ABOUT AUTHORS:
Mr. Shaikh Parvej H*, Chilwant K.M., Birajdar Shivprasad M., Prof. Garad S.V.
Maharashtra College of Pharmacy,
Nilanga, dist. Latur (MS) 413521, India
*parveja2r@gmail.com
ABSTRACT
E-Prescribing is a prescriber's ability to electronically send an accurate, error-free and understandable prescription directly to a pharmacy from the point-of-care - is an important element in improving the quality of patient care. Electronic prescribing (sometimes called “eRx”),
Through e-prescribing tools, the physician has access to drug reference checking, drug-allergy interactions, and drug-drug interactions. This additional information up front ensures a safer prescription and reduces pharmacy call backs to the practice to clarify information. Also, the electronic communication is bidirectional; patients can call the pharmacy for a prescription renewal rather than the physician, and the pharmacy can then transmit an electronic message asking the physician to authorize or deny the prescription renewal.
e- Prescription has offering & cure of disease by obtaining data from the foreign expert’s clinical trials, Electronic Prescribing can save time and money. by using software skills of various software likes electronic health record Pharmacy Benefit Manager (PBM)
REFERENCE ID: PHARMATUTOR-ART-1782
INTRODUCTION:
Because of the rising costs of healthcare in the United States, there is a need for some type of healthcare reform. Many leaders view health information technology as an important tool to assist with reducing variations in quality and improving outcomes and efficiency. One of the key areas of focus and opportunity is medication therapy management. Considerable opportunity exists with medication therapy management relative to both cost and patient safety. Approximately USD 287 billion was spent on prescription drugs in the United States in 2007, which was about five times the amount spent in 1993.1 In addition, the World Health Organization has reported that only 50 percent of people typically take their medications as prescribed. The rates are actually lower for certain medical conditions.2 It is estimated that each year approximately 530,000 adverse drug events take place among Medicare beneficiaries alone because of drugs negatively interacting with other drugs the patient is already taking, or there is inadequate information about the patient’s medical history.3 In a 1996 report by the Institute of Medicine (IOM), it was reported that more than 1.5 million Americans are injured annually by drug errors in hospital, nursing homes, and doctors’ offices and more than 7,000 die from preventable medication errors due to illegible handwriting on prescription forms.4 These negative drug events may require costly interventions in order to stabilize the patient. Electronic prescribing is the direct computer-to-computer transmission of prescription information from physician offices to pharmacies Electronic prescribing (sometimes called “eRx”), is an electronic way for doctors to write and send your prescriptions directly to your pharmacy. This means no more prescriptions on paper and less time waiting to have your prescription filled. Physician use of electronic prescribing (e-prescribing) systems to generate legible and complete prescriptions could potentially reduce medication errors and improve physician practice and pharmacy efficiency by mitigating pharmacists’ need for clarification.
EVOLUTION OF E-PRESCRIBING:
RxHub was created in 2001 by three leading pharmacy benefit manager organizations. The purpose of a pharmacy benefit manager is to fund and administer drugs on behalf of insurance companies and employers in order to control costs. RxHub also routes patient medication histories, based on claims data, and pharmacy benefit information to providers. This helps determine if a patient is eligible to receive certain medications based on the insurance plan. SureScripts was also founded in 2001 by the National Association of Chain Drug Stores and the National Community Pharmacists Association. The purpose of the SureScripts link is to provide the electronic communication between pharmacies and physicians. In July, 2008, SureScripts and RxHub merged to form Sure- Scripts-RxHub. In 2009, Sure-Scripts-RxHub was relaunched as SureScripts®. Today, SureScripts® operates the largest electronic prescribing network and is used every day by thousands of providers across all 50 states. In addition to the creation of the technical infrastructure to allow for the communication between pharmacies and physicians, the federal government established incentives for the adoption of e-prescribing. Provisions in the Medicare prescription Drug, Improvement, and Modernization Act (MMA) of 2003 were intended to foster e-prescribing by requiring standards for interoperability and by permitting third parties to offset the implementation costs. The MMA provided prescription drug coverage starting in January, 2006.9 To further promote the adoption of e-prescribing systems, the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) provided that starting in 2009, physicians would be eligible for incentive payments when they e-prescribe for Medicare patients seen in their clinics. Providers will receive a bonus equal to 2 percent of their charges billed to Medicare in 2009 and 2010 with gradual bonus decreases beginning in 2011.The Centers for Medicare and Medicaid Services (CMS) did add a fax exemption, to continue to allow computer-generated facsimile transmissions through January 1, 2012. However, in order to qualify for the e-prescribing incentive payment program, the provider cannot electronically create a prescription and fax it to the dispensing pharmacy. The prescription must be generated and transmitted electronically from the provider’s e-prescribing.
