |
Behavioural parameters Inclined board test Biochemical parameter- Cytokine assay |
It attenuated the neurological deficits, and reduced infarct volume, brain edema, and neuronal loss and degeneration. HAMI 3379 inhibited release of the cytokines IL-1b, interferon-c (IFN-c), and tumor necrosis factor-a (TNF-a) into the serum and cerebrospinal fluid, microglial activation and neutrophil accumulation, inhibited astrocyte proliferation and reduced serum IL-4 [28]. |
|
Oleoylethanolamie |
30 mg/kg |
MCAO. For 120 min, 24 hr reperfusion |
Behavioural parameters Morris water maze test, Electrophysiological recordings, Biochemical parameters-Immunohistochemisty and cell counting, Western blot |
OEA markedly increased the expressions of brain-derived neurotrophic factor (BDNF) and peroxisome proliferator-activated receptors α(PPAR α). Chronic OEA treatment can exert functional recovery of cognitive impairments and neuroprotective effects via triggering of neurogenesis in the hippocampus [29]. |
|
scopolamine and mecamylamine
|
0.1mg/kg, 0.5mg/kg |
BCCAO for 45 min, reperfusion for 8 days. |
Behavioural parameters Morris water maze, Biochemical parameters-Lactate dehydrogenase activity assay, Determination of caspase activity, acetylcholinesterase (AChE) activity, Determination of choline acetyltransferase activity (ChAT) |
Scopolamine and mecamylamine alters memory functions following GCI/R injury substantiating the combined functional importance of both muscarinic and nicotinic receptor modulation in memory dysfunction [30]. |
|
Nitric Oxide, N-nitro-L-arginine methyl ester (L-NAME), |
|
BCCAO for 10 min, 24 h reperfusion |
Rat brain hippocampus cell dissociation, Flow cytometric analysis, infarct volume measurement, Nitric Oxide detection in vivo |
Increased NO concentration, CBF significantly. Reduced infarct size and down regulated the cell death and reduced the brain injuries [31].
|
|
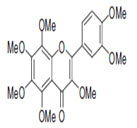
3,5,6,7,8,3’,4’-Heptamethoxy flavones
|
25 & 50 mg/kg |
BCCAO for 12min reperfusion 72 hr |
Y-maze test, Immunofluorescence for confocal microscopy |
Protected against ischemia-induced memory dysfunction, rescued neuronal cell death in the CA1 cell layer, increased the production of BDNF, stimulated the autophosphorylation of CaMK II and suppressed microglial activation in the hippocampus [32]. |
|
Rosiglitazone
|
3 mg/kg |
BCCAO reperfusion 24 or 72 hr |
Measurement of reduced glutathione (GSH) in brain tissue, Measurement of malondialdehyde (MDA) in brain tissue, Measurement of myeloperoxidase (MPO), |
PPAR-γ agonist, demonstrated preservation of cell viability of CA1 hippocampal region and attenuation of brain edema. They also showed elevated levels of GSH and low levels of the other parameters In vitro, rosiglitazone dose-dependently inhibited ROS generation by neutrophils [33].
|
|
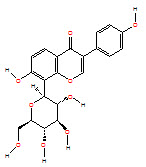
Puerarin
|
2.62, 7.86 and 23.59 mg/kg |
MCAO for 2 h |
Cell viability, Oxygen glucose deprivation/reperfusion assay, Flow cytometry, Immunohistochemistry, Western blot analysis, Nissl stain |
Puerarin treatment significantly improved the phosphorylation level of AKT in dose-dependent, reduced the infarct volume, The number of Nissl body, cleaved caspase-3 and GFAP positive cells increased [18]. |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
CONCLUSION
Stroke is a destructive experience which can result in permanent disability in brain. There is no permanent drug which can improve the blood flow at infracted area and also improve the neurological deficit. Due to the lack of treatments available for stroke, many researchers will investigated the suitable plants or drugs for the treatment of this disease. Numerous medicinal plants and herbal drugs are available to treat stroke, some of the plants are Ginkgo biloba, Fructus Chebulae, Pomegranate, Rosa laevigata, Garlic, Leonurus heterophyllus, Olive, Grape, Allium cepa, drugs.
REFERENCES
1.V. L. Feigin, “Stroke in developing countries: can the epidemic be stopped and outcomes improved?” The Lancet Neurology, vol. 6, no. 2, pp. 94–97, 2007.
2.Madl, C., Holzer, M., 2004. Brain function after resuscitation from cardiac arrest. Curr. Opin. Crit. Care 10, 213–217.
3.Choe, S.C., Kim, H.S., Jeong, T.S., Bok, S.H., Park, T.B., 2001. Naringin as an anti-atherogenic effect with the inhibition of intracellular adhesion molecule-1 in hypercholesterolemic rabbits. J. Cardiovasc. Pharmacol. 38, 947–955.
