ABOUT AUTHORS
M. Manasa Rekha*,
Department of Pharmacy Practice,
Annamacharya college of Pharmacy,
Rajampet, Andhra Pradesh, India.
*manasarekharoyal@gmail.com
ABSTRACT:
The study aims to assess the role of clinical pharmacist in Improving the quality of life of HIV patients in an antiretroviral therapy wards of a teritary care teaching hospital
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2524
INTRODUCTION:
Patient counseling is a broad term which describes the process through which health care professionals attempt to increase patient knowledge of health care issues. Patient counseling may be verbal or written performed on an individual basis or in groups, & provide directly to the patient or caregiver. The process provides for the exchange of information between the patient & health practitioner. The information gathered is needed to assess the patient’s medical condition to further design, select, implement, evaluate & modify health interventions.
Outcomes of patient counseling:
• Patient recognizes the importance of their well being.
• It encourages the patient to establish a working relationship with a pharmacist & foundation for continual interaction and consultation.
• Improves the coping strategies to deal with medication side effects and drug interactions.
• Motivates the patient to take medicine for improvement of his/her health status.
• The patient becomes an informed, efficient and active participant in disease treatment and self care management.
• Develops the ability in patient to take appropriate medication related decision concerning the compliance or adherence to their medication regimen.
Patient counseling methods:
The structure of the counseling session is divided into four groups: y Introduction of the session.
• Content of the session.
• Process followed.
• Conclusion of the session
• Review the patient record prior to counselling.
• Conduct an appropriate patient counselling introduction by self and patient.
• Explain the purpose of counselling session
• Obtain pertinent initial drug related information. E.g.: drug allergies, and other medications.
• Warn the patient about taking other medications including OTC drugs, herbals, or botanical drugs and alcohol which could inhibit or interact into the prescribed medication.
• Determines whether the patient has any other medical conditions that could influence the effects of their drug or enhance the likelihood of an ADR.
• Asses the patient understandings of reason for therapy. y Assess any actual or problems of importance to the patient.
Patient Counseling contents :
• Discuss the name and indication of the medication.
• Explain the dosage regimen including duration of therapy when appropriate.
• Assist the patient in developing a plan to incorporate the medication regimen into his/her daily routine. Explain how long it will take for the drug to show its effect.
• Discuss storage and refilling information.
• Emphasize the benefits of completing the medication as prescribed.
• Discuss the potential side effect.
• Discuss how to prevent or manage the side effects of the drug. y Discuss the precautions.
• Discuss the significant drug‐drug, drug‐food, and drug‐disease interaction. y Explain precisely what to do if the patient misses the dose.
• Explore the potential problems of the patient
• Provide accurate information.
• Use language that the patient is likely to understand.
• Use the appropriate counselling aids to support counselling.
• Present the fact and order in a logical order.
• Maintain control & direction of the counseling session.
• Probes for additional information.
• Use open‐ended question.
• Display effective non‐verbal behaviours.
• Counseling conclusion steps:
• Verify the patient understanding via feedback.
• Summaries by acknowledging or emphasizing key points of information.
• Provide an opportunity for final concerns or questions.
• Help the patient to plan, follow up and next consecutive steps.
• Expected duration of treatment
• Expected benefits of treatment
• Advice on storage
• What do if dose is missed
Interactive communication requires five key elements:
• open ‐ended questions
• awareness of nonverbal cues;
• active listening
• reflective responses
• verification of understanding
• These questions encourage disclosure of information.
• Closed‐ended questions and leading/restrictive questions elicit yes/no responses and limit the information sought from the receiver.
• These types of questions should be avoided. Example: Closed‐ended: "Do you know how to take your medication?"
• "Yes." Leading/restrictive: "You're familiar with your medications, aren't you?“
• "Yes.“ Open‐ended: "What did the doctor tell you about taking the medications?
Nonverbal clues
• Appropriate nonverbal cues are also critical for effective communication.
• Facial expressions, body posture, gestures, tone of voice and use of eye contact are all forms of nonverbal communication.
• Skilled use of our nonverbal communication can make the difference between successful interactive dialogues and frustrating nonproductive encounters.
• What we say and how we say it must have the same meaning.
• When nonverbal cues are inconsistent with the words spoken, people tend to believe the nonverbal message.
Appropriate non‐verbal clues:
• Friendly and smiling facial expressions.
• Varied eye contact(consistent, but not startling).
• Professional appearance.
• Relaxed, warm and comfortable gestures.
• Attentive body posture(slightly leaning forward).
• Appropriate personal space(18‐48 inches).
• Varied voice rate and volume to keep the individual interested. However, a high pitched voice should be avoided.
Distracting non‐verbal clues:
• Lack of eye contact may indicate little confidence or interest.
• Insufficient spatial discomfort(causing discomfort).
• Unfavorable tone of voice(can upset the people and create an unintended meaning).
• Slouching or weight shifted to one side(may indicate lack of interest).
• Messy work environment.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Reflective responses
Reflective responses reflect back to the sender the receiver's understanding of both the content of what was said and the feelings that were expressed.
