{ DOWNLOAD AS PDF }
ABOUT AUTHORS:
Alok Khunteta1,2, Vikas Pareek2*
1Registrar, Rajasthan Pharmacy Council,
2 Department of Pharmaceutics,
Lal Bahadur Shastri College of Pharmacy,
Rajasthan University of Health Sciences, Jaipur, Rajasthan
* Vikaspareek@yahoo.com
ABSTRACT:
Age-related cognitive decline is a well-known phenomenon, called by various means such as age-associated memory impairment and age associated cognitive impairment. Since cerebral aging is idiopathic, so due to lack of pure reasons it’s diagnosis is typical and also it’s not being recognized at early ages by person too. As per the reports by 2050, it is anticipated that Americans aged 65 or older will number nearly 89 million people, or more than double the number of older adults in the United States in 2010, these stats are complementary to global scenario. The review is to collectively cast Cerebral aging with reasons and solutions. The detail of theories regarding cerebral aging and its related deficits is provided. Pharmacological action of both Allopathic and Ayurvedic medicines are illustrated. The role of yoga and pranayam being a quencher of Reactive oxygen species (ROS) thus reducing cerebral aging is also provided further in review.
INTRODUCTION:
Cerebral aging or age related cognitive decline is a well known natural phenomena which was subsumed under a variety of terms, such as Age related memory impairment (whenever the decline is restricted to memory functions) and Age associated cognitive impairment (whenever the cognitive decline relates to memory and/or other cognitive functions).[1]
A neurological disorder is a disorder of the body's nervous system. Cerebral aging is well associated with major of neurological disorders and thus cerebral aging is the topic on which special emphasis is laid. Various neurological disorders are enlisted below,
(1) Aphasia (language disorder)
(2) Dysarthria(speech disorder)
(3) Apraxia(disorder in patterns or sequences of movements)
(4) Agnosia(difficulty in identifying things/peoples)
(5) Amnesia (memory disorder)
(6) Neuropathic pain
(7) Delirium and dementia
(8) Dizziness and Vertigo
(9) Stupor and Coma
(10) Multiple Sclerosis (MS) and other de-myelinating diseases.
(11)Complex regional pain syndrome (CRPS: A chronic pain condition)
(12) Epilepsy
(13) Parkinson’s Disease
(14) Alzheimer’s Disease.
Cerebral Aging is mostly related to the Geriatrics i.e. to the old people since aging get more profound in this quarter of life and can be easily recognized by cognitive disorders.[2]
Various organizations stated that individual over age 60 alternatively 65 is estimated by the World Health Organization to increase to above billion worldwide by the year 2020. Europe is expected to it’s percentage of aged residents from 20% to 25%. The population of Japan is expected to be over 30% aged. Projections for North America, East Asia, Latin America, and South Asia are 23%, 17%, 12%, & 10%, respectively. The most rapid increases are expected in developing countries. Causes of death in developing countries are expected to be largely age related by 2020. In addition, the number of individuals overage 85 will rise dramatically. The US Government expects these “oldest of old” to grow by 56% to 5.7 million upto2012 as compared to 13% increase in those aged 65-84.[3]
The given below chart will provide for the increase in geriatrics (oldies) overall in the world and this will rise up and thus worsened.
Important conclusions of the chart: there is continuous increase in the geriatric person decade wise.