4.Jeon, S.M., Bok, S.H., Jang, M.K., Lee, M.K., Nam, K.T., Park, Y.B., Rhee, S.J., Choi, M.S., 2001. Antioxidative activity of naringin and lovastatin in high cholesterol-fed rabbits. Life Sci. 69, 2855–2866.
5.K. Baker, C. B. Marcus, K. Huf fman, H. Kruk, B. Malfroy, and S. R. Doctrow, “Synthetic combined superoxide dismu-tase/catalase mimetics are protective as a delayed treatment in a rat stroke model: a key role for reactive oxygen species in ischemic brain injury,” Journal of Pharmacology and Experimen-tal Therapeutics, vol. 284, no. 1, pp. 215–221, 1998.
6.S. Cho, E.-M. Park, M. Febbraio et al., “T he class B scavenger receptor CD36 mediates free radical production and tissue injury in cerebral ischemia,” Journal of Neuroscience, vol. 25, no. 10, pp. 2504–2512, 2005.
7.U. Dirnagl, U. Lindauer, A. Them et al., “Global cerebral ischemia in the rat: online monitoring of oxygen free radical production using chemiluminescence in vivo,” Journal of Cere-bral Blood Flow and Metabolism, vol. 15, no. 6, pp. 929–940, 1995.
8.Z. G. Zhang, X. Sun, Q. Z. Zhang, and H. Yang, “Neuroprotec-tive effects of ultra-low molecular- weight heparin oncerebral ischemia/reperfusion injury in rats: involvement of apoptosis, inflammatory reaction and energy metabolism,” International Journal of Molecular Sciences, vol. 14, pp. 1932–1939, 2013.
9.C. N. Oliver, P. E. Starke-Reed, E. R. Stadtman, G. J. Liu, J. M. Carney, and R. A. Floyd, “Oxidative damage to brain proteins, loss of glutamine synthetase activity, and production of free radicals during ischemia/reperfusion-induced injury to gerbil brain,” Proceedings of the National Academy of Sciences of the United States of America, vol. 87, no. 13, pp. 5144–5147, 1990.
10.K. A. Youdim, J. P. E. Spencer, H. Schroeter, and C. Rice-Evans, “Dietary flavonoids as potential neuroprotectants,” Biological Chemistry, vol. 383, no. 3-4, pp. 503–519, 2002.
11.J. P. E. Spencer, H. Schroeter, A. J. Crossthwaithe, G. Kuhnle, R. J. Williams, and C. Rice-Evans, “Contrasting influences of glucuronidation and O-methylation of epicatechin on hydrogen peroxide-induced cell death in neurons and fibroblasts,” Free Radical Biology and Medicine, vol. 31, no. 9, pp. 1139–1146, 2001.
12.P. H. Chan, “Role of oxidants in ischemic brain damage,” Stroke, vol. 27, no. 6, pp. 1124–1129, 1996.
13.C. Rice-Evans, “Flavonoid antioxidants,” Current Medicinal Chemistry, vol. 8, no. 7, pp. 797–807, 2001.
14.Xu, L. and Wu, F., 2015. Cryptanalysis and improvement of a user authentication scheme preserving uniqueness and anonymity for connected health care. Journal of medical systems, 39(2), p.10.
15.Gaire, B.P. and Kim, H., 2014. Neuroprotective effects of Fructus Chebulae extracts on experimental models of cerebral ischemia. Journal of Traditional Chinese Medicine, 34(1), pp.69-75.
16.Ahmed, M.A., El Morsy, E.M. and Ahmed, A.A., 2014. Pomegranate extract protects against cerebral ischemia/reperfusion injury and preserves brain DNA integrity in rats. Life sciences, 110(2), pp.61-69.
17.Jung, Y.S., Park, D.I., Kim, Y.H., Lee, J.H., Seo, P.J., Cheon, J.H., Kang, H.W. and Kim, J.W., 2015. Efficacy and safety of CT‐P13, a biosimilar of infliximab, in patients with inflammatory bowel disease: A retrospective multicenter study. Journal of gastroenterology and hepatology, 30(12), pp.1705-1712.
18.Wang, N., Zhang, Y., Wu, L., Wang, Y., Cao, Y., He, L., Li, X. and Zhao, J., 2014. Puerarin protected the brain from cerebral ischemia injury via astrocyte apoptosis inhibition. Neuropharmacology, 79, pp.282-289.
19.Zhang, S., Qi, Y., Xu, Y., Han, X., Peng, J., Liu, K. and Sun, C.K., 2013. Protective effect of flavonoid-rich extract from Rosa laevigata Michx on cerebral ischemia–reperfusion injury through suppression of apoptosis and inflammation. Neurochemistry international, 63(5), pp.522-532.