Patients who should always be counselled
• Confused patients
• Patient with hearing impairment
• Poor literacy
• Patients profile change with dosing
• Transferring of prescription
• Patient s receiving drugs with special storage requirements
Patients should be counseled at certain intervals
• Asthamatic patients
• Diabetic patients
• Patients receiving 4 or more drugs
• Patients who are mentally ill
• Epileptic patients
• Patients misusing drugs
• Patients who are terminally ill.
METHODOLOGY:
AIM:
The study aims to assess the role of clinical pharmacist in Improving the quality of life of HIV patients in an antiretroviral therapy wards of a teritary care teaching hospital.
OBJECTIVES:
The Main Objective Of The Present Study Includes, Improving Quality Of Life Of HIV infected Patients, Achievement Of Patient Medication Adherence ,Life Style Modification ,Psychological Building, Creating and Improving Social awareness about HIV, Improving the Patient health related outcomes.
METHODOLOGY:
Study Design: It is a Prospective observational study.
Study Period: The Present study was conducted for a period of 24 months from march 2015 to march 2017.
Study site : The Present study was conducted in ART Department at Rajiv Gandhi Institute of Medical Sciences ( RIMS), Kadapa.
Sample size: The Patients taken for the present study period of 24 months it was 70 patients.
Source of Data: All the patients satisfying the inclusion criteria were selected from ART department in Rajiv Gandhi institute of medical sciences (RIMS) Government Hospital, Kadapa. All the required data was collected from patients through Patient representative interview and case sheets and treatment charts.
Inclusion criteria
• Patients with aging above 18 years and below 60 years.
• Patients with serological HIV positive.
• The Patients who are willing to participate in the study.
Exclusion criteria
• Patients who are not willing to Participate in the study.
RESULTS:
AGE WISE DISTRIBUTION OF MALE POPULATION:
In this study total of 70 patients were enrolled in the study. The males population is 42.The age wise male Patients population ranges from 2(4.7619 ) Patients were in the age group of 10-20 years ,11(26.1904 )Patients were in the age group of 20-30 years, 12(28.5714) patients were in the age group of 30-40 years ,9(21.428) patients were in the age group of 40-50 years ,8(19.0476 )Patients were in the age group of 50-60 years.
Table 1.1 Age wise distribution of male patients
|
Age in years |
Total number of Patients |
Percentage (%) |
|
10-20 |
2 |
4.7619 |
|
20-30 |
11 |
26.1904 |
|
30-40 |
12 |
28.5714 |
|
40-50 |
9 |
21.428 |
|
50-60 |
8 |
19.0476 |
|
Total |
42 |
100 |
|
|
|
P value <0.0001 |
Fig 1.1 Age wise distribution of male patients

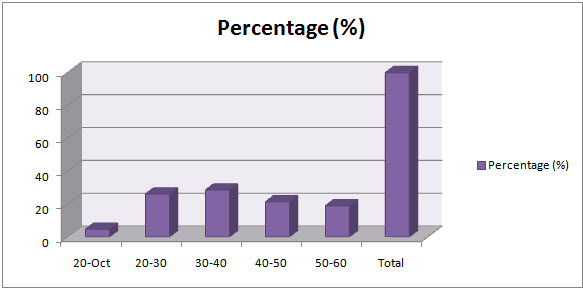
Fig 1.2 Age wise distribution of male patients showing percentage of distribution.
AGE WISE DISTRIBUTION OF FEMALE POPULATION:
In this study total of 70 patients were enrolled in the study. The Females population is 28.The age wise Female patients population ranges from the 0 Patients were in the age group of 10-20 and 14 (50 ) were from 20-30 years, 10( 35.71428 ) Patients were in the age group of 30-40 years and 3(10.714 ) patients were in the age group of 40-50 years and 1(3.5714 )patients were in the age group of 50-60 years .
Table 1.2 Age wise distribution of Female Patients
|
Age |
Total |
Percentage (%) |
|
10-20 |
0 |
0 |
|
20-30 |
14 |
50 |
|
30-40 |
10 |
35.71428 |
|
40-50 |
3 |
10.714 |
|
50-60 |
1 |
3.5714 |
|
Total |
28 |
100 |
|
|
|
P value <0.0001 |
Fig 1.3 Age wise distribution of Female patients.


Fig 1.4 Age wise distribution of Female patients showing percentage of distribution.