54.6 million Population of geriatrics is postulated for 2020 and influencing increase till 2030 of 71.5 million is expected.[4]
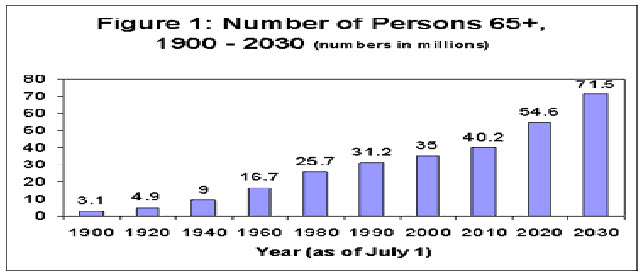
Figure.1: Bar graph showing yearly increase in geriatrics expecting 71.5 million old people in 2030.[4,5]
With neurological disorders the normal cerebral aging pattern got altered and the more serious effects can be seen in the individuals early in the ages. Some of the neurological disorders and their related cognitive impairment (dementia i.e. forgetfulness) is correlated under:
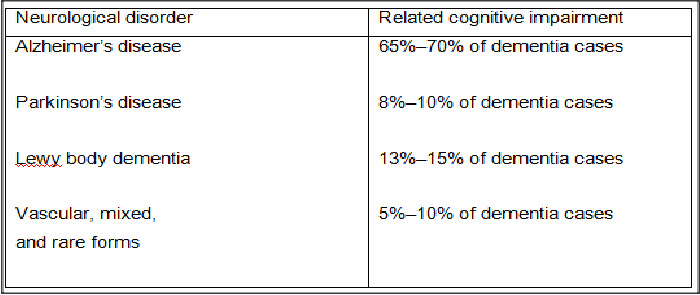
Data giving a reason, neurological disorders are closely studied with the phenomena of cerebral aging. The best scholars are working on the reasons of cerebral aging and possible therapies to cure them. The recent advancement of technologies like Proton Emission Tomography, Radiography, etc. provided best diagnosis to relate structural changes (from molecular to organ level) to the Cognitive impairment and neurological disorders.[6]
Further, researches in preclinical and clinical level had provided the pharmacotherapy for the individual. One of the newest drug for Cerabral aging is TRIVASTAL LA by Serdia Parma.(Biperiden) is marketed with dose of 50mg, pharmacological action is selective D2/D3 dopamine receptor agonist with additional α2-noradrenergic properties.[7]
DISCUSSION:
Cerebral aging is the natural phenomena, explained by different scholars in view of different mechanisms given below:
(1) Single Mechanism: Explains that particular reason is the cause of cerebral aging.
Salthouse says, increase in age is the cause of cerebral aging. Baltes & lidenberg says that, decrease in crude measure of sensory function of visual and auditory is the reason of cerebral aging related impairments.
(2) Specific Cognitive Mechanism: explains that executive functions i.e. ability to switch in tasks, inhibitory functions & working memory processes decreases with age.[8]
Executive functions are required for:
• Reasoning
• Encoding
• Strategy
• Retrieval of information from long term memory.
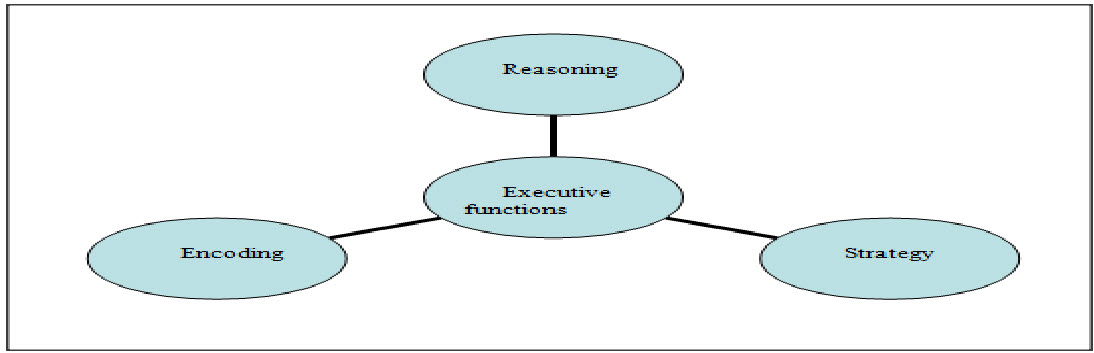
Figure.2: Various executive functions that are being impaired in cerebral aging process.[9]
Cerebral aging related cognitive disorders are mostly recognized as,
(a)Decrease in working memory: Working memory is the centrally executive system, which is important to run all the cognitive tasks requiring effortful processes.
Working memory works by the two passive storage subsystems which are specific for verbal and visio-spatial domains. So, the impairment to these subsystems is the prior cause of inefficiency of working memory.
(b)Loss of Specificity or Differentiation in brain recruitment while performing an array of cognitive targets. Also different parameters of analysis are day to day decrease in personal efficiency to do the work efficiently.[10]
Causes:
(1) Role of Inhibition: Geriatrics are less effective at inhibiting irrelevant information and so these will form “mental clutter”, a dumped place in working memory. This shows that while working memory space is same but due to mental clutter it seems diminished. So, improper inhibition results decrease of working memory and thus execution of cognitive action.
(2) Brain atrophy: With age brain shrinks and cause volumetric changes but the change is not uniform, frontal cortex shrinks more, medio-temporal areas less and the occipital cortex at least.
This lead to decline in memory requires executive functions i.e. tasks requiring, strategic and effortful processes. While the other functions related to recognize and listening remains intact a bit.