20.Cervantes, M.I., de Oca Balderas, P.M., de Jesús Gutiérrez-Baños, J., Orozco-Ibarra, M., Fernández-Rojas, B., Medina-Campos, O.N., Espinoza-Rojo, M., Ruiz-Tachiquín, M., Ortiz-Plata, A., Salazar, M.I. and Rubio-Osornio, M., 2013. Comparison of antioxidant activity of hydroethanolic fresh and aged garlic extracts and their effects on cerebral ischemia. Food chemistry, 140(1), pp.343-352.
21.Liang, H., Liu, P., Wang, Y., Song, S. and Ji, A., 2011. Protective effects of alkaloid extract from Leonurus heterophyllus on cerebral ischemia reperfusion injury by middle cerebral ischemic injury (MCAO) in rats. Phytomedicine, 18(10), pp.811-818.
22.Mohagheghi, F., Bigdeli, M.R., Rasoulian, B., Hashemi, P. and Pour, M.R., 2011. The neuroprotective effect of olive leaf extract is related to improved blood–brain barrier permeability and brain edema in rat with experimental focal cerebral ischemia. Phytomedicine, 18(2), pp.170-175.
23.Wang, Q., Chen, Z.H. and Ding, Z.X., 2009. Performance of abrasive wear of WC-12Co coatings sprayed by HVOF. Tribology International, 42(7), pp.1046-1051.
24.Kumar, A., Bora, K.S., Jaggi, A.S. and Shri, R., 2016. Comparative evaluation of neuroprotective effect of three varieties of Allium cepa in chronic constriction injury induced neuropathic pain. Thai Journal of Pharmaceutical Sciences (TJPS), 40(1).
25.Hu, Y., Duan, M., Liang, S., Wang, Y. and Feng, Y., 2015. Senkyunolide I protects rat brain against focal cerebral ischemia–reperfusion injury by up-regulating p-Erk1/2, Nrf2/HO-1 and inhibiting caspase 3. Brain research, 1605, pp.39-48.
26.Cheng, D.T., Mitchell, T.N., Zehir, A., Shah, R.H., Benayed, R., Syed, A., Chandramohan, R., Liu, Z.Y., Won, H.H., Scott, S.N. and Brannon, A.R., 2015. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. The Journal of Molecular Diagnostics, 17(3), pp.251-264.
27.Park, E., Choi, S.K., Kang, S.W., Pak, Y.K., Lee, G.J., Chung, J.H. and Park, H.K., 2015. Cerebral ischemia-induced mitochondrial changes in a global ischemic rat model by AFM. Biomedicine & Pharmacotherapy, 71, pp.15-20.
28.Shi, Q.J., Wang, H., Liu, Z.X., Fang, S.H., Song, X.M., Lu, Y.B., Zhang, W.P., Sa, X.Y., Ying, H.Z. and Wei, E.Q., 2015. HAMI 3379, a CysLT 2 R antagonist, dose-and time-dependently attenuates brain injury and inhibits microglial inflammation after focal cerebral ischemia in rats. Neuroscience, 291, pp.53-69.
29.S. S. Huang, M. C. Tsai, C. L. Chih, L. M. Hung, and S. K. Tsai, “Resveratrol reduction of infarct size in Long-Evans rats subjected to focal cerebral ischemia,” Life Sciences, vol. 69, no. 9, pp. 1057–1065, 2001.
30.Sarma, B., Ray, R.S., Mohanty, S.K. and Misra, M., 2014. Synergistic enhancement in the capacitance of nickel and cobalt based mixed oxide supercapacitor prepared by electrodeposition. Applied Surface Science, 300, pp.29-36.
31.Liu, K., Yan, M., Zheng, X. and Yang, Y., 2014. The dynamic detection of NO during the ischemic postconditioning against global cerebral ischemia/reperfusion injury. Nitric Oxide, 38, pp.17-25.
32.Okuyama, S., Morita, M., Miyoshi, K., Nishigawa, Y., Kaji, M., Sawamoto, A., Terugo, T., Toyoda, N., Makihata, N., Amakura, Y. and Yoshimura, M., 2014. 3, 5, 6, 7, 8, 3′, 4′-Heptamethoxyflavone, a citrus flavonoid, on protection against memory impairment and neuronal cell death in a global cerebral ischemia mouse model. Neurochemistry international, 70, pp.30-38.
33.Al Rouq, F. and El Eter, E., 2014. PPAR-γ activator induces neuroprotection in hypercholesterolemic rats subjected to global cerebral ischemia/reperfusion injury: In vivo and in vitro inhibition of oxidative stress. Experimental gerontology, 51, pp.1-7.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE