ABOUT AUTHOR
Abdul Kader Mohiuddin
Department of Pharmacy, World University of Bangladesh
ABSTRACT
Obtaining an accurate medication history, keeping and proper maintenance of patient medical records, tracking medication lists are essential parts of medicine reconciliation and these are the processes where pharmacists play a vital role in. Without all these, prescribers may inadvertently make incorrect decisions about a patient’s treatment, causing harm if previously discontinued medicines are restarted, or if current medicines are omitted or prescribed at the wrong dose for the patient. Medical records are a fundamental part of a physician’s duties in providing patient care. Medical records can contain a wide range of material, such as handwritten notes, computerized records, correspondence between health professionals, lab reports, imaging records, photographs, video and other recordings and printouts from monitoring equipment. Poor record keeping is a major factor in litigation cases brought against healthcare professionals.
Reference Id: PHARMATUTOR-ART-2685

Figure 1. Importance of Thorough Communication on Patient History (Cordant Health Solutions, 2015). According to the online medical website Monthly Prescribing Reference, a communication breakdown between a physician and two of her colleagues contributed to an eventual patient overdose, and resulted in a wrongful death lawsuit against all three providers and several pharmacies. The prescribing physician was eventually dropped from the wrongful death lawsuit, but the case has continued against both previous physicians based on their lack of communication regarding the insurance letters and the patient’s history of doctor shopping – highlighting the importance of complete communication and comprehensive, timely transfer of patient information prior to further prescriptions or other treatments.
INTRODUCTION
Medication histories have traditionally been documented in the ‘Drug history’ section of a physicians’ associates; if pharmacists or nurses identified any errors with this list, they would usually document these in the subsequent progress notes. Erroneous drug histories can lead to discontinuity of therapy, recommencement of ceased medicines, inappropriate therapy and failure to detect a drug-related problem. These errors can have adverse consequences for the patient during their hospital stay. Perpetuation of these errors on discharge may result in adverse events, from duplication of therapy, drug interactions and discontinuation of an essential medicine. Once an accurate medication history has been obtained, this information should be documented in the patient’s medical notes.
Accurate Medication History
Obtaining an accurate medication history is the first step of the medicine reconciliation process. Such histories usually consist of a list of all medicines (prescribed and purchased) that a patient was taking prior to their admission to hospital. Due to the lacking standardization of the medication lists, important information is frequently lacking or—in case of handwritten medication lists—not readable (Taib et.al, 2010; Hartel et.al, 2011). In addition to this, details of allergies or sensitivities to medicines (or excipients), recently stopped medicines (e.g. in the past month), and recent short courses of antimicrobials or corticosteroids should also be included (Harig et.al, 2018). Obtaining an accurate medication history in a pre-operative clinic will allow appropriate suspension of certain medicines (e.g. anticoagulants and antiplatelets) prior to surgery, preventing complications following surgery or the procedure being cancelled (if this information is identified on the day of surgery). There are also many records that are indirectly related to patient management such as accounts records, service records of the staff, and administrative records, which are also useful as evidences for litigation purposes (Nickless et.al, 2016). Medical recording needs the concerted effort of a number of people involved in patient care (Kadam et.al, 2017; WHO, 2006; Al-Bassam et.al, 2016). Documenting the medical history can be lifesaving as well. An encounter with an awake patient who is able to answer all questions which are subsequently recorded on the electronic medical record, could prove to have vital information in the event the patient mental status changes, or during a later encounter if the patient is unable to give their history such as in a traumatic accident (Nichol et.al, 2019). Critically ill adults often have extended hospital lengths of stay and are at high risk of having medication-related adverse events. Between 70% and 95% of clinical records include inaccurate medication lists, and approximately 20% to 30% of all ambulatory patients experience an ADE annually (Bolster, 2019). Potential drug interactions and treatment duplications may result from prescribers being unaware of patients' complete list of home medications (Nester et.al, 2002).
Sources of Medication/Patient History
Patient history simply reveals an idea of his profile, medication behavior, lifestyle, previous history of major/minor surgery, drug hypersensitivity, food habits etc. More often source of history is patient himself. A patient’s social history can provide useful information when reviewing their pharmaceutical care (Macchia et.al, 2015; Regitz-Zagrosek et.al, 2012; Worm et.al, 2015; Shim et.al, 2014). For example, smoking tobacco induces enzymes that speed up the metabolism of theophylline and changes in vitamin K consumption can reduce the efficacy of warfarin. Asking about a patient’s social history also facilitates asking questions about any recreational drug use such as cannabis or ecstasy.