(3) Oxidative Stress: Caused due to vasoconstriction leading to decrease in blood supply further causing parenchymatous damage. Parenchymatous damage further causes decrease in metabolic demand worsening blood supply further.[11]
(4) Lipid Peroxidation & accumulation of lipofuscin pigment in brain regions.
(5) Neurotransmitter deficiency:
1. Cholinergic deficiency:
It relates to decrease in acetylcholine in nervous system due to many reasons like decrease in cholineacetyl transferase, less choline content in body. In this condition the cholinergic receptors remain intact but the decrease in Ach will lead to impairment.
Cholineacetyl transferase (chat) deficiency is mild in normal patients but more profound in Alzheimer’s disease (here frontotemporal cortex and hippocampus are majorly affected).
2. Noradrenergic deficiency:
Deficit of Adrenaline and Noradrenalin (the major excitatory and responsive neurotransmitter) will lead to the basic causes of geriatric related cognitive impairment. [12]
(6) Drug Toxicity or Adverse Reactions: Drug therapy has contributed significantly to the management of numerous medical conditions in older patients, a substantial number of these individuals will experience some sort of Adverse Drug Reaction (ADR). ADRs have been recognized as a serious health problem, and one US Government report estimated that 10% to 15% of geriatric hospital admissions were caused by ADRs.
The relative odds of an ADR specifically related to cognitive impairment in older individuals have also been found to increase as the number of prescription drugs increased.
Cognitive impairment is a broadly definable ADR, which is extremely important in older people and one to which they seem to have heightened susceptibility. Symptomatology includes disorders that can be termed “psychiatric” and/or “neurologic,” and often occurs on a continuum. Some drugs that are linked with discretely classifiable outcomes, such as depression and suicide or seizures, are often also noted to cause a variety of more subtle central nervous system (CNS) disturbances as well, such as confusion or decreased sensory gain. Such symptoms are more difficult to assess and could clearly have an impact on cognitive abilities.
However, these drugs may more routinely be considered in the context of their most dramatic adverse sequelae, and may be overlooked when considering drugs that can impair “cognition.”[13]
Drugs used for sedation, for example, may impair cognition in the course of exerting their therapeutic effect without an undesired outcome if the setting is proper and the effect terminates in a predictable and expected manner.
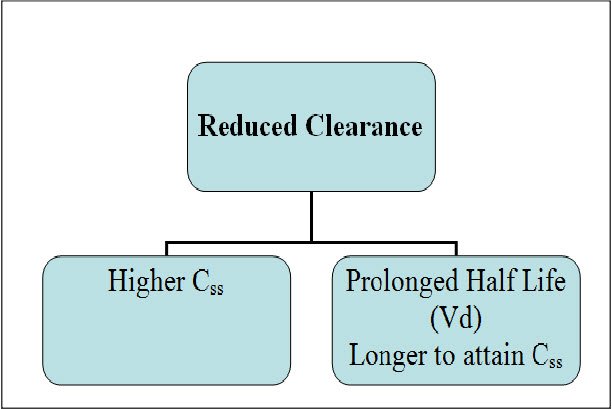
Figure.3: Consequences of reduced clearance in the elderly. For any given drug, impairment of the capacity for drug elimination (reduced clearance) will cause an elevation in steady-state concentrations (Css) with a resulting increase in the likelihood of toxicity. Reduced clearance also may cause a prolongation of elimination half-life, and a consequent delay in the rate of attainment of the steady-state condition. An increase in volume of distribution (Vd) may also contribute to a prolongation of elimination half-life.[14]
Aged individuals are commonly on multiple medications increases the risk of all ADRs, including those resulting in impaired cognition. Many of the commonly used medications, such as digoxin, psychotropics, and those with anticholinergic (muscarinic-blocking) properties, have been well documented as causes of cognitive disturbances, even when used alone.
A number of intrinsic physiologic alterations also put older individuals at increased risk for cognitive toxicity, including changes in neuroplasticity with resulting changes in drug sensitivity, and changes in drug distribution and elimination with subsequent pharmacokinetic toxicity. These factors form the basis for the age’s increased risk for the development of cognitive problems from medications. [15]
Manifestations of cognitive toxicity:
As with many ADRs, a clear association between drug and cognitive disturbance can be difficult to definitively establish, particularly if the disturbance is subtle and if the impairment is in fact multifactorial in origin. Acute confusional states (delirium) have been most clearly documented by clinical report, but dementia has also been shown to be a presentation of drug toxicity. Delirium is characterized by disturbed consciousness with reduced ability to focus, sustain, or shift attention. Onset is usually rapid with fluctuations in levels of impairment over the course of a day. Such patients also frequently exhibit confusion, agitation, delusions, and/or hallucinations. Many medications have been reported to cause delirium, such as those with anticholinergic activity, as well as opioids, sedatives, anxiolytics, and others. It is also important to recall that withdrawal from some sedative-hypnotics and anxiolytics, has also been reported to precipitate delirium.
