{ DOWNLOAD AS PDF }
ABOUT AUTHOR
AK Mohiuddin
Department of Pharmacy, World University of Bangladesh,
Dhanmondi, Dhaka, Bangladesh
ABSTRACT
In the business world, customer relationship management is utilized to hold customer reliability so as to expand income. Healthcare associations can fabricate a similar sort of relationship with patients, and it can likewise offer progressively unmistakable advantages. The principal advantage is by utilizing a similar hospital a patient's treatment history ought to be moderately outstanding by the association. Intermittently, extraordinary hospitals utilize distinctive patient data frameworks which are not constantly perfect with one another. On the off chance that a patient continues changing the hospital, his or her medical record can be dissipated around different destinations. In a perfect world, if the patient is treated by a similar doctor in each visit, that doctor will get progressively comfortable with the patient, which could enhance treatment. The most unmistakable advantage, be that as it may, is time. In the event that the patient goes to a similar doctor inevitably, there is no requirement for long registration toward the start of each visit. In spite of the fact that a developing collection of proof backings the utilization of cell phone short message service (SMS) for increasing physical movement, sustenance, and smoking suspension, past investigations were constrained by an attention on center to upper pay populaces, and have not focused on transcendently country networks outside the healthcare conveyance framework. Hospital websites are considered as a fitting framework for trading data and building up correspondence between patients, hospitals, and medical staff. Website character, website contact intelligence, shopping accommodation, just as consideration and service are the variables to the extent the patient relationship management is concerned. In healthcare situations, patients are considered as the primary customers; in this way, the term Patient Relationship Management (PRM) is utilized in these unique situations. PRM permits healthcare focuses to have a superior understanding into the requirements of patients while giving them better consideration. Thusly, PRM gives a chance to utilize information and data to comprehend customers and to make an incentive with them. The requirement for PRM developed when associations comprehended that it was less exorbitant to keep their present customers, while pulling in another customer would be more-expensive for an association than keeping their present customers.
Reference Id: PHARMATUTOR-ART-2656
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 7, Issue 04 Received On: 11/02/2019; Accepted On: 05/03/2019; Published On: 01/04/2019 How to cite this article: Mohiuddin, A. 2019. Patient Relationship Management : Patient Care with CRM Approach. PharmaTutor. 7, 4 (Apr. 2019), 22-36. DOI:https://doi.org/10.29161/PT.v7.i4.2019.22. |

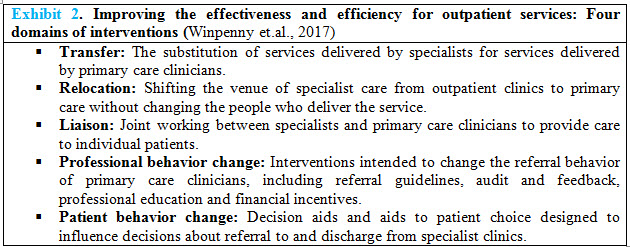
Figure 1. Customer Relationship Management Solutions for Patient Care (Source: Enterprise IT Solutions - Qatar HQ) Patient Relationship Management or Customer Relationship Management for healthcare is a system design strategy said to have the potential to increase patient satisfaction and reduce healthcare costs. By storing all of this information, health care providers will be able to send e-information to patients about newly published health care studies that may be relevant to the patient, or offer specialized suggestions that fit the patient profile. Also, a PRM in healthcare can help promote disease education, prevention, and wellness services. This information could also be used to automate those call center operations, in which routine advice for certain aspects of care can be made available at the call center without having to distract nurses or physicians from their primary care duties (Vardasca et.al., 2011).
INTRODUCTION
A PRM application likewise can give better mind to patients by permitting hospitals a superior comprehension of patients' needs and need through enhanced correspondence by means of follow-up frameworks. Seeing how the treatment has functioned is urgent for doctors. By telling the doctors, how fulfilled the patients are, doctors can have a superior comprehension on how the medications and tasks they perform are working. Along these lines, having better patient relationships and better patient steadfastness benefits both the healthcare association and the patient. Today, patients can without much of a stretch discover guidelines for their treatment from the Web. At the point when hospitals give constant data and disperse it to their present and potential patients it will assist them with staying in contact with individuals just as rival other healthcare associations for customers. Hospital management procedures should think about far reaching, productive hospital data frameworks which bolster a move of center to patients. With the possibility of PRM, hospitals might almost certainly proceed onward towards more customer-driven tasks than previously. PRM permits healthcare focuses to have a superior knowledge into the necessities of patients while giving them better consideration. In healthcare and treatment associations, PRM centers around such needs as deciding the patients' meetings with doctors and the historical backdrop of the patients' medicines. In the event that a patient is analyzed by a solitary doctor each time he/she visits the inside, as a result of the doctor's nature with the patient, not exclusively will the treatment procedure enhance, yet in addition the patient's time just as the doctor's time will be spared. All in all, this framework underpins issues identifying with the patient, data on the treatment, mindfulness, and the patient's consideration procedure. Nowadays, hospitals broadly utilize the Internet to give their services. Patients can without much of a stretch discover guidelines for their treatment by means of websites. At the point when hospitals give genuine data on the treatment of their patients through their websites, they won't just collaborate with patients yet additionally assist make a focused domain with different hospitals with regards to pulling in patients. Discoveries of various examinations have shown that the websites of a few instructive hospitals are normal regarding structure (fundamental page, principle connections and sub-joins), and extremely poor as far as substance and sub-joins (Theme-based substance), requiring adjustment, fruition and development. Websites have been intended to address data issues and offer vital assets. Accordingly, the structure of websites ought to be founded on the present needs of the clients and should be sufficiently adaptable to meet their future needs so it can upgrade their dimension of fulfillment with the association and bit by bit increment the association's profitability over the long run.