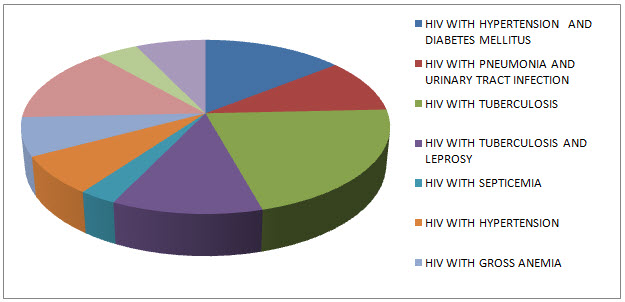
TABLE 1.3 SHOWING MEDICAL DIAGNOSIS CASES OF HIV WITH OTHER COMORBIDITIES TO WHOM THE QUALITY OF LIFE IMPROVED AFTER PATIENT COUNSELING WAS DONE.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
|
VARIOUS MEDICAL DIAGNOSIS CASES |
TOTAL |
|
HIV WITH HYPERTENSION AND DIABETES MELLITUS |
10 |
|
HIV WITH PNEUMONIA AND URINARY TRACT INFECTION |
7 |
|
HIV WITH TUBERCULOSIS |
15 |
|
HIV WITH TUBERCULOSIS AND LEPROSY |
8 |
|
HIV WITH SEPTICEMIA |
2 |
|
HIV WITH HYPERTENSION |
5 |
|
HIV WITH GROSS ANEMIA |
5 |
|
HIV WITH AGRANULOCYTOSIS |
10 |
|
HIV WITH ASTHMA AND COPD |
3 |
|
HIV WITH OTHER COMORBIDITIES |
5 |
|
Total Cases |
70 |
Fig 1.4 Showing Medical Diagnosis Cases Of Hiv With Other Comorbidities To Whom The Quality Of Life Improved After Patient Counseling Was Done
RESULTS AND DISCUSSION:
A total 70 patients were screened during the study period. In this study total of 70 patients were enrolled in the study, The males population is 42.The age wise male Patients population ranges from 2(4.7619 ) Patients were in the age group of 10-20 years ,11(26.1904 )Patients were in the age group of 20-30 years, 12(28.5714) patients were in the age group of 30-40 years ,9(21.428) patients were in the age group of 40-50 years ,8(19.0476 )Patients were in the age group of 50-60 years. In which 28 patients were female and 42 patients were found as male patients. In this study total of 70 patients were enrolled in the study. The Females population is 28.The age wise Female patients population ranges from the 0 Patients were in the age group of 10-20 and 14 (50 ) were from 20-30 years, 10( 35.71428 ) Patients were in the age group of 30-40 years and 3(10.714 ) patients were in the age group of 40-50 years and 1(3.5714 )patients were in the age group of 50-60 years.And counseling was done toall the above patients and quality of life is improved after counseling as the present study is highly significant as the P value <0.0001.
CONCLUSION:
The present study concludes that clinical pharmacist play a key role in patient safety, Particularly in ART department they are important for Improving Quality Of Life Of HIV Infected Patients through patient counselling by making the patients adhere to their day to day medication use by medication adherence, they are much needed to improve psychological building of HIV infected ones and to create and improve social awarness about HIV infection and its transmission.
REFERENCES:
1. *M. Manasa rekha ,A. Bharath kumar ---a prospective study on implementation of clinical pharmacy services to general medicine department in a teritary care teaching hospital published in journal of pharma research in ISSN: 2319-5622.
2. Frank D. Dundee, Dominic M. Dundee, and David M.Noday, Pediatric counseling and medication management services: Opportunities for community pharmacists, Journal of the American pharmaceutical association., 42, 2002,556-567.
3.G Parthasarathi, Karin nyfort-hansen, Milap C Nahata. A textbook of clinical pharmacy practice, second edition, Indcom Press, India, 2012, 2-18.
4.Parthasarathi G, Hasan KN, Nahata MC. A Text Book of Clinical Pharmacy Practice. 3rded., Chennai, India; Orient longman private limited: 2004.
5.Javedh Shareef, Sajitha M S, C. S. Shastry.Impact of Pharmacist Provided Patient Counseling on Quality of Life Inpatients with Asthma in a Tertiary Care Teaching Hospital.International Journal of Pharma Research & Review, Feb 2014; 3(2):1-10.
6.A.Bharath kumar,B.Kumar,M.Saipavan,M.Gobinath.A Review on scope importance and future needs of clinical pharmacy practice in india. International journal of current trends in Pharmaceutical research.2015, 3(3): 916-923.
7.A.Bharath Kumar,Kumar B, RameshD, Gobinath M.A Review On Pharamcotherapy And Management Of Tuberculosis.International journal of Pharmaceutical research and bio sciences, 2014; Volume 3(5): 406-436.
8.Bharath A,Ramesh D, Kumar B, Gobinath M.Prevention And Management of Hiv Aids.Ijprbs, 2014; Volume 3(3): 217-235.
9.A.Bharath Kumar,S.P.Zakiullah,M.Manasarekha.A Review On Stroke Prevention And Management Through Life Style Modifications.World Journal of Pharmaceutical Research. Vol 5, Issue 5, 2016.
10.American College of Clinical Pharmacy. Pharmacotherapy 2008-28 (6), 816–817.
11.American College of Clinical Pharmacy.The Definition of Clinical Pharmacy. Pharmacotherapy 2008; 28(6):816-817.
12.Marie Cicelie.C.Ng,MonetM.Loquias.Retrospective Quality Assessment of a Hospital-Based Drug Information Service.International Journal of Pharmacy Teaching & Practices 2013, Vol.4, Issue 3, 724-730.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