Dementia associated with medication use involves multiple cognitive deficits, including memory impairment with accompanying deficits in speech, recognition, motor and sensory ability, or other executive functions (such as planning, organizing, or abstracting). Onset is generally insidious, and progression is slow. Drug treatment may not be ongoing at the time the condition is identified, but, in general, has previously been prolonged and intensive. Sedative-hypnotics, anxiolytics, anticonvulsants, and intrathecal methotrexate have all been reported to cause dementia.[17]
Investigators examining the effect of particular drugs in controlled settings are able to assess less global or drastic, but still definitive effects by using formal testing to measure effects on memory, attention/concentration, reaction time, and executive function in relation to drug exposure. For example, impairment of mental skills in older subjects has been found to be greater and more persistent than in younger subjects following administration of some benzodiazepines, such as triazolam and alprazolam .Some data suggest that the aged are more sensitive to the effects of any given plasma level of these drugs. Similarly, cognitive decrements have been measured following oxybutynin and diphenhydramine .These deficits can be assessed using various methods such as arithmetic calculation, digit recognition, simple reaction time, and the digit symbol substitution test.
Sedating drugs can clearly impair awareness of hazards and diminish reaction time, and overall sedation and reaction time have been recognized as two potentially important factors in falls.
An anticholinergic drug administered to an aged person, for example, blocks postsynaptic acetylcholine receptors in a CNS that already has compromised cholinergic system activity. The result can be confusion, disorientation, and memory loss, which would not occur in a younger person with more baseline acetylcholine neurotransmission.[18]
Drug classes implicated in the concurrence of cognitive toxicity:
The following drugs or drug classes have been implicated in the concurrence of cognitive toxicity:
1. Selegiline:The most frequent problems include delirium, hallucinations, agitation, and overall sedation.
2. L-dopa: Used as a sole agent or in combination with carbidopa, a variety of cognitive problems have been reported to be associated with its use.
3. Amantadine:Used as an antiviral as well as in Parkinson’s disease, therapy has been linked to suicide attempts in patients with and without previous psychiatric problems. These patients exhibit a variety of abnormal mental states, including confusion, depression, paranoia, personality changes, and aggressive behavior. In aging populations, where its use would most likely occur, clearance is reduced and plasma levels are higher at standard doses.
4. Phenytoin:The CNS is the most common site of toxicity, which appears to be dose-related, but can occur even within the usual effective serum concentration range of 40 to 79 µmol/L. Confusion as well as speech and coordination difficulties are common.
5. Digoxin: Some data indicate that this drug ranks first in the number of prescriptions made out to the elderly in the US. A spectrum of CNS-related effects can occur, including depression and anxiety as well as confusion and delirium with hallucinations. Such symptoms may appear in the absence of cardiac toxicity and at therapeutic plasma levels (0.6–2.6 nmol/L). Clearance of digoxin correlates with renal function as determined by creatinine clearance, which generally declines with age.
6. Alpha Blockers: Symptoms ranging from depression to memory disturbances and pseudodementia have been attributed to individual drugs, including propranolol and local use of timolol in glaucoma.
7. Lidocaine: Symptoms ranging from confusion to delirium are common manifestations of toxicity.
8. Antibiotics: Penicillins, cephalosporins, quinolones, and imipenem/cilastatin have all been shown to cause cognitive disturbances, particularly at high doses in renal insufficiency, severely ill patients, and/or patients with increased blood–brain barrier permeability. Quinolones such as ciprofloxacin can cause events such as anxiety and agitation, while imipenem can precipitate confusion (as well as convulsions).
9. Corticosteroids:Particularly at higher doses, drugs such as prednisone can precipitate psychosis. Memory and attention deficits have also occurred during chronic therapy.
10. Immunochemotherapy: Both interferon-alpha and interleukin-2 have been linked with serious depression.
11. Opiate analgesic: Symptoms ranging from overt sedation to depression and delirium have occurred with many of the narcotics and vary with the clinical setting (postoperative vs. chronic pain management). Some investigators feel that meperidine may be more likely to cause symptoms because of the anticholinergic nature of its metabolite, normeperidine.[19]
Treatment:
Therapeutic implication of Neurotransmitter deficits:
1. Acetylcholine precursors:
1. Choline oral source: Natural food contains little choline salts most is found as lecithin in eggyolk, meat, fish and soyabean oil. Lecithin (phosphatidyl choline).
