{ DOWNLOAD AS PDF }
ABOUT AUTHOR:
Amitava Sinha Ray
RANBAXY LABORATORIES LTD.
West Bengal, India
a.amitava.s@gmail.com
ABSTRACT:
Diabetes is a major problem across the world also it is a serious problem in India. Diabetes Mellitus is a silent killer of human body. Several types of complication are occurred in diabetic patient. One of the serious complications is Diabetic foot ulcer. Generally occurred due to breakdown in the skin and subcutaneous tissue also muscle. It will be more dangerous if it will become infected. Sometimes it is also needed to cut down the leg by surgery to prevent the spread of infection. A diabetic patient should take care for his foot to avoid this type of complication, also should be more care full to the management of blood sugar in normal level.
INTRODUCTION
An ulcer is defined as a breakdown in the skin that may extend to involve the subcutaneous tissue or even to the level of muscle. These problems are common, particularly on the lower extremities. Leg and foot ulcers have many causes. Diebetic foot ulcer generally causes as a complication of Type-II Diabetes.Also it is caused by Diabetic neuropathy.
First of all we have to know about Diabetes.Diabetes is a chronic disease, which occurs when the pancreas does not produce enough insulin, or when the body cannot effectively use the insulin it produces. This leads to an increased concentration of glucose in the blood (hyperglycaemia). The body is unable to produce or unable to properly use and store glucose (a form of sugar). Glucose backs up in the bloodstream and blood glucose or "sugar" to rise too high. It is a syndrome of impaired carbohydrate, fat, and protein metabolism caused by either lack of insulin secretion or decreased sensitivity of the tissues to insulin. When we take some food there glucose is present, in case of DM due to lack of insulin glucose can’t go in to the cell then glucose level is increased into the blood.DM is totally depend upon the insulin which is secreted from the pancreas specifically from the islet of Langerhans of pancreas.
Type 2 diabetes mellitus, sometimes called age-onset or adult-onset diabetes,is the common form of diabetes mellitus that effects approximately 5% of Americans under the age of 50 and 15% of those 50 and older. More than 90% of the diabetics in the United States have Type 2 diabetes mellitus.[1]
The number diabetic people in world was estimated at 131 million in 2000. It is projected to increase to 366 million by 2030.Diabetic patients have up to a 25% lifetime risk of developing a foot ulcer.The annual incidence of diabetic foot ulcers is ~ 3%.[2]
Foot Ulcer:
Ulcers are breaks in the superficial layers of the skin that are slow or difficult to heal. It may be accompanied by inflammation. Sometimes don't heal and become chronic. Chronic foot ulcers mainly affect the elderly. Especially People with diabetes (Type-II) are at high risk of developing foot ulcers. Foot care must be taken by a diabetic patient. The most common cause of chronic foot ulcers is affected or poor blood circulation in the legs & foot. These ulcers may be due to problems with the arteries or, more commonly with the veins, or to a mixture of both.But diabetes can also directly damage the small blood vessels. A person with diabetes has a much increased risk of developing arterial ulcers. Diabetes directly damages the small blood vessels. Decubitus ulcer-The breakdown and death of skin tissue because of prolonged pressure that interrupts blood flow to the area.[3]

Causes include:
a) Venous leg ulcers: when the veins are unable to supply blood properly, high pressure builds up, damaging the skin which then breaks down into an ulcer[5]
b) Injuries – traumatic ulcers
c) Pressure– Prolonged pressure on the skin that affect the blood supply to one area of skin.
d) Diabetes – Because of poor blood circulation, or loss of sensation (due to diabetes-related nerve damage or diabetic neuropathy) means that pressure on the skin goes unnoticed resulting in pressure ulcer.
e) certain skin conditions
f) Vascular diseases such as atherosclerosis that reduce arterial blood supply to the extremities
g) Infections.
DIABETIC FOOT ULCER:
Diabetic foot ulceris a serious complication of diabetes mellitus. It occurs in 15% of all patients with diabetes and precedes 84% of all diabetes-related lower-leg amputations. Wound healing is an innate mechanism of action that works reliably most of the time.[6] A key feature of wound healing is stepwise repair of lost extracellular matrix(ECM) that forms the largest component of the dermal skin layer.Controlled and accurate rebuilding is essential to avoid under- or over-healing that may lead to various abnormalities. But in some cases, certain disorders or physiological insult disturbs the wound healing process. Diabetes mellitus is one such metabolic disorder that impedes the normal steps of the wound healing process.[6] Many studies show a prolonged inflammatory phase in diabetic wounds, which causes a delay in the formation of mature granulation tissue and a parallel reduction in wound tensile strength. Non-healing chronic diabetic ulcers are often treated with extracellular matrix replacement therapy.
