 ABOUT AUTHORS
ABOUT AUTHORS
Salman S. Dhankwala*, Ajinkya N. Gavsane, Prithvirj M. Ghuli, Sagar A. Jadhav
Department of Pharmaceutical Chemistry,
Appasaheb Birnale College of Pharmacy,
Sangli, Maharashtra, India
*salman.2.dhankwala@gmail.com
{ DOWNLOAD AS PDF }
ABSTRACT
Ischemic heart diseases are a major public health problem, it includes disorders of the heart and blood vessel. Ischemia is a condition in which the blood flow (and thus oxygen) is restricted or reduced in a part of the body.Cardiac ischemia is the name for decreased blood flow and oxygen to the heart muscle It's the term given to heart problems caused by narrowed heart arteries. When arteries are narrowed, less blood and oxygen reaches the heart muscle. This is also called coronary artery disease and coronary heart disease. This can ultimately lead to attack. Ischemia often causes chest pain or discomfort known as angina pectoris. Disease is diagnosed according to medical parameters; following diagnosis of the disease the treatment is started. The treatment is includes in medicines of Heart diseases and is as well as lifestyle.
Reference Id: PHARMATUTOR-ART-2584
INTRODUCTION:
Coronary artery diseases are the most common cause of sudden death. These are major health problem throughout the world and a common cause of premature morbidity and mortality, According to World Health Organization (WHO) (Kharade S.M, et al.,2014) .Approximately one third 40 million patient are suffered from these diseases. About 610,000 people die of heart disease in the united states every year–that's an 1 in every 4 deaths. (Erling Falk, et al.,1st edition)
Ischemia is a condition in which the blood flow (and thus oxygen) is restricted or reduced in a part of the body. Cardiac ischemia is the name for decreased blood flow and oxygen to the heart muscle. (Schocken DD, et al.,2015), It's the term given to heart problems caused by narrowed heart arteries. When arteries are narrowed, less blood and oxygen reaches the heart muscle. This is also called coronary artery disease and coronary heart disease. This can ultimately lead to heart attack.
In short we can say that ischemia is restriction in blood supply to tissue ,causing shortage of oxygen and needed for cellular metabolism.
Anatomy of an coronary arteries (Erling Falk, et al,.1st edition)
Coronary arteries supply blood to the heart muscle. Like all other tissues in the body, the heart muscle needs oxygen-rich blood to function. Also, oxygen-depleted blood must be carried away. The coronary arteries wrap around the outside of the heart. Small branches dive into the heart muscle to bring it blood.
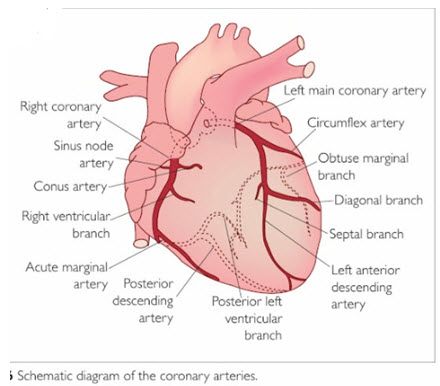
Figure 1: Anatomy of an arteries in H
eartThere is an two types of an arteries:
a) Left main coronary artery (LMCA):
The left main coronary artery supplies blood to the left side of the heart muscle (the left ventricle and left atrium). The left main coronary divides into branches: the left anterior descending artery branches off the left coronary artery and supplies blood to the front of the left side of the heart .The circumflex artery branches off the left coronary artery and encircles the heart muscle. This artery supplies blood to the outer side and back of the heart.
b) Right coronary artery (RCA):
The right coronary artery supplies blood to the right ventricle, the right atrium, and the SA (sinoatrial) and AV (atrioventricular) nodes, which regulate the heart rhythm. The right coronary artery divides into smaller branches, including the right posterior descending artery and the acute marginal artery. Together with the left anterior descending artery, the right coronary artery helps supply blood to the middle or septum of the heart.