2. Inhibition of acetylcholine hydrolysis: Physostigmine(esterase blocker), Centrally acting AchE inhibitor: improves long term memory and reverse the scopolamine induced memory deficiency.[21]
2. Direct Cholinegic agonists: Arecholine.
3. Noradrenegic Agonists:
1. Levodopa
2. Ritalin
3. Metrazol
4. Adrafinil
5. modafinil : medications improving alertness
(Ritalin and metrazol causes adrenergic “mood elevation”)
4. Other Neuromodulating drugs for cerebral aging:
1. Hydergine (6mg):It has high affinity for NA receptors in brain causing increase in Cyclic AMP at receptor level relating improve in metabolic functioning of brain cells. Also increases cerebral blood flow. Indicated for mild to moderate dementia. Improves cognitive functions, self care abilities, motivation and mood disorders in elders.[22]
2. Nootrophil: Cyclic derivative of GABA. Increase energy stores in the brain and promotes interhemispheric transfer of information.
3. Vasopressin: First neuropeptide used for improving cognitive functions in elders. Nasal Spray used for amnesic and demented patients. Act by stimulation of ACTH secretion which in turn improves attention arousal system of elderly. Causes release of other peptide modulators too e.g. endorphins.[23]
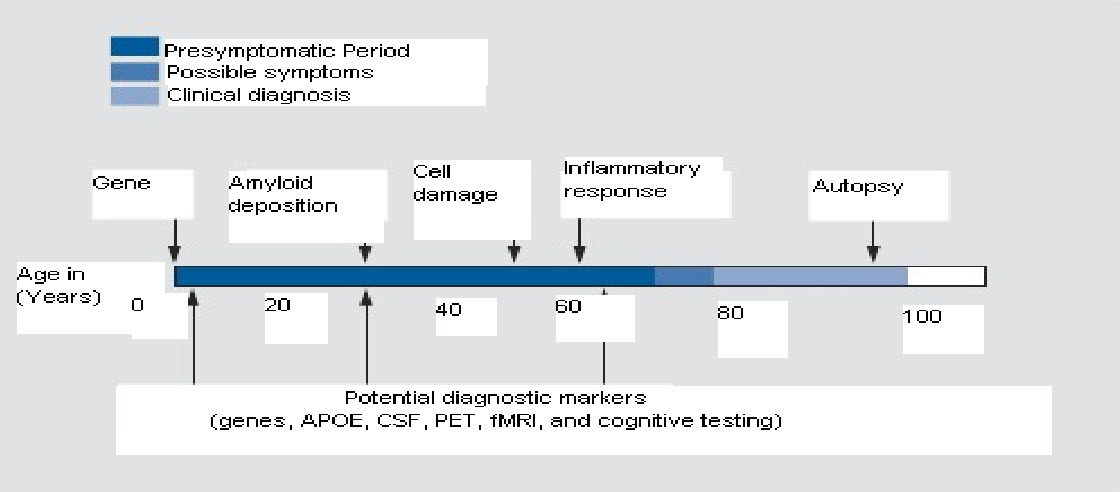
Figure.4: Potential physiological pathways to Alzheimer’s Disease, APOE, apolipoprotein E , CSF , PET, fMRI .[24]
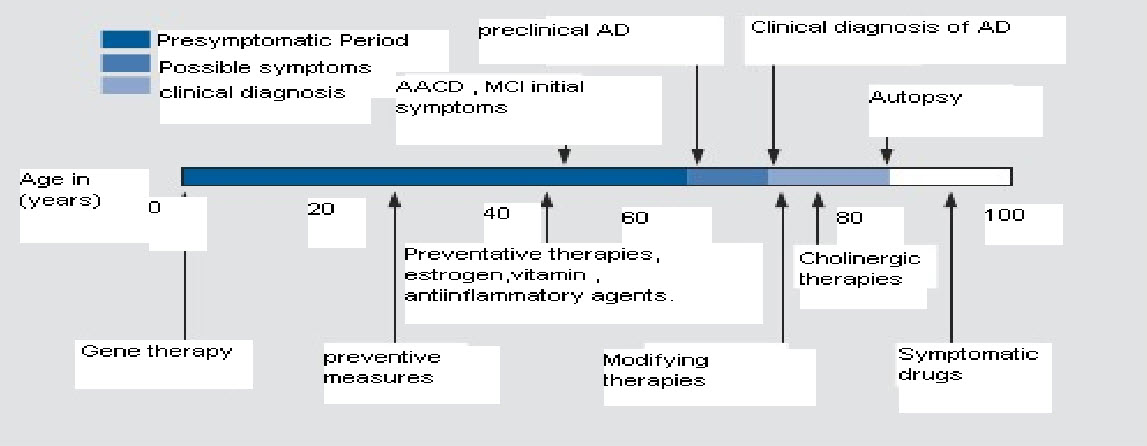
Figure.5: Typical clinical course current and future therapeutic. AACD, age- associated cognitive decline; AD, Alzeimer's disease; MCI, mild congitive impairment.