FEATURES:
1. Improved patient safety and overall quality of care.
2. Reduces or eliminates phone calls and call-backs to pharmacies.
3. Eliminates faxes to pharmacies.
4. Streamlines the refill’s requests and authorization processes.
5. Increases patient compliance.
6. Improves Formulary adherence.
7. Increases patient convenience.
8. Offers true Provider Mobility.
9. Improves reporting ability.
10. Fast way of communication between prescriber and acceptor.
11. Doctor can prescribe to patients easily.
12. Patients can retrieve prescription from anywhere by accessing site. Pharmacy can check prescription details and inform doctor easily if there is mistake.
PROCESS OF PRESCRIBING:

Fig: 1 diagram showing prescribing process.
companiesandmarkets.com
FUNCTIONS OF PRESCRIBER:
1. A "qualified" e-prescribing system must be capable of performing all of the following functions generating a complete active medication list incorporating electronic data received from applicable drug plan(s) if available
2. Selecting medications, printing prescriptions, electronically transmitting prescriptions, and conducting all safety checks using integrated decision support systems (safety checks include: automated prompts that offer information on the drug being prescribed, potential inappropriate dose or route of administration, drug-drug interactions, allergy concerns, or warnings of caution)
3. Providing information related to the availability of lower cost, therapeutically appropriate alternatives (if any)
4. Providing information on formulary or tiered formulary medications, patient eligibility, and authorization requirements received electronically from the patient's drug plan
5. Review patients' current medication list and medication history information within the practice.
6. Work with an existing medication within the practice, this can involve viewing details of a medication, remove a medication from the active medication list, change dose, etc., for a medication or renew one or more medications
7. Prescribe or add new medication and select the pharmacy where the prescription will be filled.
8. The information is then sent to the Transaction Hub, where information on the patient eligibility, formulary, and medication history/fill status is sent back to the prescriber.
9. Patient-specific information capabilities (e.g., current patient medication list, access to patient historical data, patient identification)
10. System integration capabilities (e.g., connection with various databases, connection with pharmacy and pharmacy benefit manager systems)
MODEL CONSIDERED IN E-PRESCRIBING PROCESS:
The basic components of an electronic prescribing system are the:
Prescriber - typically a physician
1. Transaction hub
2. Pharmacy with implemented electronic prescribing software
3. Pharmacy Benefit Manager (PBM)
The PBM and transaction hub work closely together. The PBM works as an intermediate actor to ensure accuracy of information, although other models may not include this to streamline the communication process.
PRESCRIBER:
The prescriber, generally a clinician or health care staff, are defined as the electronic prescribing system user and sign into the system through a verification process to authenticate their identity. The prescriber searches through the database of patient records by using patient-specific information such as first and last name, date of birth, current address etc. Once the correct patient file has been accessed, the prescriber reviews the current medical information and uploads or updates new prescription information to the medical file.
TRANSACTION HUB:
The transaction hub provides the common link between all actors (prescriber, pharmacy benefit manager, and pharmacy). It stores and maintains a master patient index for quick access to their medical information as well as a list of pharmacies. When the prescriber uploads new prescription information to the patient file, this is sent to the transaction hub. The transaction hub will verify against the patient index. This will automatically send information about this transaction to the PBM, who will respond to the hub with information on patient eligibility, formulary, and medication history back to the transaction hub. The transaction hub then sends this information to the prescriber to improve patient management and care by completing and authorizing the prescription. Upon which, the prescription information is sent to the pharmacy that the patient primarily goes to.
PHARMACY:
When the pharmacy receives the prescription information from the transaction hub, it will send a confirmation message. The pharmacy also has the ability to communicate to the prescriber that the prescription order has been filled through the system. Further system development will soon allow different messages such as a patient not picking up their medication or is late to pick up medication to improve patient management.