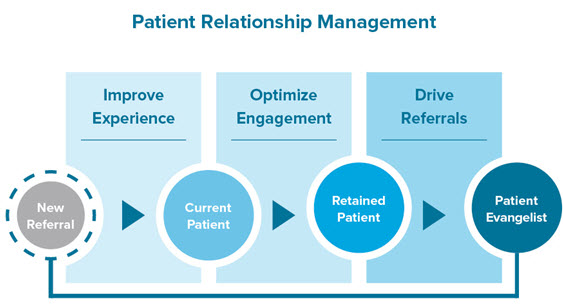
Figure 2. Patient loyalty program 200. To improve clinical outcomes, increase patient satisfaction and incur profit revenue, engaging patients in their own healthcare is critical. The US government is encouraging the use of Electronic Health Records (EHRs) via HealthIT.gov and promoting incentives to doctors who use EHRs meaningfully to reduce medical errors and improve the quality of care. CROs and independent service providers are designing educative websites that can be accessed via mobiles or the internet for educating patients on diseases. A few examples of available websites and tools are (1) Agency for Health Research and Quality maintained by US Department of Health and Human Services (2) ClinicalResearch.com (3) WELVU – Mobile First, an iPad- and iPhone-based educative tool providing medical illustration, quality scores, and health outcomes to engage patients (4) Krames patient education from StayWell (5) ExitCare OnScreen™ video solutions for patient education. The retention of patients in a trial is the key to the success of the overall project. Acurian, a service provider for recruitment and retention services uses platforms such as Facebook and Myspace for patient referrals and retention strategies. The easier it is to be compliant to study schedule, the better is the retention till the end. Dose compliance tracking tools like MediGuard™ enable reminders to be set up for dose intake (Source: Sharma, 2015)
Key Elements of PRM For Hospitals
• Collection of data related to personal details of the patients, frequency of visits of the patients, the doctor he is referring to, admission of patients, medical history, discharges, attendants, details of physicians etc. from across the enterprise, recording it and maintaining a database or the Master File.
• Analyzing the data and identifying the potential profitable customers, formulating the best marketing opportunities for them and finding the best medium to communicate with the identified targets.
• Developing marketing campaigns for turning the likely to be customers into profitable customers.
• Tracking the effectiveness and return on investment from these campaigns (Rafique et.al., 2016)
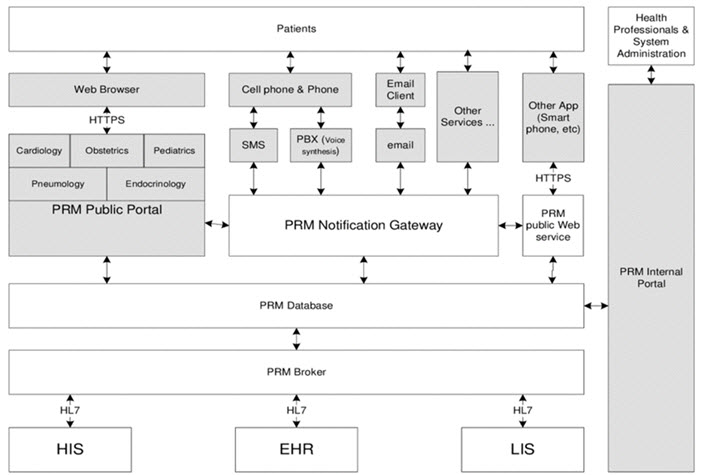
Figure 3. Patient relationship management system architecture. To support compliance with the HIPAA, organizations are increasing standard data communication with payers. In addition, integration with other healthcare organizations is frequently required to support clinical workflow and HIN participation. An organization may integrate external services into its SOA solution to provide complete process interoperability. For example, when a patient is registered within an organization, the service may use an external service provided by the HIN to register the patient for the entire community of care. Not only is the patient’s registration information synchronized, but this external communication is placed into the related workflow with little user impact, creating interoperability outside organization system boundaries (Hussain et.al., 2012).
Application of PRM
PRM is not a technology but rather a vision realized through technology; technology grants the ability to achieve more cohesion between the disparate parts of the healthcare system, which in turn improves both clinical outcomes and patient satisfaction". PRM can
• Help prevent additional illness. With a 360-degree view of the patient, physicians can more easily identify relationships between current symptoms and future health concerns.
• Improve the quality and consistency of care. Automated processes can be created to ensure critical safety procedures are followed, and that the organization is in compliance with privacy and other regulatory policies.
• Speed routine processes, such as admissions, referrals, and discharges. By analyzing the performance of routine processes over time, improvements can be made that eliminate unnecessary steps and increase patient satisfaction.
• Eliminate time wasted accessing information. By electronically storing indexed documents, such as treatment plans, symptom-and-diagnoses relationships, and reference articles, less time is spent searching for information needed to deliver quality care.