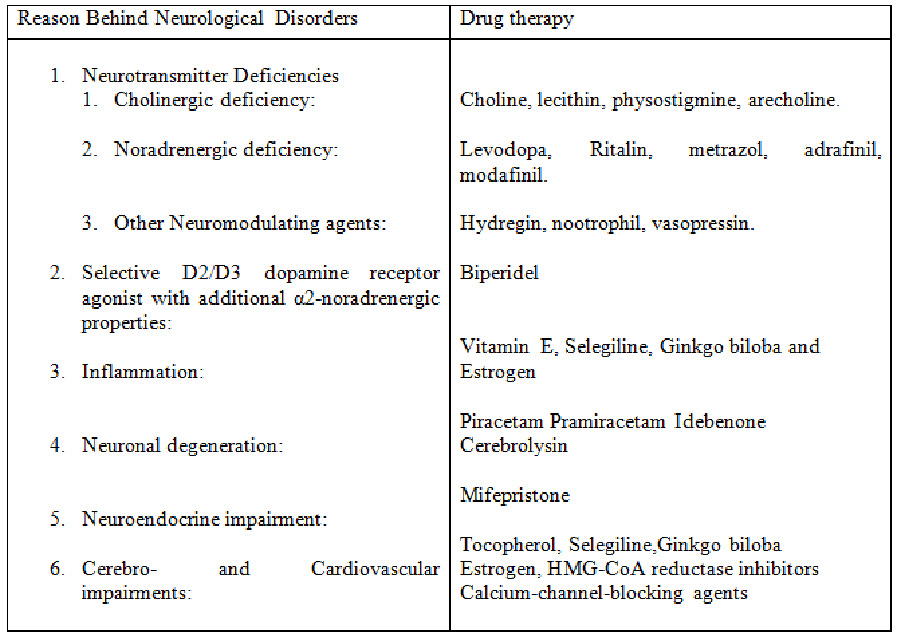
Table showing possible drug therapy for the particular neurological disorder characterized by the reason behind:[25]
Ayurvedic Treatment:
1. Brahmihelps to dilate the cerebral blood vessels improving circulation to the brain.
2. Bacopa, bhringaraj and shankhapushpihelp enhance mental performance and promote intelligence.[26]
3. Nasya oilhas been used for centuries to improve voice, vision and bring clarity of Mind.
4. Tulsi tailam, use on scalp and having 3-5 leaves of the “wonder drug” is may prove benificial in Neurocognitive disorders.[27]
Non Pharmacological treatment:
Treatment includes providing older adults with memory supports that bypass the need to encode items actively or deliberately, thus lessening the executive processing requirements of the tasks.
Specific examples in which environmental supports have effectively repaired the memory of older adults include:
1. Using matching picturesto support memory for sentences, resulting in dramatically better memory in older adults (probably due to dual coding of the material) and
2.Providing older adults with memory cuesthat are conceptually related to target words, resulting in larger memory improvements for the words in the old compared with the young.[28]
Further practice of Yoga is the beneficial part to revive the dead cells and potential of body efficiently. Utilizing Brahamri Pranayam is one of best possible outcome to be in future since it revitalizes the neuronal cells by vibration(OM) lead to their utmost efficiency and thus the age related cognitive decline can be combated.
Proper lifestyle, the healthy one will lead to the normal aging (the rule of life-aging-death) without impairing the cognitive actions to large extent. So, advisable part is to stop using tobacco, have a nice breath full of oxygen to revitalize the cells of body, perform yoga and exercise.
Precautions & Suggestions:
1. A balanced diet of fresh, organic fruits and vegetables is best including some nuts and ghee.
2. Avoid cheeses and meats.
3. Add carrots and beets to your diet.
4. Avoid alcohol, marijuana and other drugs which directly damage brain tissue and affect memory.
5. Limit caffeine which stresses the nervous system, causing the mind to jump from thought to thought.
CONCLUSION:
Cerebral Aging & Neurological Disorders is a vast topic & the work done on this topic will never be said complete, but still every effort is made to give best of best data related.