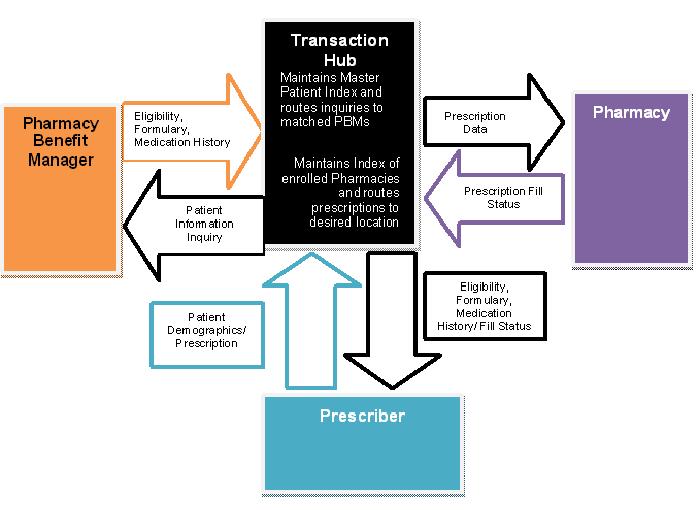
Fig:2 High-level dataflow diagram outlining the roles and processes involved in electronic prescribing (hrsa.gov)
TYPES OF ELECTRONIC PRESCRIBING SYSTEMS:
In order to help meet these aims we evaluated two electronic prescribing systems.
1.ServeRx system
2.Meditech system
1.ServeRx system
ServeRx which was being introduced to a general surgical ward at Charing Cross hospital.The ServeRx system (MDG Medical, Israel) went live in June 2003 as a beta test on a 28-bed general surgery ward in Charing Cross Hospital, part of Hammersmith Hospitals NHS Trust, in West London. Different versions of the system were introduced at different stages, as various upgrades were put into place.ServeRx is a closed-loop system, comprising the following three elements:
1. Electronic prescribing, scheduling and administration software;
2. Ward-based automated dispensing;
3. Electronic drug trolleys.
1. Electronic prescribing, scheduling and administration software
There were two prescribing terminals on the study ward, plus one in the pharmacy department. There were also two hand-held tablet computers on the study ward which can be taken from patient to patient and used to view, prescribe and discontinue medication orders. These had to be synchronised with the ward-based server via a docking station before and after each use. The software used on the prescribing terminals and hand-held computers was windows-based; the patient medication screen was intended to resemble an inpatient drug chart.When prescribing, a doctor could access pull-down lists of all drug products stocked on the ward, all drug products in the Trust’s formulary and all products in the drug dictionary. Prescribing was by product (aspirin 75mg soluble tablets) rather than by drug (aspirin). Default doses were suggested for most products; decision support will be discussed in more detail If the patient had any allergies entered, these were displayed on the prescribing screen. When patients were transferred from other wards, pharmacists were authorised to transcribe their existing medication orders onto the computer system. When patients were transferred from the study ward to other wards, their medication was printed out in a format representing the Trust’s standard medication chart, which allowed a further three days of medication administration to be documented. Pharmacists checked and approved medication orders from a separate pharmacy screen, which indicated unapproved medication orders. Medication orders did not have to be approved before they could be administered by nursing staff. At the approval stage, pharmacists could enter additional instructions relating to administration; further instructions cannot be entered once orders have been approved. The facility for prescribing discharge medication was not in use at the time of this study; discharge medication was therefore prescribed on the Trust’s standard paper discharge prescription
2.Ward-based automated dispensing:
The majority of medication was stored in large automated cabinets; the doses required were transferred by nursing staff to an electronic drug trolley at each drug round (Figure 3). The automated cabinets, containing computer-controlled drawers and a touch-sensitive non-Windows based computer screen, The patient’s name was indicated on the drawer using a liquid crystal display. It was not possible for the nurse to view details of previous medication administration from this screen. Nursing staff were able access medication that was not currently prescribed using a “stat” facility; this was used if medication was needed in an emergency or was prescribed
3. Electronic drug trolleys:
There were two electronic drug trolleys (Figure 4), one for each half of the ward. Each contained twenty drawers and docked with the automated cabinet. When medication was being prepared for a drug round, one drawer in the drug trolley opened at a time, and the patient’s name indicated on the drawer’s liquid crystal display. When all medication for a given patient had been prepared, the system instructed the nurse to close that patient’s drawer in the drug trolley before medication for the next patient could be prepared. Once all medication had been prepared for a given drug round, the trolley could be disconnected from the main system and taken around the ward.It was not possible to view details of drugs due at other times of day, or of previous doses administered or omitted. On completion of the drug round, details of all doses administered and reasons for any omitted were uploaded to the main server once the trolley was docked. Medication prescribed to be given “when required” was generally given separately outside of the main drug rounds.