• Automate proactive communications. By viewing patient data sorted by certain characteristics, targeted proactive communications can easily be sent. For example, mailings to diabetic patients can inform them of new information, treatment options, or upcoming educational offerings.
• Reduce the number of missed appointments. Tasks can easily be set up to streamline appointment reminder calls. Automated processes can be put in place for follow-up and rescheduling should appointments be missed (Hajikhani et.al., 2015).
Benefits of PRM in the Health Care Industry
• Patient PRM applications can speed routine processes, such as admissions, referrals, and discharges by analyzing the performance of routine processes over time. Improvements can be made to eliminate unnecessary steps and increase patient satisfaction.
• Furthermore, it can help prevent additional illness by physicians taking thorough examination of the patients all times to enable them easily identify relationships between current symptoms and future health concerns.
• Moreover, PRM application can eliminate time wasted accessing information by electronically storing indexed documents, such as treatment plans, symptom-and diagnoses relationships, and reference articles, less time is spent searching for information needed to deliver quality care.
• The PRM can automate proactive communications by viewing patient data sorted by certain characteristics, targeted proactive communications that can easily be sent. For example, mailings to diabetic patients can inform them of new information, treatment options, or upcoming educational offerings.
• PRM can also contribute to improve the quality and consistency of care by creating automated processes to ensure critical safety procedures are followed, and that the organization complies with privacy and other regulatory policies.
• Finally, yet importantly is that PRM will reduce the number of missed appointments. Tasks can easily be set up to streamline appointment reminder calls. By putting automated processes in place for follow-up and rescheduling should appointments be missed (Paazine et.al., 2011).
PRM versus CRM in Private and Public Health Care
In brief, while CRM and PRM involve similar approaches, "the goal of CRM is ultimately to increase consumer spending. Conversely, PRM strives to give patients the information they need to make better healthcare choices, which will ultimately save them and the system money". PRM also requires added consideration for handling complex data and the need to enforce airtight security and the appropriate use of patient data. Despite the differences, commonalities between CRM and PRM enable stronger relationships that benefit from: greater anticipation of customer needs and wants, improved communication channels, timely and credible information, and the capture of tacit knowledge in essence knowing people better without wasting their time. However, the marketing tactics of commercial persuasion and manufactured demand do not directly apply in healthcare; therefore, the best ‘marketing’ goal that a private for-profit healthcare organization can hope for in "the migration of CRM to PRM is the natural evolution of building the perception. When the need arises, the promoted physician practice or hospital is there to help you." Nevertheless, ‘perception management’ also applies to public PRM in efforts to nurture relationships with a patient/provider audience receptive to preventive, cost-saving interventions that stave off the need for expensive acute care services. Responsibility for the public purse creates an impetus for seeking these efficiencies through this form of Citizen Relationship Management—the CRM equivalent in the public realm (Vardasca et.al., 2011; Oinas-Kukkonen et.al., 2008)
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
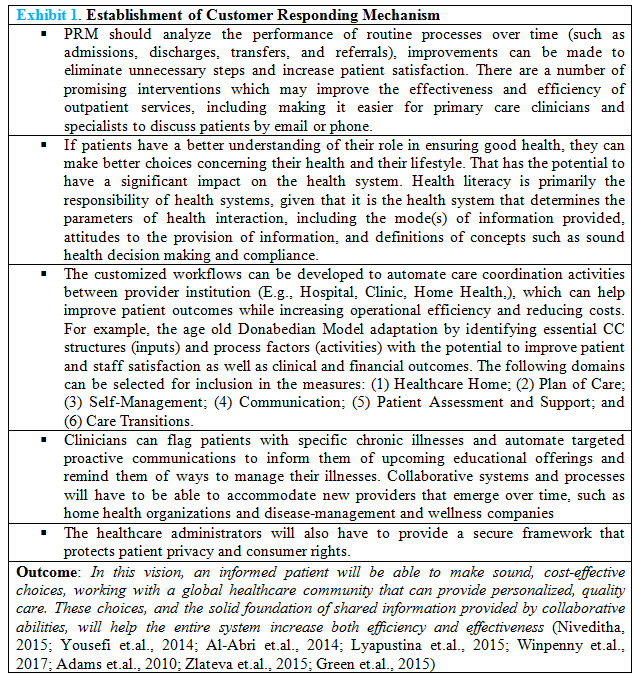
Implementation of CRM in Health Care
CRM system needs a daily accumulation of data from both in-patient and outpatient departments’ terminals through multi-media platform and integration with other ancillary technical systems enable an effective CRM system to be completed after the following work is done well.
• Integration of CRM system with HIS
• Integration of CRM with Hospital Web Platform
• Integration of CRM with Call Centers
• Integration of CRM with short-message gateway
• Establishment of Customer Responding Mechanism and Database (Anshari et.al., 2011, Poku et.al., 2016)
PRM Programs in Hospital Setting
A Customer Relationship Program for patients in a hospital can be broadly classified into two factions i.e. In Patient CRM and Out Patient CRM. In Patient CRM includes all those customer care activities when a person gets treatment in the hospital and avail the facilities rendered by the hospitals. Here the customers can be the patient and the attendants to the patient i.e. who accompanies or visit the admitted patients. Out Patient CRM consists of those customer care activities when the person is discharged from the hospital. It includes maintenance of database of each and every patient and thereafter, maintaining regular interaction with the patient.