As per the work done on the topic it is being concluded that the, Cerebral Aging is a topic of present era since the ratio of geriatrics in population is on higher ratio, so to preserve the efficiency cerebral aging has to be controlled. Yes , the cerebral aging is the natural phenomena leading soon after puberty but still it causes drastic disorders in young when forced by some etiological factor known or not.
Various neurological disorders can cause additive problems with cerebral aging out of all Alzheimer’s disease is one leading a major concern.
Further it will be necessary to be abreast of knowledge that which medication or health aid, both prescription or nonprescription, can cause disorders of cognition. It should not be necessary to under treat the elderly and deprive them of the benefits of pharmacotherapy in order to avoid toxicity. A high level of vigilance and care should keep the therapy that is intended to extend life and enhance its quality from diminishing vital cognitive capacity in geriatrics.
Development of new technologies like Investigational neuropharmacologic techniques comprise a powerful and complementary collection of research tools for studying the effects of aging and disease on regional and specific measures of brain function. These have allowed us to characterize both the normal neurochemical changes that accompany successful aging and the accelerated or aberrant alterations seen in neuropsychiatric and behavioral dysfunction. Future work will carry the findings of the past decade into the realm of intervention.
Advancements in structural and functional imaging naturally complement those in molecular neurobiology and genetics, but we are just beginning to realize their potential combined power. For example, the recent availability of animal PET scanners presents the opportunity for the in vivo study of genetic models of disease, such as AD. Further, neuropharmacologic approaches to cognitive enhancement and slowing of dementia progression may be evaluated and monitored by imaging strategies. Indeed, the challenges posed by an increasingly aged population in industrialized nations are formidable, but may best be met by the combined application of developing technologies.
It is likely that just as there are behavioral routes to healthy bodies, there are behavioral routes to healthy minds. The linkage of studies of behavior across the life span will result in critical knowledge that will allow individuals to take control of their cognitive future and alter the neurobiological age of their minds. Such an outcome should offer huge rewards to both individual and to our society. A tremendous national investment in the neuroscience of cognitive aging combined with committed effort and generous cooperation among scholars is needed.
Age related cognitive treatment is always related to the lifestyle so proper lifestyle, the healthy one will lead to the normal aging(the rule of life-aging-death)without impairing the cognitive actions to large extent. So, advisable part is to stop using tobacco, have a nice breath full of oxygen to revitalize the cells of body, perform yoga and exercise.
Being in Oldies is not the age to panic for, it’s the most important part of life when a person is able to give his/her experiences of life able to share that and thus forms the new world already having a knowledge from past experiences of elders.
So, while the Old people are not able to do physical work to large extent but their part in society is of enormous value, so to gain more and more from respected ones, their mental health should be cared for. So, cerebral aging is the topic for growth, to develop and for this continuous work and research is needed and world is moving that way too. Future is not ahead when elementary cause of cerebral aging will be identified, and treatment to nullify them in optimized manner will be developed.
REFERENCES:
1.Jernigan T, Archibald S, Berhow M, Sowell E, Foster D, Hesselink J. Cerebral structure on MRI, part I: localization of age-related changes. Biol Psychiatry. 1991;29:55-67.
2.Blatter D, Bigler E, Gale S, et al. Quantitative volumetric analysis of brain MR: normative database spanning 5 decades of life. Am J Neuroradiol. 1995;16:241-251.
3.Miller AKH, Alston RL, Corsellis JAN. Variation with age in the volumes of grey and white matter in the cerebral hemispheres of man: measurements with an image analyser. Neuropathol Appl Neurobiol. 1980;6:119-132.
4.Joan T. Erber, Aging and Older Adulthood, 24 Aug 2011
5.Ito M, Hatazawa J, Yamaura H, Matsuzawa T. Age-related brain atrophy and mental deterioration—a study with computed tomography. Br J Radiol 1981;54:384-390.
6.Murphy D, DeCarli C, Schapiro M, Rapoport S, Horwitz B. Age-related differences in volumes of subcortical nuclei, brain matter, and cerebrospinal fluid in healthy men as measured with magnetic resonance imaging. Arch Neurol. 1992;49:839-845.
7.Christiansen P, Larsson H, Thomsen C, Wieslander S, Henriksen O. Age dependent white matter lesions and brain volume changes in healthy volunteers. Acta Radiol. 1994;35:117-122.