LICENSED CYTOKINES[9]
|
Drug |
Corporation |
Target |
Approval |
|
Regranex®, Becaplermin, rHPDGF-BB |
Ortho-McNeil |
Diabetic neuropathy, foot ulcers |
Dec-97 |
Wound Care for prevention of ulcer:
In general, wounds should be kept clean and moist to promote granulation and prevent infection. Topical therapy alone to heal a wound. It must be stressed that, in most cases, it is adherence to the principles outlined earlier and not what is put on a wound that will lead to a successful result. Wounds resistant to healing, however, may benefit from the many wound care modalities available. Topical growth factors, negative pressure wound therapy, living skin equivalents, and silver-impregnated dressings are among the many adjunctive therapies available for ulcer care.[5]
a) The ulcer should covered with a protective dressing.
b) Clean and re-dress the ulcer regularly.
c) May need to remove any hard skin that prevents the ulcer from healing depending on the site and size of the ulcer.
d) Wearing special shoes for the foot to keep the pressure off the ulcer.
e) Antibiotics will be advised if the ulcer, or nearby tissue, becomes infected.
f) Sometimes a small operation is needed to drain pus and clear dead tissue if infection becomes more severe.
g) In some cases, the arteries in the legs are very narrow and greatly reduce the blood flow to the feet.[5]
Table-1—Information regarding Footwear,General Care and Hygiene[10]
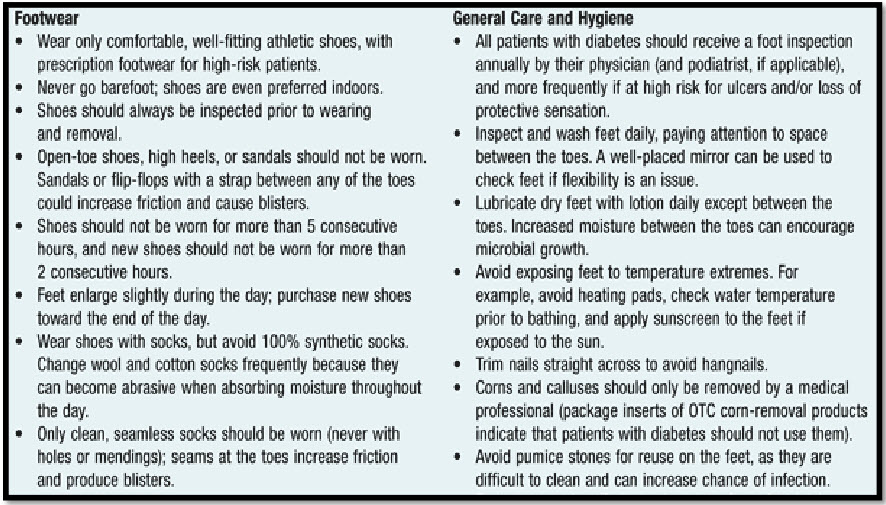
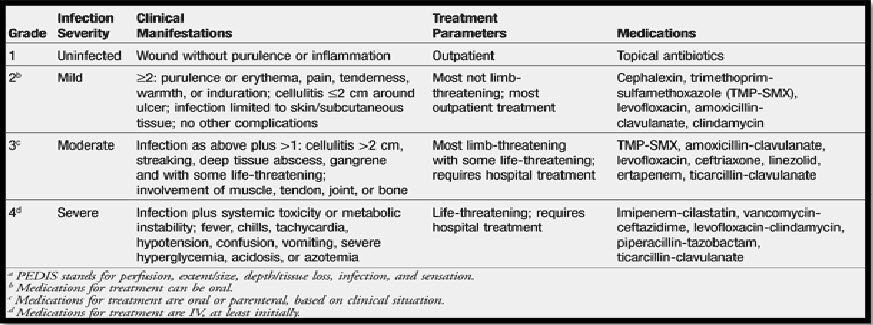
Table-2-Treatment parameter for diabetic foot ulcer[11]
CONCLUSION:
Patients with diabetes are at an increased risk for developing foot ulcerations. The consequences of persistent and poorly controlled hyperglycemia lead to neuropathic and vascular abnormalities that cause foot deformities and ulceration. The feet of diabetic patients should be examined regularly.
If ulcers are present, the treatment strategy should include appropriate dressings. Further, the presence of infections should be determined by clinical findings and appropriate wound cultures and treated based on the culture results. By conducting a periodic foot survey in diabetic patients and incorporating the appropriate basic and specialized care as warranted, the risk of ulceration and its associated morbidities can be reduced.
REFERENCES:
1. PHARMACOLOGY DEMYSTIFIED MARY KAMIENSKI, CEN JIM KEOGH(2006 EDITION)
2. American Diabetes Association. Consensus development conference on diabetic foot wound care. 7-8 April 1999, Boston, Mass Adv Wound Care. 1999, 12: 353-361.
3. Essential of Anatomy and Physiology, Valerie C. Scanlon, Tina Sanders(Fifth Edition 2007)
4. Diabetic Foot Ulcer by Diane Norwood, MS, RD, CDE (beliefnet.com/healthandhealing/getcontent.aspx?cid=102704)
5. A Review of the Pathophysiology, Classification, and Treatment of Foot Ulcers in Diabetic PatientsWarren Clayton, Jr., MD and Tom A. Elasy, MD, MPH
6. Diabetic Foot Ulcers: Pathogenesis and ManagementAm Fam Physician. 2002 Nov 1;66(9):1655-1663.
7. healthylogica.blogspot.in/2012/07/how-to-prevent-onset-of-diabetic-foot.html
8. worldwidewounds.com/2002/may/Vowden/Complex-Foot-Ulcer.html
9. Principles of Immunopharmacology Edited by Frans P. Nijkamp and Michael J. Parnham(2nd revised and extended edition)
10. American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S54.
11. Lipsky BA, Berendt AR, Deery HG, et al. Diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2004;39:885-910.
REFERENCE ID: PHARMATUTOR-ART-2251
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 10 Received On: 11/07/2014; Accepted On: 26/07/2014; Published On: 01/10/2014How to cite this article: AS Ray; Diabetic Foot Ulcer: A Serious Problem for Diabetic Patient; PharmaTutor; 2014; 2(10); 23-26 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