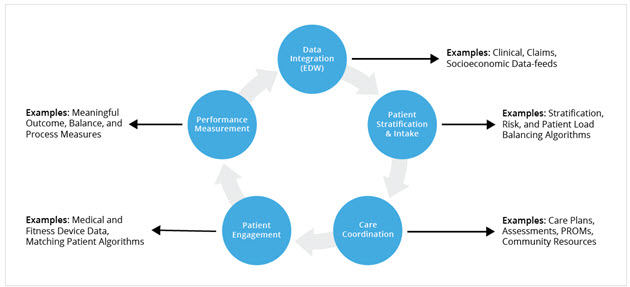
Figure 4. Components of a well-organized care management program.
Many healthcare organizations have leveraged information from their Health Catalyst Analytics Platform, including their Late-Binding™ Data Warehouse (EDW) and broad suite of analytics applications, to support the identification of specific patient cohorts to monitor the impact of care management interventions on individual and population health outcomes. The programs featured below focus on different patient populations, but they share major commonalities. The themes of aggregating data to identify and risk stratify potential patients, focusing on care coordination functions, developing processes to improve patient engagement, and importantly, measuring performance, are prevalent throughout the examples. The care managers assess patient risks and needs, including comprehensive functional assessments and potential barriers to care. They closely monitor patients during office appointments; looking for gaps in understanding or the ability to comply with the established medical treatment plans; use phone calls and home visits to monitor patients after visits; and coordinate services such as diagnostic tests, transportation, social services, and specialist services. Care managers also serve as liaisons between the patient and other members of the care team across all settings. Leaders at Partners use data from the EDW to calculate the return on investment (ROI) for the iCMP, and to compare the iCMP patient outcomes to non-iCMP patients (Source: Chaguturu, 2016).
In Patient CRM: The most important parameter for a person visiting any hospital is the way of treatment he will get there. Winning over patient’s faith is of utmost importance for the employees of the hospital. Presence of a clean environment and suitable hoteling and space in the hospital cannot attract the patient's trust and in fact hospital must show its ability to meet the patient's needs practically in terms of the manner of service delivery and the personnel-patient interaction. Right from the chief doctor to the ward boy, it is the duty of each and every employee to ensure patient satisfaction and proper training can be given in this regard. They should make the patient believe that the hospital is doing their level best to cure him. Clear instructions about the procedures should be given to the patients and their attendants to eliminate unnecessary steps and avoid hassles. If the private hospitals aim to enhance the patients' trust, the quality improvement efforts must focus on the managerial aspects of service delivery, such as scheduling, timely and careful doing of the services, and strengthening the interpersonal relationships as well as the communication skills of the physicians, nurses and other personnel.
Out Patient CRM: Out Patient CRM includes post discharge activities which help in maintaining and strengthening the relationship with the patients. Hospitals should record and maintain computerized database of each and every patient in detail which includes personal details of the patient, medical history, referred physicians, scheduled appointments, frequency of visits etc. This information would in turn help in other CRM activities of the post discharge period. Even after getting discharged from the hospital, the patient needs to come again for further treatment or check up at regular intervals. These activities might include:
• Sending greetings and wishes on birthdays to the patients along with the offer of free health check-up. This would make the patient feel special and make him believe that the hospital still cares for him even after discharge.
• Maintaining a database would enable the hospital to send continuous reminder to the patients about the scheduled appointment and seek their confirmation that they would be coming.
• The hospitals can create “Rehabilitation Centers” for the patients who are suffering from long ailments. Once they are discharged from the hospital, the hospitals can arrange a visit to these centers for them where they can meet the people who are suffering from similar ailment or have already been treated for the same. This would give moral support to the patients and would curb the sense of insecurity and loneliness in them.
• The database helps the hospitals to get the proper understanding about the profile of patients who are visiting the hospital. It helps to list out the kind of disease from which most patients suffer from, their referral sources, the geographical areas from which the patients come from etc. Creating customer delight is crucial for any organization. Similarly, hospitals must also strive hard to achieve customer lifetime value by improving customer loyalty. CRM is not only confined to maintenance of database of every patient but it also about the use of technology to provide value added services to its customers. Apart from patients and attendants, now the hospitals are also driving their attention towards the customers i.e. the ones who are presently healthy and are availing the offers given by hospitals in terms of health packages and insurance schemes etc (Rafique et.al., 2016; Paazine et.al., 2011; Walker et.al., 2013; Posner et.al., 2017; Freytag et.al., 2017; Khoshraftar et.al., 2011; Zarei et.al., 2015)
PRM and Industrial Age Medicine
Patients who are more engaged with their care have better outcomes, and leading healthcare organizations are actively seeking to develop strategic approaches to promote this process. Many profit hunting HCEs are striving to improve patient satisfaction. Focus on patient satisfaction alone can actually be undesirable in terms of achieving cost-effective, high-quality care. For example, physicians have been known to inappropriately prescribe opioid pain drugs and antibiotics in order to protect patient satisfaction scores. To thrive in a value-driven reimbursement environment, providers will need to adopt a sincere orientation towards patients and families in order to achieve significant activation and engagement. This process can result in stronger therapeutic alliances between providers and patients, improved patient decision-making, and better health outcomes. Stronger relationships between providers and patients can increase value, but these relationships cannot be forged by initiatives that focus merely on satisfaction. Just as companies outside the healthcare sector have developed systems, tools, and processes around CRM, healthcare organizations should build the same discipline around the concept of PRM (Poku et., al 2016; Khoshraftar et.al., 2011; Yaghoubi et.al., 2017; Elangchezhian et.al., 2014; Dash et.al., 2011; Asgar et.al., 2015; Lyapustina et.al., 2015; Zgierska et.al, 2012; Business Roundtable, 2014; Primary Care Collaborative, 2010; Zgierska et.al, 2014)

Figure 5. Tools for Providing Excellent Communication in a Healthcare Setting.