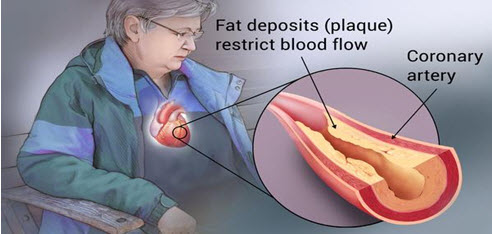
Figure 2:Fat Deposits In Plaque (Arteries) Of Heart
Coronary heart disease (CHD), previously called ischaemic heart disease, is when your coronary arteries become narrowed by a gradual build-up of fatty material within their walls. These arteries supply your heart muscle with oxygen-rich blood. ("Coronary heart disease".,2013)
This condition, known as atherosclerosis, is caused by the build up of fatty material called atheroma inside the artery walls. ( Shanthi Puska.et al.,2011)
In time, your arteries may become so narrow that they cannot deliver enough oxygen-rich blood to your heart. The pain and discomfort you may feel as a result is called angina.
If a piece of atheroma breaks off it may cause a blood clot (blockage) to form. If it blocks your coronary artery and cuts off the supply of oxygen-rich blood to your heart muscle, your heart may become permanently damaged. This is known as a heart attack.
Coronary heart disease, sometimes just called heart disease, is caused by a gradual build-up of fatty material leading to the narrowing of coronary arteries. Fatty build-up in the arteries is also known as atherosclerosis. Angina is a symptom of coronary heart disease usually characterized by pain or discomfort in the chest.
When we were formed in 1961 the total number of deaths from coronary heart disease in the UK that year was more than 160,000. But thanks in-part to BHF-funded research this number has halved. In spite of this coronary heart disease is still the single biggest cause of death in the UK. Although the death rate from coronary heart disease has come down, the burden is still great. There are now approximately 2.3 million people living with coronary heart disease in the UK. [WHO Disease and injury country estimates, 2009]
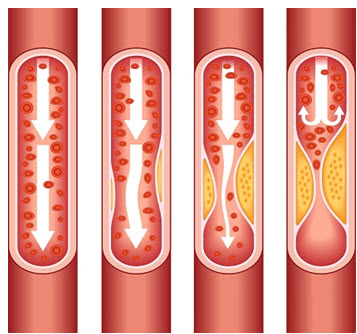
Figure 3:The interruption of an blood flow in arterial.
Classification of coronary artery diseases:
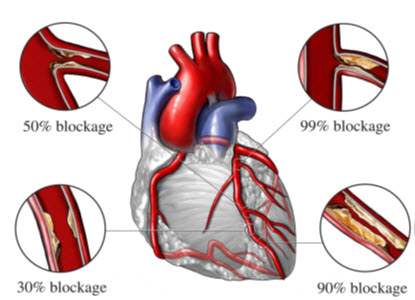
Figure 4: Classification of Coronary Artery diseases
Coronary diseases are mainly of an 3 types:
1] Obstructive coronary artery diseases:
These type of an diseases mainly cause an blockage in an arteries and by an clotting an blood it narrowed an blood vessels. In these an 30% of an blockage an done in arteries is known as obstructive coronary artery disease
2] Non-obstructive coronary artery diseases:
In these types of an diseases mainly cause an inappropriately constrict or malfunction after branching into vessels or are squeezed by overlying an heart muscles. In these type of disease the 50% of blockage is done, is known as an Non- obstructive coronary artery disease.
3] Spontaneous coronary artery dissection (SCAD):
In these type in which suddenly split in an arteries is known as spontaneous Coronary artery dissection.
Risk factors for coronary heart disease: (Kwak SM, et al.,2012)
A risk factor is something that increases your likelihood of getting a disease. There are several factors that can increase the risk of developing CHD. The main ones are:
• Smoking
• High blood pressure
• High blood cholesterol
• Diabetes
• Being physically inactive
• Being overweight or obese
• Family history of heart disease
• Ethnic background
• Sex - men are more likely to develop CHD at an earlier age than women.