8.Wahlund LO, Agartz I, Almqvist O, et al. The brain in healthy aged individuals: MR imaging. Radiology. 1990;174:675-679.
9.Golomb J, Kluger A, de Leon MJ, et al. Hippocampal formation size in normal human aging: a correlate of delayed secondary memory performance. Learn Mem. 1994;1:45-54.
10.DeCarli C, Murphy D, Gillette J, et al. Lack of age-related differences in temporal lobe volume of very healthy adults. Am J Neuroradiol. 1994;15:689-696.
11.Resnick S, Davatzikos C, Kraut M, Zonderman A. Longitudinal changes in MRI volumes in older adults. Presented at First International Meeting of the Alzheimer's Imaging Consortium 2000. Washington DC. 2000.
12.Autti T, Raininko R, Vanhanen SL, Kallio M, Santavuori P. MRI of the normal brain from early childhood to middle age. I. Appearances on T2- and proton density-weighted images and occurrence of incidental high-signal foci. Neuroradiology. 1994;36:644-648.
13.Horikoshi T, Yagi S, Fukamachi A. Incidental high-intensity foci in white matter on T2-weighted magnetic resonance imaging. Frequency and clinical significance in symptom-free adults. Neuroradiology. 1993;35:151-155
14.Longstreth W, Manolio T, Arnold A, et al. Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. The Cardiovascular Health Study. Stroke. 1996;27:1274-1282.
15.Yetkin F, Fischer M, Papke R, Haughton V. Focal hyperintensities in cerebral white matter on MRI images of asymptomatic volunteers: correlation with social and medical histories. Am J Roentgenol. 1993;161:855-858.
16.Kalaria R. Cerebrovascular degeneration is related to amyloid protein deposition in Alzheimer's disease. Ann N Y Acad Sci. 1997;826:263-271.
17.Pantoni L, Garcia J. Cognitive impairment and cellular/vascular changes in cerebral white matter. Ann N Y Acad Sci. 1997;826:92-101.
18.Hatazawa J, Shimosegawa E, Satoh T, Toyoshima H, Okudera T. Subcortical hypoperfusion associated with asymptomatic white matter lesions on magnetic resonance imaging. Stroke. 1997;28:1944-1947.
19.Kuwabara Y, Ichiya Y, Sasaki M, et al. Cerebral blood flow and vascular response to hypercapnia in hypertensive patients with leukoaraiosis. Ann Nucl Med. 1996;10:293-298.
20.Whitehouse PJ, Price DL, Struble RG, Clark AW, Coyle JT, DeLong M. Alzheimer's disease and senile dementia: loss of neurons in the basal forebrain. Science. 1982;215:1237-1239.
21.Francis PT, Palmer AM, Snape M, Wilcock GK. The cholinergic hypothesis of Alzheimer's disease: a review of progress. J Neurol Neurosurg Psychiatry. 1999;66:137-147.
22.Little JT, Johnson DN, Minichiello M, Weingartner H, Sunderland T. Com-bined nicotinic and muscarinic blockade in elderly normal volunteers: cognitive, behavioral, and physiologic responses. Neuropsychopharmacology.1998;19:60-69.
23.Mohs RC, Rosen WG, Davis KL. The Alzheimer's disease assessment scale: an instrument for assessing treatment efficacy. Psychopharmacol Bull.1983;19:448-450.
24.Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer's disease. Am J Psychiatry. 1984;141:1356-1364.
25.Folstein MF, Folstein SE, McHugh PH. Mini-Mental State: a practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res. 1975;12:189-198.
26.Michelle Morgan, Herbs to Enhance Mental and Physical Performance, MediHerb a Phytotherapist’s perspective: No. 39 July 2004.
27.K. MIYAMOTO, Alternative Medicine for the Elderly, Editors: E. Paul Cherniack MD, Neil Cherniack PhD, Springer Link, 2003
28.Cerebral aging: integration of brain and behavioral models of cognitive function, Denise C. Park, PhD, Thad A. Polk, PhD, and Christy Marshuetz, PhD, Dialogues in Clinical Neuroscience, Sep. 2001 151-65
REFERENCE ID: PHARMATUTOR-ART-2203
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 7 Received On: 07/05/2014; Accepted On: 12/05/2014; Published On: 01/07/2014How to cite this article: A Khunteta, V Pareek; Cerebral Aging and Neurological Disorders; PharmaTutor; 2014; 2(7); 29-39 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