The AWARE pneumonic is a great way to improve communication in the healthcare environment. Communication with sending and receiving facilities, dispatch, and even with those on scene calls will only help increase the continuity of care. Patients and carers place high value on face-to-face communication with health-care professionals, who can engage on an emotional level, listening and assessing patients’ information needs and providing information with clarity and sympathy. This is especially relevant when dealing with patients with a cancer diagnosis, who may be facing difficult or complex decisions about treatment options. Specific communication needs at different stages must also be considered—diagnosis, treatment, recurrence, palliative and terminal care. It is suggested that good communication is a pre-requisite for enabling patients and carers to make informed decision about care (Source: Liptrott et.al., 2009)
Prompt Attention and Ensuring Hassle Free Service
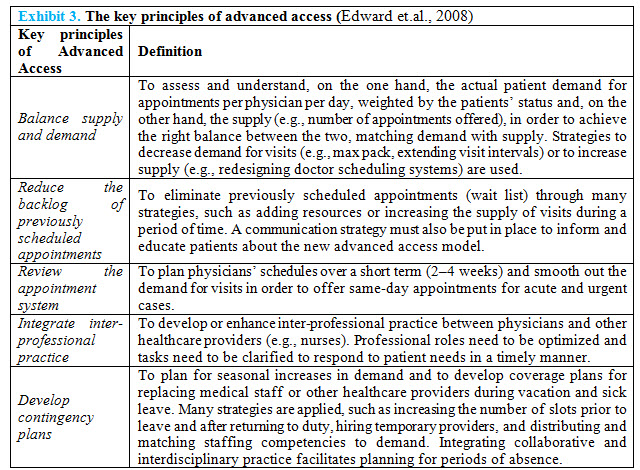
There is much that a concerted effort around PRM can address. Most importantly, delayed access to health care is assumed to negatively affect health outcomes due to delays in diagnosis and treatment. Patients still have to wait days together to see their physicians after scheduling an appointment. The actual doctor’s visit consumes an average of 2 h of a given patient’s time, the bulk of which entails travel and waiting, with precious little dedicated to face-time with providers. The Institute of Medicine recommends that at least 90% of patients should meet doctors within 30 minutes of their scheduled appointment times. A waiting time is not only a factor that affects patient satisfaction but also one of indexes to evaluate the quality of services rendered to outpatients. Healthcare providers do not routinely check in on patients after even major changes to treatment regimens to assess efficacy, adherence, and side effects. Moreover, there is still no national mandate for providers to include patients’ caregivers around transitions of care. Patients and families deserve better healthcare delivery systems than they are currently getting, and a focus on PRM is one mechanism for realizing this aim (Poku et.al., 2017; Abou-Malham et.al., 2018; Edward et.al., 2008; Thi-Thao-Nguyen et.al., 2018;
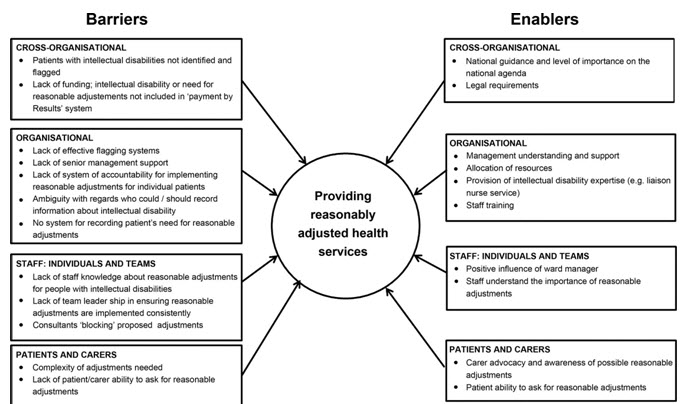
Figure 6. Empirical framework: barriers and enablers in relation to provide reasonably adjusted health services to patients.