• Age - the older you are, the more likely you are to develop CHD.
• The more risk factors you have, the more likely you are to develop CHD. Even though you can’t change all your risk factors, there is plenty you can do to reduce your risk and help to protect your heart. [ Kerola, AM, et al.,2012]
Signs and symptoms [Kontos, MC et al.,2010]
Chest pain that occurs regularly with activity, after eating, or at other predictable times is termed stable angina and is associated with narrowing’s of the arteries of the heart. Angina that changes in intensity, character or frequency is termed unstable. Unstable angina may precede myocardial infarction. (Kwak SM, et al.,2012)
The main symptoms are as follows:
1] Mild chest pain
2] Heaviness
3] Tightness
4] Burning
5] Squeezing
The image showing the difference between the normal and affected blood artery:

Pathophysiology:
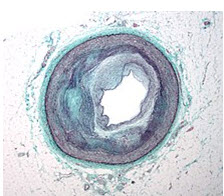
Figure 5: Macrography of an Coronary Artery In Disease
Micrograph is a coronary artery with the most common form of coronary artery disease (atherosclerosis) and marked luminal narrowing. Masson's trichrome . Limitation of blood flow to the heart causes ischemia (cell starvation secondary to a lack of oxygen) of the heart's muscle cells. The heart's muscle cells may die from lack of oxygen and this is called a myocardial infarction (commonly referred to as a heart attack). It leads to damage, death, and eventual scarring of the heart muscle without a regrowth of heart muscle cells. Chronic high-grade narrowing of the coronary arteries can induce transient ischemia which leads to the induction of a ventricular arrhythmia, which may terminate into a dangerous heart rhythm known as ventricular fibrillation, which often leads to death. (Ambrose, John et al.,2015)
Typically, coronary artery disease occurs when part of the smooth, elastic lining inside a coronary artery (the arteries that supply blood to the heart muscle) develops atherosclerosis. With atherosclerosis, the artery's lining becomes hardened, stiffened, and accumulates deposits of calcium, fatty lipids, and abnormal inflammatory cells – to form a plaque. Calcium phosphate (hydroxyapatite) deposits in the muscular layer of the blood vessels appear to play a significant role in stiffening the arteries and inducing the early phase of coronary arteriosclerosis. This can be seen in a so-called metastatic mechanism of calciphylaxis as it occurs in kidney diseases and hemodialysis (Rainer Liedtke 2008).
Although these people suffer from a kidney dysfunction, almost fifty percent of them die due to coronary artery disease. Plaques can be thought of as large "pimples" that protrude into the channel of an artery, causing a partial obstruction to blood flow. People with coronary artery disease might have just one or two plaques, or might have dozens distributed throughout their coronary arteries. A more severe form is chronic total occlusion (CTO) when a coronary artery is completely obstructed for more than 3 months.
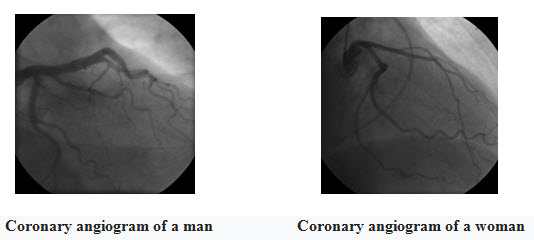
Figure 6: Coronary Angiogram of Man And Women
For symptomatic people, stress echocardiography can be used to make a diagnosis for obstructive coronary artery disease. The use of echocardiography, stress cardiac imaging, and/or advanced non-invasive imaging is not recommended on individuals who are exhibiting no symptoms and are otherwise at low risk for developing coronary disease. (American College of Cardiology 2013)
The main diagnosis for an coronary are as follows:
1] Baseline electrocardiography (ECG)
2] Exercise ECG – Stress test
3] Exercise radioisotope test (nuclear stress test, myocardial scintigraphy)
4] Echocardiography (including stress echocardiography)
5]Coronary angiography.