2.Meditech system
Electronic Prescribing at Queen’s Hospital was part of the wider Meditech Hospital Information System (HIS) Medical notes were maintained in the traditional paper format but all other records were made and stored electronically. The intensive care unit, theatres, outpatients and the private ward were the only departments not to use EP at the time of the study The HIS allowed all authorised staff involved in patient care access to any type of record and supporting information The gateway into the system was through the Patient Care Inquiry module, which allowed the patient to be identified. To enter the system, staff must key in a personal identification number (PIN), which changes every 3 months, and a password, which does not change. Staff had to be trained before they could receive a PIN. Two full-time trainers provided training for all new medical and nursing staff. Pharmacy training was done within the department by members of the core implementation team. Within the hospital, the HIS could be accessed almost anywhere using mobile wireless laptops or static computers or older “dumb” terminals. Most wards had three static terminals and two laptops. Senior staff could also access the system from home. The system had been extensively developed and customized since the initial pilots between 1994 and 1996, and there had been three software upgrades by the time of our study. Version 4.8, which ran on a non-Windows platform and did not require use of a mouse, was in use at the time of this evaluation. Navigation was by function keys, often in combination with shift and arrow keys. The functions assigned to “F keys” could vary depending on the type of static terminal used,
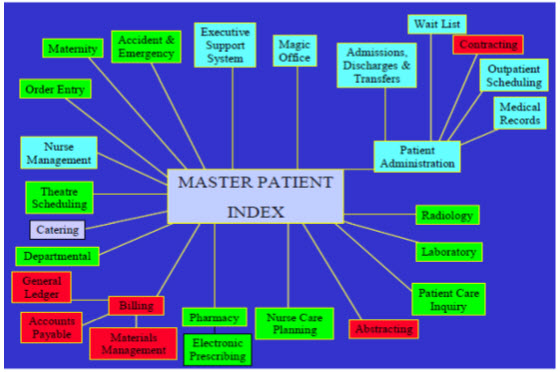
Fig :3 Overview of the HIS meditech.com-
The EP prescribing (order entry) screen followed the logic of the paper drug chart, listing drug, route, dose, times, start and stop dates, administration dates and times (Figures). There were “look-up” functions for drug names, doses and routes, and a print monograph option for individual drugs. There were some decision support rules (see Appendix E for details) but dose checking was not routine at the time of this evaluation. The aide memoiregiven to newly trained prescribers warned that checking for allergies or incorrect doses was their responsibility. Coloured pop-up boxes warned if certain information (such as a stop date for an antibiotic) had not been entered or if a particular caution applied. Full interaction checking was carried out. There were two types of once-only orders: ONE, which was a single dose and STAT which indicated a dose to be given straight away. These had default start and stop dates entered automatically. Regular medicines were allocated times corresponding to ward medicine rounds, with a 2-hour window around the scheduled time to allow for variation in practice. A patient’s current medicines could be listed to screen; paging down gave the details of who prescribed, who gave, and where relevant, who dispensed, the medication. This was called the order history. Discharge medication had to be flagged by the prescriber, then “converted” from inpatient orders in the pharmacy before dispensing. These electronic prescription orders were called down by the pharmacy system in batches, at a frequency set by the dispensary manager. Discharge medication information could be imported automatically into an electronic discharge summary, a printed version of which was sent to patients’ general practitioners.
The laptop was usually placed on the shelf on the side of a conventional drug trolley, where paper drug charts/clip boards or files would rest in other hospitals. The nurse picked the patient name from the list of current admissions, and then checked the patient’s identity in the traditional way by reading the patient’s wristband. The drug administration screen for a patient resembled a compressed drug chart, with medication orders listed on left-hand side of screen and a series of columns to the right. As required and stat medication orders were listed after all other regular medication. New orders for drugs which are not carried as ward stock were flagged *NS*. These items would be picked up by the pharmacy system during regular scans for new orders. Drugs due at the current round were highlighted on the screen. The nurse selected each medication to administer by selecting a tick mark in the relevant column. The screen flagged up any doses which were scheduled, but not given on a previous round. Nurses could view the order history screen to see the reason why previous doses were not given, and can add comments themselves. The recording of each drug administration was signed off separately, as it would be on a paper chart. The system records the actual administration time, and the theoretical “drug round time”
Pharmacists could access and review patient medication orders from anywhere in the hospital. They had the same access as prescribers. However, they normally limited themselves to changes in dose form or dose if these were incorrect, and contacted the prescriber if the drug itself needed changing. They could do this electronically by writing free text notes for prescribers and nurses into the patient record. Each pharmacist carried out a daily prescription review of their allotted wards or consultant firms using the Meditech system. Prescription screening activity was targeted to newly prescribed items, and those which required monitoring New orders which had not been reviewed by a pharmacist are marked *UNR*. Orders for which pharmacists have made an intervention are flagged *I*; these could be audited in detail.