The findings reported here have been derived from across data sets. An empirical framework representing the full list of barriers and enablers in relation to providing reasonably adjusted health services for patients with intellectual disabilities is given. The adjustments needed by different patients with intellectual disabilities varied greatly. This lack of homogeneity could make it difficult for healthcare staff to know how to adjust their care for an individual patient. For example, one patient with intellectual disabilities would benefit from an early morning appointment in an outpatient clinic, so that the waiting area was not yet too busy and waiting times were kept to a minimum; for another patient, however, such an early appointment was prohibitively difficult, as it took him several hours to get ready in the morning (Tuffrey-Wijne et.al., 2014).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
To ensure actual benefit of the patient
Patients often demand things they don’t need, like expensive antibiotics for a cold or an MRI for low back pain, and providers may be confronted with requests for items that they don’t know the value of, such as back stretchers for cervical radiculopathy. Physicians will need access to the best evidence on therapies and technologies, and must also become skilled at explaining to patients why they will not benefit from things that are unlikely to help them (Poku et.al., 2017). Clearly, this will be a delicate balance. Health care system is characterized by high and rising healthcare costs as well as gaps in quality, safety, equity, and access. With limited healthcare budgets, it is important that resources are used in a way that provides the most value for patients. US healthcare system faces daunting challenges in the years ahead. Increasing costs, limitations in access to care, and variability in the quality of care delivered threaten the long-term viability of the system. According to the MedPAC, Medicare enrollment is projected to increase by more than 50% over the next 15 years from 54 million beneficiaries today to more than 80 million in 2030 (Landers et.al., 2016). Among the oldest Americans, the Census predicts that the population age 85 and above will double by 2036 and triple by 2049. Benefits in healthcare include both the quality and patient experience associated with the provision of healthcare services. While value-based purchasing (VBP) can refer to a wide variety of payment strategies that link provider performance and reimbursement (Damberg et.al., 2014), this paper will focus on VBP programs where providers are paid fee-for-service with payment adjustments up or down based on value metrics, a structure also known as pay-for-performance. This trend has led to calls for multi-stakeholder collaboration to improve quality and reduce the cost of healthcare, and to increase transparency regarding the cost and quality of healthcare services (Mannion et.al., 2008). As a result, a number of payment and delivery reforms have recently emerged, which attempt to promote higher value healthcare (Chee et.al., 2016). Long-term success is predicated on the creation of patient-centric value creation (eg, higher quality, patient-centered care at a lower cost). The Institute of Medicine has emphasized value as an important part of improving health care systems, and the American College of Physicians has launched the High Value Care Initiative. It is an increasingly important concept in medicine and rehabilitation, home care, long term care, hospice and other similar HCEs. The value-based system refers to a personalized care, where patient’ expectations and needs are included in a holistic approach of medicine that considers physical, mental, and spiritual well-being (Mor et.al., 2005). Providers should also assess their risk tolerances and organizational cultures. At the micro level, the quality-cost relationship is focused on the impact of health care service delivery on individual patients, as well as on the decisions of individual providers and organizations that manage the care. At the macro level, this relationship is evaluated based on population impact and the costs to society to achieve a positive health status for large cohorts of people (Institute of Medicine US, 2002; Carvalho et.al., 2018). Achieving success in value-based payment and delivery requires an organizational culture that emphasizes and facilitates high-quality, safe, patient-centered, cost-effective care. It also requires strong physician leadership and a willingness to change often longstanding practice patterns and systems of care (Bozic, 2013). Finally, organizations should define in advance the metrics they will use to evaluate and monitor successes or failures. Thus, aligning PRM with an appropriate reimbursement model is essential—in a fee-for-service reimbursement environment, utilizing PRM to deliver an ever-growing set of unnecessary services would be a real risk (Skempes et.al., 2018). As emerging reimbursement schemes increasingly reward true healthcare value creation, provider organizations will find incorporating PRM to be a key element of a winning strategy.
CONCLUSION
Reflecting on the future state of our healthcare delivery system, it is important to note that high levels of satisfaction and high care quality do not always align. A national study demonstrated that higher patient satisfaction was correlated with higher total healthcare expenditure and increased mortality. Patients often demand things they don’t need, like expensive antibiotics for a cold or an MRI for low back pain, and providers may be confronted with requests for items that they don’t know the value of, such as back stretchers for cervical radiculopathy. Physicians will need access to the best evidence on therapies and technologies, and must also become skilled at explaining to patients why they will not benefit from things that are unlikely to help them. Clearly, this will be a delicate balance. Furthermore, while the takeaways described by the three companies are important lessons for healthcare leaders to internalize, they must do so in a measured way that acknowledges the inherent differences between operating a healthcare delivery enterprise and operating a service enterprise outside the healthcare domain. In the latter, the primary goal is to deliver service excellence in order to increase customers’ willingness to pay and/or to increase the rate of return customers. Healthcare, of course, is different. Maximizing value delivery in healthcare services will mean improving the health of patients in part by avoiding costly acute care services. It may also be hard for patients to fully judge the value of a healthcare service even after that service is provided. Thus, aligning PRM with an appropriate reimbursement model is essential—in a fee-for-service reimbursement environment, utilizing PRM to deliver an ever-growing set of unnecessary services would be a real risk. As emerging reimbursement schemes increasingly reward true healthcare value creation, provider organizations will find incorporating PRM to be a key element of a winning strategy.
REFERENCES
1. Abou-Malham S, Touati N, Maillet L, Breton M. (2018); The challenges of implementing advanced access for residents in family medicine in Quebec. Do promising strategies exist? ; Med Educ Online ;23(1); 1438719
2. Adams RJ. (2010); Improving health outcomes with better patient understanding and education; Risk Manag Healthc Policy; 3; 61-72
3. Asgar MG, Shahri S. (2015); Customer relationship management in healthcare; Umhuriyet University Faculty of Science Science Journal (CSJ), 36(3); 1003-1005
4. Anshari M, Almunawar MN.(2011); Evaluating CRM Implementation in Healthcare Organization; 2011 International Conference on Economics and Business Information IPEDR vol.9 (2011) IACSIT Press, Bangkok, Thailand.