Coronary Artery Bypass Surgery.

A surgeon creates a graft to bypass blocked coronary arteries using a vessel from another part of your body. This allows blood to flow around the blocked or narrowed coronary artery. Because this requires open-heart surgery, it's most often reserved for cases of multiple narrowed coronary arteries. (Stergiopoulos K, et al.,2014 )
MANAGEMENT: [Ohman, EM. ,March 2016]
The treatment of chronic ischaemic heart disease has two major goals:
(i) to prevent myocardial infarction (MI) and death, thereby improving life expectancy.
(ii) to reduce symptoms of angina and the occurrence of ischaemia, which should improve quality of life.
Medical therapy with aggressive cardiovascular risk factor modification is the cornerstone of therapy for chronic ischaemic heart disease. This holds true for patients being treated either medically or with coronary revascularization. The treatment strategies for chronic stable angina is separated into two important divisions:
(1) anti-anginal therapy and
(2) education and risk factor modification.
Anti-anginal therapy
Conditions that exacerbate and provoke angina should be considered; these include medications such as vasodilators, excessive thyroid replacement therapy, and vasoconstrictors. Medical problems such as profound anaemia, uncontrolled hypertension, hyperthyroidism, and hypoxemia should also be considered. Primary cardiac disorders such as tachy-and brady-arrhythmias, valvular heart disease (especially aortic stenosis), and hypertrophic cardiomyopathy may also exacerbate angina pectoris and should be excluded. Careful attention to history, thorough physical examination, and selection of appropriate laboratory and other diagnostic studies can help identify these clinical conditions.
β-blockers
β-blockers decrease heart rate, contractility and arterial pressure, resulting in decreased myocardial oxygen demand. In patients with chronic stable exertional angina, β-blockers decrease heart rate and blood pressure during exercise, and the onset of angina (ischaemic threshold) is delayed or avoided. Various types of β- blockers are available for the treatment of hypertension and angina (Table 1). All β-blockers appear to be equally effective in reducing angina pectoris. In the treatment of stable angina, it is conventional to adjust the dose of these drugs to reduce the resting heart rate to 50-60 beats per minute.
Table 1: Properties of β-blockers in clinical use
|
Drugs |
Selectivity |
Partial agonist activity |
Usual dose for angina |
|---|---|---|---|
|
Propranolol |
None |
No |
20-80 mg bid |
|
Metoprolol |
β1 |
No |
50-200 mg bid |
|
Atenolol |
β1 |
No |
50-200 mg bid |
|
Nadolol |
None |
No |
40-80 mg qd |
|
Timolol |
None |
No |
10 mg bid |
|
Acebutolol |
β1 |
Yes |
200-600 mg bid |
|
Betaxolol |
β1 |
No |
10-20 mg qd |
|
Bisoprolol |
β1 |
No |
10 mg qd |
|
Esmolol (intravenous) |
β1 |
No |
50-300 mg/kg/min |
|
Labetalol* |
None |
No |
200-600 mg bid |
|
Carvedilol* |
None |
No |
12.5-50 mg bid |
* combined α- and β-blocker. bid- twice a day ; qd – every day; tid – three times a day
The absolute cardiac contraindications for the use of β-blockers are severe bradycardia, pre-existing high degree atrioventricular block, sick sinus syndrome, and severe decompensated left ventricular failure (β-blockers have now been shown to reduce total mortality in patients with compensated heart failure). β- blockers should also be avoided in patients with pure vasospastic angina (Prinzmetal angina) because these agents may induce coronary vasospasm from unopposed α-receptor activity. Asthma and bronchospastic disease, severe depression, and severe peripheral vascular disease are relative contraindications. Most diabetic patients tolerate β-blockers, although these agents should be used cautiously in patients who require insulin. In the absence of contraindications, β- blockers are preferred as initial therapy. The evidence for this approach is strongest in patients with a history of prior MI, for which this class of drugs has been shown to reduce mortality.