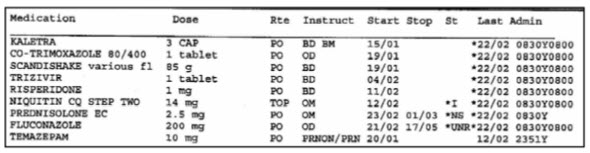
Fig : 4. A current medication record showing scheduled and actual administration times
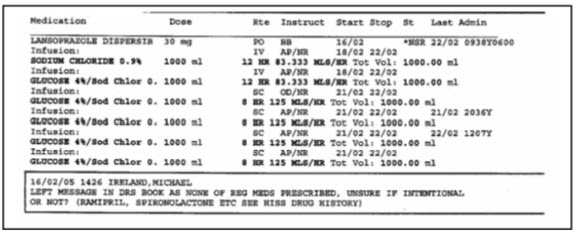
Fig 5.: Example of a note from pharmacist to
Challenges of E-Prescribing:
What are some of the challenges associated with e-prescribing? While there are many benefits associated with electronic prescribing, there are also a number of challenges associated with the implementation and ongoing maintenance of the systems. Funding. A concern for providers is the direct and indirect costs associated with implementing an e-prescribing system. All physicians, but particularly those in small practices, the inner city, or in rural settings, may believe that the cost of a system is too high for them to ever receive a positive return on investment (ROI). Change Management. To implement any health IT requires change management and new workflow systems. For the transition from paper to electronic prescriptions, this change can represent a very large hurdle. Practices are used to doing things in a "certain way" and change can be difficult to get everyone one board (particularly those who are technology averse). Additionally, it can be very time-consuming to conduct the planning, training, and implementation of new electronic systems and workflows. Hardware and Software Selection. Selecting the correct hardware, software, and post-implementation technical support for the practice environment can be difficult for many practices, including small or very busy offices or those that lack information technology staff. Practices often grapple with questions such as:
• Do they use a standalone system or one that is part of an electronic medical Record ?
• How do they select a vendor?
• How do they decide what the system needs to do?
• How do they implement it?
• Is the software certified ?
Connectivity: While almost all chain pharmacies (97 percent) are connected to the e-prescribing system, the vast majority (73 percent) of independent pharmacies are not yet connected. Although most payers or PBMs (representing about 200 million lives) are connected, the patient, formulary, eligibility, or medication history information may not be current. Many small or rural providers and pharmacies face additional issues such as a lack of broadband connectivity and access to information technology professionals to support them.
Standards: With the exception of the requirements set forth by the Centres for Medicare and Medicaid Services (CMS) for use in Medicare Part D, there are no national standards for e-prescribing but they are being developed by the National Council for Prescription Drug Programs (NCPDP). While there are many organizations involved in the development and updating of e-prescribing and related technical standards for the reporting abilities, content and transmission, this work has not been harmonized across vendors and platforms.
State Regulations: There are variations in states about who may prescribe, what may be prescribed and under what circumstances. Reconciliation of those laws and requirements is important because many Americans live in one state and may obtain healthcare (including prescriptions) in another. State governments, such as Connecticut, need to conduct their own analysis of laws and regulations within their own states so as to update to accommodate e-prescribing, such as reconciling paper document retention requirements with electronic data storage, as well as facilitate e-prescribing and other health information exchange (such as remote monitoring and telemedicine) across state lines.
Controlled Substances: To date, the Drug Enforcement Administration (DEA) does not allow electronic transmission of controlled substances, which affects about 20 percent of prescriptions in the US. In July 2008, the DEA released proposed regulations allowing e-prescribing of controlled substances for comment to the public (comments were due on September 25, 2008). Parallel to this effort, the DEA released the final rule of the implementation of the Ryan Haight Online Pharmacy Protection Act of 2008 on April 6, 2009. The Department of Health and Human Services (HHS) is working with the DEA to promulgate regulations governing the issuance of a special registration to practitioners engaged in the practice of telemedicine.