5. Al-Abri R, Al-Balushi A. (2014); Patient satisfaction survey as a tool towards quality improvement; Oman Med J.; 29(1):3-7.
6. Business Roundtable(2014); Driving Innovation in the Health Care Marketplace A CEO Report. Available from: https://s3.amazonaws.com/brt.org/archive/0_healthcare/BRT-Health-Care.pdf
7. Bozic KJ. (2013); Improving value in healthcare. Clin Orthop Relat Res ;471(2); 368-70.
8. Bradley EH, Fennell ML, Pallas SW, Berman P, Shortell SM, Curry L. (2011); Health services research and global health; Health Serv Res; 46(6pt2); 2019-28.
9. Carvalho AS, Martins Pereira S, Jácomo A, Magalhães S, Araújo J, Hernández-Marrero P, Costa Gomes C, Schatman ME. (2018); Ethical decision making in pain management: a conceptual framework; J Pain Res; 15(11); 967-976
10. Chee TT, Ryan AM, Wasfy JH, Borden WB. (2016); Current State of Value-Based Purchasing Programs; Circulation ;133(22); 2197-205.
11. Chaguturu S. (2016); Care Management: A Critical Component of Effective Population Health Management; Web Health Catalyst; 1-8
12. Damberg CL, Sorbero ME, Lovejoy SL, Martsolf GR, Raaen L, Mandel D. (2014); Measuring Success in Health Care Value-Based Purchasing Programs: Findings from an Environmental Scan, Literature Review, and Expert Panel Discussions; Rand Health Q ;4(3):9
13. Dash SK, Panda AK (2011); Managing Customer Relationships In Private Health Care Facilities - A Study With Reference To Greater Noida City Of Uttar Pradesh; Serbian Journal of Management ; 6(1); 27 – 42
14. Edward GM, Das SF, Elkhuizen SG, Bakker PJM, Hontelez JAM, Hollmann MW, Preckel B, Lemaire LC; (2008); Simulation to analyse planning difficulties at the preoperative assessment clinic; British Journal of Anaesthesia; 100(2); 195–202
15. Elangchezhian K, Malmarugan D (2014); A Study on Customer Relationship Management Practices In Hospitals; Vellore Institute of Technology, Deemed University, Vellore. Available From: http://www.indianmba.com/Faculty_Column/FC14/fc14.html
16. Fraser I, Encinosa W, Glied S. (2008); Improving efficiency and value in health care: introduction; Health Serv Res ;43(5Pt2); 1781-6.
17. Freytag J, Stroben F, Hautz WE, Eisenmann D, Kämmer JE. (2017); Improving patient safety through better teamwork: how effective are different methods of simulation debriefing? Protocol for a pragmatic, prospective and randomised study. BMJ Open; 7(6):e015977.
18. Green BN, Johnson CD. (2015); Interprofessional collaboration in research, education, and clinical practice: working together for a better future; J Chiropr Educ; 29(1); 1-10.
19. Gentry S, Badrinath P. (2017); Defining Health in the Era of Value-based Care: Lessons from England of Relevance to Other Health Systems; Cureus; 9(3); e1079
20. Giuseppe Speziale (2015); Strategic management of a healthcare organization: engagement, behavioural indicators, and clinical performance; European Heart Journal Supplements; 17(Issue suppl_A, 1); A3–A7
21. Hajikhani S, Tabibi SJ, Riahi L. (2015); The Relationship Between the Customer Relationship Management and Patients' Loyalty to Hospitals; Glob J Health Sci. ;8(3);65-71.
22. Institute of Medicine (US) Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule; Nass SJ, Levit LA, Gostin LO, editors. Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research. Washington (DC): National Academies Press (US); 2009. 6, A New Framework for Protecting Privacy in Health Research. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9585/
23. Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century. Washington (DC): National Academies Press (US); 2002. 2, Understanding Population Health and Its Determinants. Available from: https://www.ncbi.nlm.nih.gov/books/NBK221225/
24. Jewell DV, Moore JD, Goldstein MS. (2013); Delivering the physical therapy value proposition: a call to action; Phys Ther; 93(1):104-14.
25. Khoshraftar A, Yazdi MFA. (2011); Improving The CRM System In Healthcare Organization. International Journal of Computer Engineering & Science; 1(2); 28-35.
26. Lyapustina T, Alexander GG. The prescription opioid addiction and abuse epidemic: how it happened and what we can do about it. The Pharmaceutical Journal (A Royal Pharmaceutical Society Publication) 11 June, 2015.
27. Liptrott S, Peccatori F, Cocquio A, Martinelli G. (2009); Communication skills and raising awareness in clinical practice: an Italian experience; Ecancermedicalscience; 3; 135.
28. Landers S, Madigan E, Leff B, Rosati RJ, McCann BA, Hornbake R, MacMillan R, Jones K, Bowles K, Dowding D, Lee T, Moorhead T, Rodriguez S, Breese E. (2016); The Future of Home Health Care: A Strategic Framework for Optimizing Value; Home Health Care Manag Pract; 28(4);262-278.
29. Marzorati C, Pravettoni G. (2017); Value as the key concept in the health care system: how it has influenced medical practice and clinical decision-making processes; J Multidiscip Healthc;10; 101-106.