Calcium antagonists
Calcium antagonists effectively treat hypertension and angina pectoris. These agents are commonly divided into the dihydropyridine and nondihydropyridine classes (Table 2). Calcium antagonists decrease coronary vascular resistance and increase coronary blood flow. All of these agents cause dilatation of the epicardial coronary vessels and the microcirculation arteriolar resistance vessels. Dilatation of the epicardial coronary arteries is the principal mechanism that allows calcium antagonists to relieve vasospastic angina. Calcium antagonists also concurrently decrease myocardial oxygen demand, primarily by reduction of systemic vascular resistance and reduction in arterial pressure. In addition, certain calcium antagonists (verapamil and diltiazem) reduce myocardial oxygen demand by decreasing heart rate and contractility.
Table 2: Properties of calcium antagonists in clinical use
|
Drugs |
Usual dose |
Duration of action |
Side effects |
|---|---|---|---|
|
Dihydropyridines |
|||
|
Nifedipine |
Immediate release: 30-90 mg daily orally Slow release: 30-180 mg orally |
Short |
Hypotension, dizziness, flushing, nausea, constipation, edema |
|
Amlodipine |
5-10 mg qd |
Long |
Headache, edema |
|
Felodipine |
5-10 mg qd |
Long |
Headache, edema |
|
Isradipine |
2.5-10 mg bid |
Medium |
Headache, fatigue |
|
Nicardipine |
20-40 mg tid |
Short |
Headache, dizziness, flushing, edema |
|
Non-dihydropyridines |
|||
|
Bepridil |
200-400 mg qd |
Long |
Arrhythmias, dizziness, nausea |
|
Diltiazem |
Immediate release: 30-80 mg 4 times daily |
Short |
Hypotension, dizziness, flushing, bradycardia, edema |
|
Slow release: 120-320 mg qd |
Long |
||
|
Verapamil |
Immediate release: 80-160 mg tid Slow release: 120-480 mg qd |
Short Long |
Hypotension, myocardial depression, heart failure, edema, |
bid – twice a day; qd – every day; tid - three times a day
Short-acting dihydropyridine calcium antagonists have the potential to enhance the risk of adverse cardiac events and should be avoided. Long-acting calcium antagonists of the dihydro-and nondihydropyridine class relieve angina and are appropriate initial therapy in patients with contraindications to β-blockers. They can also be substituted for β-blockers in patients who develop unacceptable side effects or can be used in combination with β-blockers when initial β-blockers therapy is unsuccessful.
Nitrates
Nitrates dilate epicardial coronary arteries and arterioles and reduce cardiac preload. They also relieve coronary spasm and dynamic stenoses, especially at epicardial sites. Their use is associated with reflex tachycardia, an effect that may increase myocardial oxygen demand. This response may be blunted by the concomitant administration of β-blockers or calcium antagonists, such as diltiazem or verapamil, which slow conduction.
Nitrates are available in multiple preparations exhibiting wide duration in clinical effect (Table 3). Short-acting nitrates, which are most often administered as sublingual tablets or buccal mucosal spray, are commonly used to treat acute episodes of angina. Unless contraindications exist, all patients with chronic stable angina should be given a short-acting nitrate and should be properly instucted in its use. The efficacy and action of long-acting nitrates depend on the dosing, bioavailability, and half-life of the various preparations. The most important aspect of long-term nitrate therapy is to ensure an adequate nitrate-free interval (typically night time), which will prevent nitrate tolerance.