Future of e-prescribing:
MyRxPad has not yet been fully evaluated. We plan to invite prescribers for evaluation through the NLM outreach program, as well as invite users who visit the website to try it out. To make the system more fully functional, we plan to implement electronic transmission of prescriptions using the NCPDP SCRIPT standard. Inclusion of formulary and benefits information would be an additional feature. Extending the application to a platform of a hand held device is much more likely to insure acceptance and use by many prescribers.
Conclusion:
The opportunity that exists with medication therapy management in healthcare is extremely important to the overall issue of rising costs in healthcare. Because the concept of e-prescribing is relatively new, there are still challenges with issues related to workflow; usage with controlled substances; messaging, terminology, and transaction standards; and the overall costs of software, hardware, and integration. However, there are many documented benefits including economic alternatives for patients, eliminating errors from poor handwriting, reducing callbacks from the pharmacy, increasing convenience for the patients, spending less time on prescription renewals, and providing an opportunity for better patient compliance to taking medications. With the additional financial incentives over the next few years to implement e-prescribing programs in healthcare facilities, we should see an enormous growth in the use of electronic prescriptions, and greater benefits should be realized not only in costs but also the quality of healthcare.
References:
1. e-Health Initiative. Electronic Prescribing: Toward Maximum Value and Rapid Adoption. Washington, DC April 14, 2004.
2. Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.
3. Halamka J, Aranow M, Ascenzo C, et al. EPrescribing collaboration in Massachusetts: early experiences from regional prescribing projects. J Am Med Inform Assoc. 2006 May-Jun; 13(3):239-44.
4. Gleason, KM, Groszek JM, Sullivan C. Reconciliation of discrepancies in Medication histories and admission orders of newly hospitalized patients. Am J Health-Syst Pharm. 2004; 61:1689-95.
5. Kilbridge P, Classen D. The informatics opportunities at the intersection of patient Safety and clinical informatics. J Am Med Inform Assoc. 2008; 15:397-407.
6. Dolin RH, Alschuler L, Boyer S, Beebe C, Behlen FM, Biron PV, Shabo Shvo A. HL7 Clinical Document Architecture, release 2. J Am Med Inform Assoc 2006;13(1):30-39.
7. Health Level Seven. HL7 implementation guide: CDA release 2 – Continuity of Care Document (CCD). Ann Arbor, MI: Health Level Seven, Inc., 2007.
8. nlm.nih.gov/research/umls/rxnorm/index.html
9. Liu S, Ma W, Moore R, Ganesan V, Nelson SJ. RxNorm: Prescription for electronic drug information exchange. IT Pro 2005;7(5):17-23.
10. Hamann C, Poon E, Smith S, et al. Designing an electronic medication reconciliation system. AMIA Annu Symp Proc. 2005;976.
11. Grannis SJ, Overhage JM, McDonald CJ. Analysis of Identifier Performance Using a Deterministic Linkage Algorithm. AMIA Annu Symp Proc. 2002:305-9.
12. MedRunner Inc. (2011). e-Prescribing. Retrieved November 22, 2011, from MedRunner
13. American Medical Association. A Clinician's Guide to Electronic Prescribing.RetrievedDecember17,2011, from:
14. a b c d e f g U.S. Department of Health and Human Services. (n.d.). How does e- prescribing work? Retrieved December 17, 2011, from Health Resources and Services Administration: hrsa.gov/healthit/toolbox/Health ITAdoptiontoolbox/ElectronicPrescribing/epreswork.html
15. American College Of Rheumatology. (2011). E-Prescribing. Retrieved December 17, 2011, from Practice Management: rheumatology.org/practice/office/hit/erx.asp
16. Institute of Medicine (2000). To err is human: building a safer health system.
17. a b U.S. Department of Health and Human Services. "The Benefits of Electronic Prescribing".
18. Medicare Program; E-Prescribing and the Prescription Drug Program; Proposed Rule. 70 FR 6256, February 4, 2005
19. Grossman, J. M., Gerland, A., Reed, M. C., & Fahlman, C. (2007). Physicians’ experiences using commercial e-prescribing systems. Health affairs, 26(3), 393- 404.
20. Lasky, M. C., & Keen, S. (2007). An Electronic Subscription Prescription. Intellectual property & Technology Law Journal , 19 (10), 9-11.
21. "Prepare to meet "meaningful use" EMR requirement". American Medical Association..
22. "E-PRESCRIPTION: IMPENDING ACCEPTANCE IN EUROPE". Frost & "Meaningful Use Stage 2 Crib Sheet"Physicians Practice, September 2012.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