30. Mor V. (2005); Improving the quality of long-term care with better information. Milbank Q; 83(3); 333-64.
31. Mannion R, Davies HT. (2008); Payment for performance in health care; BMJ; 336(7639):306-8.
32. Monem H, Hussin ARC, Sharifian R. (2012); Comprehensive Prioritized Perspectives of CRM System for Implementation in the Developing Countries’ Hospitals; International Journal of Computer Applications; 50(20):5-12
33. Niveditha MS(2015); Re -engineering The Outpatient Process Flow of a Multi - Specialty Hospital. Thesis submission for Master of Science in Health Administration; 1-162
34. Oinas-Kukkonen H, Räisänen T, Hummastenniemi N. (2008); Patient relationship management: an overview and study of a follow-up system; J Healthc Inf Manag; 22(3); 24-9
35. Poku MK, Behkami NA, Bates DW. (2014); Patient Relationship Management: What the U.S. Healthcare System Can Learn from Other Industries; J Gen Intern Med; 32(1); 101-104
36. Posner GD, Clark ML, Grant VJ. (2017); Simulation in the clinical setting: towards a standard lexicon; Adv Simul (Lond); 2; 15
37. Primary Care Collaborative (2010); Transforming Patient Engagement: Health IT in the Patient Centered Medical Home October 2010. Available from: https://www.integration.samhsa.gov/Health_IT_in_the_PCMH.pdf
38. Prentice JC, Pizer SD. (2007); Delayed access to health care and mortality. Health Serv Res; 42(2); 644-62.
39. Paazine V, Adjei M. (2011); Customer Relationship Management in the Health care Industry in Ghana;a Case Study in Ashanti Region and the Upper West Region; (Master Thesis) Iulea University of Technology, Sweden
40. Rafique N, Dadhichi A. (2016); Emerging Role of Customer Relationship Management in Global World with reference to Healthcare Services in Hospitals. IRACST- International Journal of Research in Management & Technology (IJRMT); 6(3);90-95
41. Rundell SD, Goode AP, Friedly JL, Jarvik JG, Sullivan SD, Bresnahan BW. (2015); Role of Health Services Research in Producing High-Value Rehabilitation Care. Phys Ther; 95(12); 1703-11.
42. Skempes D, Melvin J, von Groote P, Stucki G, Bickenbach J. (2018); Using concept mapping to develop a human rights based indicator framework to assess country efforts to strengthen rehabilitation provision and policy: the Rehabilitation System Diagnosis and Dialogue framework (RESYST); Global Health; 14(1); 96.
43. Sharma NS. (2015); Patient centric approach for clinical trials: Current trend and new opportunities. Perspect Clin Res; 6(3); 134-8.
44. Thi-Thao-Nguyen S, Yamamoto E, Thi Ngoc Nguyen M, Bao Le H, Kariya T, Saw YM, Duc Nguyen C, Hamajima N. (2018); Waiting time in the outpatient clinic at a national hospital in Vietnam; Nagoya J Med Sci; 80(2):227-239.
45. Tuffrey-Wijne I, Goulding L, Giatras N, Abraham E, Gillard S, White S, Edwards C, Hollins S. (2014); The barriers to and enablers of providing reasonably adjusted health services to people with intellectual disabilities in acute hospitals: evidence from a mixed-methods study; BMJ Open; 4(4);e004606
46. Vardasca TR, Martins HM. Patient Relationship Management in public healthcare settings System architecture. IEEE Communications Society subject matter experts for publication in the IEEE ICC 2011 proceedings. Conference Paper June 2011
47. Walker LE, Nestler DM, Laack TA, Clements CM, Erwin PJ, Scanlan-Hanson L, Bellolio MF. (2018); Clinical care review systems in healthcare: a systematic review; Int J Emerg Med; 11(1):6.
48. Winpenny EM, Miani C, Pitchforth E, King S, Roland M. (2017); Improving the effectiveness and efficiency of outpatient services: a scoping review of interventions at the primary-secondary care interface; J Health Serv Res Policy; 22(1);53-64
49. Yousefi K, Kargari M. (2014); Patient Relationship Management Method, an Approach toward Patient Satisfaction: A Case Study in a Public Hospital; International Journal of Travel Medicine and Global Health2(1); 11-17.
50. Yaghoubi M, Asgari H, Javadi M. (2017); The impact of the customer relationship management on organizational productivity, customer trust and satisfaction by using the structural equation model: A study in the Iranian hospitals; J Educ Health Promot; 6; 6.
51. Zgierska A, Miller M, Rabago D. (2012); Patient satisfaction, prescription drug abuse, and potential unintended consequences; JAMA; 307(13):1377-8.
52. Zgierska A, Rabago D, Miller MM. (2014); Impact of patient satisfaction ratings on physicians and clinical care; Patient Prefer Adherence; 8; 437-46.
53. Zlateva I, Anderson D, Coman E, Khatri K, Tian T, Fifield J. (2015); Development and validation of the Medical Home Care Coordination Survey for assessing care coordination in the primary care setting from the patient and provider perspectives; BMC Health Serv Res; 15; 226
54. Zarei E, Daneshkohan A, Khabiri R, Arab M. (2014); The Effect of Hospital Service Quality on Patient's Trust; Iran Red Crescent Med J; 17(1);e17505
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