Table 3: Properties of nitrates in clinical use
|
Compound |
Route |
Dose |
Duration of effect |
|---|---|---|---|
|
Nitroglycerin
|
Sublingual tablets |
0.3-0.6 mg up to 1.5 mg |
Short 2-3 minutes |
|
Spray |
0.4 mg as needed |
Short 2-3 minutes |
|
|
Ointment |
2% 6 X 6 in., 15 X 15 cm 7.5-40 mg |
Effect up to 7 h |
|
|
Transdermal |
0.2—0.8 mg/h every 12 h |
8-12 h during intermittent therapy |
|
|
Oral sustained release |
2.5-13 mg |
4-8 h |
|
|
Buccal |
1-3 mg 3 times daily |
3-5 h |
|
|
Intravenous |
5-200 μg/min. |
Tolerance in 7-8 h |
|
|
Isosorbide dinitrate
|
Sublingual |
2.5-15 mg |
Up to 60 min. |
|
Oral |
5-80 mg, 2-3 times daily |
Up to 8h |
|
|
Spray |
1.25 mg on tongue as needed |
2-3 min. |
|
|
Chewable |
5 mg |
2-2.5 h |
|
|
Oral slow release |
40 mg 1-2 times daily |
Up to 8 h |
|
|
Intravenous |
1.25-5.0 mg/h |
Tolerance in 7-8 h |
|
|
Ointment |
100 mg/24 h |
Not effective |
|
|
Isosorbide-5- mononitrate
|
Oral
|
20 mg twice daily / 60-240 mg once daily |
12-24 h
|
In patients with exertional stable angina, nitrates improve exercise tolerance, increase the time to onset of angina, and decrease ST-segment depression during treadmill exercise testing. Combined with β-blockers or calcium antagonists, nitrates produce greater anti-anginal and anti-ischaemic effects in patients with stable angina.
Revascularization
CABG versus medical therapy
Evidence from randomized clinical trials has demonstrated that coronary artery bypass grafts (CABG) improves mortality when compared to medical therapy for patients with significant left main disease, three vessel disease with left ventricular ejection fraction (LVEF) of less than 50%, or multi-vessel disease with involvement of the proximal left anterior descending artery (LAD). Although these trials were performed in an era prior to the availability of percutaneous coronary intervention (PCI) and the routine use of aspirin, β-blockers, and lipid lowering therapy, these surgical indications remain currently valid.
CABG versus PCI
PCI may be considered in patients with multi-vessel CAD (including the proximal LAD), who have anatomy suitable for catheter-based technique, do not have diabetes, and have normal left ventricular function. CABG or PCI may be considered in appropriate patients with single or multi-vessel CAD who have not been treated successfully by medical therapy and can undergo revascularization with acceptable risk.
PCI versus medical therapy (Nitroglycerin Sublingual ,.2017)
Many trials illustrate that low-risk patients with chronic stable angina pectoris and normal left ventricular function can be treated safely with medical therapy. Because of the risk of procedure-related complications, clinicians must carefully balance this excess hazard with the need for greater symptomatic improvement when selecting patients for PCI.
Antiplatelet agents
Aspirin (75-150 mg) exerts its antithrombotic effect by inhibiting cyclo-oxygenase and synthesis of platelet thromboxane A2. It is effective in preventing first heart attacks, improving mortality in acute coronary syndromes, and reducing adverse cardiovascular events in patients with stable angina pectoris. Aspirin should therefore be considered as first line therapy in all patients with chronic ischaemic heart disease. In patients with absolute aspirin contraindications alternative antiplatelet regimes such as dipyridamole (Persantine), ticlopidine (Ticlid), glycoprotein 11b/111a receptor antagonists may be considered, although the clinical data supporting their use in angina pectoris is less established.
Lipid lowering therapy
Of the classes of antihyperlipidemic drugs, the hydroxy-methylglutanyl coenzyme A reductase inhibitors or statins are the most potent agents available in lowering total and low density lipoprotein (LDL) and atherogenic cholesterol and are the only lipid-lowering agents shown to improve overall mortality in clinical trials. Furthermore, statins also exhibit anti-inflammatory properties, which may positively modify the artherosclerotic process.
Therefore, statins should be considered in all patients with established CAD and LDL cholesterol ≥ 130 mg/dL, targeting the on-therapy LDL cholesterol to less than 100 mg/dL. In general, modification of diet and exercise are less effective than statins in achieving the target levels of LDL cholesterol; thus, lipid lowering pharmacotherapy is usually required in patients with angina and should be considered as first-line therapy in disease modification.
A high density lipoprotein (HDL), antiatherogenic cholesterol level of less than 35 mg/dL is an independent risk factor for adverse cardiovascular events. Hygienic measures such as weight loss, exercise, alcohol consumption, diabetes control, and smoking cessation may provide modest increases in HDL cholesterol. Recently, a randomized trial comparing the fibrate gemfibrozil to placebo demonstrated reduced cardiovascular mortality in patients with CAD and an isolated HDL cholesterol of less than 35 mg/dL.
Education and Risk Factor Reduction (Walker C, et al.,2009)
Identification and treatment of coronary disease risk factors in patients with angina is necessary for optimal secondary prevention of chronic ischaemic heart disease. Established and modifiable coronary disease risk factors, such as cigarette smoking, hypertension, diabetes mellitus, and hyperlipidemia, are common in patients with chronic ischaemic heart disease. These risk factors are readily amenable to modification, and their treatment can affect clinical outcome favourably.
Studies show that the risk of death from CAD is inversely proportional to education. It is therefore important for the physician to assess the patient’s baseline understanding of his or her condition and to appropriately educate the patient and his or her family on the pathology and pathophysiology of the disease, prognosis of condition, and treatment and risk factor reduction options.
Obesity
Obesity is a common condition associated with an increased risk for coronary artery disease and mortality. Obesity is also associated with and contributes to other coronary risk factors, including high blood pressure, glucose intolerance, low levels of HDL cholesterol, and elevated triglycerides. Thus, much of the increased CAD risk associated with obesity is mediated by these factors. Weight reduction in obese patients with coronary disease can likely reduce the risk of future events because weight reduction will reduce other modifiable risk factors and reduce the increased myocardial oxygen demand imposed by obesity. Weight reduction is therefore recommended in all obese patients with ischaemic heart disease. Strategies to improve weight reduction include:
a. lowering total caloric intake,
b. eating foods low in cholesterol and saturated fat and high in fibre and unsaturated fat, and
c. exercise training.
Exercise
Exercise training improves blood pressure, glucose control, lipid profile, exercise endurance, and objective measures of ischaemia. In addition, exercise training may lead to changes in weight and a sense of well-being. For these reasons, a regular exercise program should be part of a multifactorial intervention program in patients with stable chronic ischaemic heart disease.
FOLLOW-UP
Patients who are successfully treated for chronic ischaemic heart disease should have follow-up evaluation every 4 to 12 months. A more precise interval cannot be recommended because many factors influence the length of follow-up period. Five questions must be answered regularly during the follow-up evaluation:
(1) Has the patient decreased the level of physical activity?
(2) Have the patient’s anginal symptoms increased in frequency and become more severe since the last visit?
(3) How well is the patient tolerating therapy?
(4) How successful has the patient been in reducing modifiable risk factors and improving knowledge about ischaemic heart disease?
(5) Has the patient developed any new comorbid illnesses or has the severity or treatment of known comorbid illnesses worsened the patient’s angina?
Patients who cannot reliably identify and report changes in their status or who need more support with their treatment or risk factor reduction should be seen more frequently.
CONCLUSION:
The increase globalization and modernization in life style of people has attributed many diseases. According to an survey of an death rate the “1” in every “4” death is among from an Ischemic heart diseases. Ischemic heart diseases are one of the most threatening problem faced by the people. The group of patients who are suffering from coronary arteries diseases are very likely to be more prone to have developed with hypertension, life style and not proper Diet. A ischemic heart disease is cure fast when we do proper diagnosis and take an suitable drug. Ischemic heart disease is cure when an patient change the lifestyle. And also is cure by taking proper diet and doing regular exercise , an avoiding the alcohol and smoking and taking suitable drug. If any symptoms acquire regarding coronary heart disease, it should fast consult doctor and diagnosis. By using these proper medicine and obey an prevention, we can reduce the sudden ischemic heart disease death and save the patient’s health & life.
REFERENCES:
1. "Coronary heart disease". NIH . Archived from the original on 12 September 2013. Retrieved 15 September 2013
2. "Nitroglycerin Sublingual: MedlinePlus Drug Information". medlineplus.gov. Archived from the original on 6 January 2017
3. "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009
4. Ambrose, John; Singh, Manmeet (2015). "Path physiology of coronary artery disease leading to acute coronary syndromes".
5. American College of Cardiology (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Cardiology, archived from the original on 17 December 2013, retrieved 10 February 2014
6. Erling Falk,Prediamn K. shah, Pim J. Feyter. Ischemic heart disease 1th edition. Burden on ischemic heart diseases. Page no-15 -18
7. Erling Falk,Prediamn K. shah, Pim J. Feyter. Ischemic heart disease 1th edition. Anatomy of Heart. Page no: 20 to 23
8. Hackshaw, Allan; Morris, Joan K; Boniface, Sadie; Tang, Jin-Ling; Milenkovic, Dusan (24 January 2018). "Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study report.
9. Kerola, AM; Kauppi, MJ; Kerola, T; Nieminen, TV (October 2012). "How early in the course of rheumatoid arthritis does the excess cardiovascular risk appear?". Annals of the rheumatic diseases. 71 (10): 1606–15.
10. Kharade S.M, Rajmane M.A, Samudre P.A, Patil S.S. A Review: Etiology and Path physiology of Congestive Heart Failure. International Journal of Pharmaceutical and Phytopharmacological Research, 2014; 3(5): 352-356.
11. Kontos, MC; Diercks, DB; Kirk, JD (Mar 2010). "Emergency department and office-based evaluation of patients with chest pain". Mayo Clinic Proceedings. 85 (3): 284–99.
12. Kwak SM, Myung SK, Lee YJ, Seo HG (2012-04-09). "Efficacy of Omega-3 Fatty Acid Supplements (Eicosapentaenoic Acid and Docosahexaenoic Acid) in the Secondary Prevention of Cardiovascular Disease: A Meta-analysis of Randomized, Double-blind, Placebo-Controlled Trials". Archives of Internal Medicine. 172 (9): 686–94.
13. Mendis, Shanthi Puska, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18.
14. Ohman, EM (March 2016). "CLINICAL PRACTICE. Chronic Stable Angina". New England Journal of Medicine. 374 (12): 1167–76.
15. Schocken DD, Ischemic heart diseases: A scientific statement from the American Heart Association. Circulation. 2015.
16. Stergiopoulos K, Boden WE, Hartigan P, Mobius-Winkler S, Hambrecht R, Hueb W, Hardison RM, Abbott JD, Brown DL (2014). "Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials". JAMA Intern Med. 174 (2): 232–40.
17. Walker C, Reamy BV (April 2009). "Diets for cardiovascular disease prevention: what is the evidence?". Am Fam Physician. 79 (7): 571–8.
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 6, Issue 5 Received On: 02/03/2018; Accepted On: 02/04/2018; Published On: 01/05/2018 How to cite this article: Dhankwala SS, Gavsane AN, Ghuli PM, Jadhav SA; Review on Ischemic Heart Diseases and Its Medication; PharmaTutor; 2018; 6(5); 23-31; http://dx.doi.org/10.29161/PT.v6.i5.2018.23 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