Patients should always be consulted unless it is not physically possible (e.g. they are unconscious or confused). The WHO program Patients for Patient Safety also emphasizes the central role patients should play in efforts to improve the quality and safety of health care (McTier et.al, 2015). A patient’s symptoms and measurements, along with the implications, factors at stake, and potential trade-offs of different management options, are likely to be discussed with family, friends, and peers (Vassilev et.al, 2014). Direct discussion with the patient may also highlight issues with medicines adherence and identify other medicines that the patient uses (e.g. over the counter medicines, herbal medicines or medicines from specialist clinics) (Fitzgerald et.al, 2009). Patients should also be consulted to confirm any previous allergies or intolerances to medicines. Patient participation in medication management during hospitalization has been proposed as a defense against medication errors and as a means of improving patients' adherence to medications once discharged from hospital (Michaelsen et.al, 2015).
Parents and Associates: The validity of parental report was 81% for medication name, 79% for route of delivery, 66% for the form of the medication, and 60% for dose. Parents' report improved on the validity of documentation by physicians across all medication details save for medication name. Parents' report was more valid than nursing documentation at triage for all medication details (Rappaport et.al, 2017).
Previous Surgery Reports provide medicine lists and information on medicines the GP has prescribed for the patient. Another consideration when obtaining information from GPs is the surgery opening hours. Although an increasing number of hospitals have access to patients’ summary care records (SCRs). In Scotland, the SCR contains elements such a patient’s name, address, age, allergies, current medications, diagnoses. It is connected to 100% of general practices, and is automatically updated from existing GP records. Its main objective is to be accessed in emergency and unscheduled care scenarios (Séroussi et.al, 2016). When contacting hospital/GP receptionists, practitioners should remember that these individuals often receive little or no training regarding medicines and it may be more appropriate to obtain a written copy of the medication summary, usually in the form of a fax (Hewitt et.al, 2009).
Previous discharge prescriptions (either filed in the case notes or accessed electronically) may help if a patient has been discharged from hospital recently (i.e. in the past month). However, it must always be confirmed whether there have been any changes to their medications since the previous discharge from hospital. Previous prescription of β-blockers may confer a survival advantage to patients who subsequently develop sepsis with organ dysfunction and who are admitted to an ICU (Macchia et.al, 2012).
Medicine Administration Record (MAR) sheets will often accompany a patient admitted from a nursing or residential home. These should be read carefully to identify any medicines recently started, discontinued, refused or omitted. Extra care should be taken when reviewing MAR sheets with handwritten additions or amendments and those that do not indicate how many pages make up the MAR. Use of the eMAR application significantly reduces the rate of ME-MAR and their potential risk. The main cause of ME-MAR was the failure to follow work procedures (Vicente Oliveros et.al, 2017). Electronic medical administration record (eMAR) systems offer an alternative strategy to study adherence to prescriptions in health care institutions and facilitate efficient review of a large number of drug administration events with no potential for observer effect bias (Dalton et.al, 2015). Errors in preadmission medication histories are associated with older age and number of medications and lead to more discharge reconciliation errors. A recent medication list in the EMR is protective against medication reconciliation errors (Porter et.al, 2005).
Patient medication lists (either repeat prescriptions or self-produced lists) may be brought directly with the patients on admission to hospital. The patient should be asked if this information is up-to-date and whether all parts of the repeat prescription list have been brought in. In Germany, 25–50% of patients with long-term medication have a medication list. An updated and comprehensive medication list may reduce patients' concerns and increase the perceived necessity of their medication. There should be a standard to prepare and providing medication list, otherwise it lacks important information. More often handwritten prescriptions are not completely readable (Jäger et.al, 2015). It is possible that, if patients consulted other physicians or pharmacists for reasons, they think bear no relation to their current visit, they might not report additional drugs without being prompted. For example, a patient might be taking an anti-inflammatory medication for a musculoskeletal disorder but might not think to mention it to a doctor being consulted about hypertension. It is essential to ask patients explicitly whether new medications should be added to the list and to specify the reason for and dosage of the new medications (Lussier et.al, 2007). Patient involvement is essential to maintain accurate and updated medication lists, provide quality care, and decrease potential errors (Chae et.al, 2009).
Community pharmacies are regularly used, with studies reporting that in some regions more than 80% of patients use the same pharmacy for their regular medicines. However, since a patient may visit any community pharmacy, they may not hold an accurate list of all medicines and should not be used as a single source of information. The community pharmacy may provide information on compliance aids or medicines that are not supplied on a repeat prescription from the GP, such as methadone or medicines obtained from a memory clinic. Community pharmacies may also be able to give information when other sources are unavailable (e.g. methadone doses when the community drug service is closed) (Nickless et.al, 2016).
Specialist clinics may also hold additional medicines information, so GPs may not have information about medicines that they do not prescribe. The patient’s medical history may suggest that they receive medicines via another prescriber (e.g. donepezil from a memory clinic, antiretrovirals from an HIV clinic, or methadone from a community drug service) (Nickless et.al, 2016).
Care transition & Medication Errors (MEs)
Transition of care on admission to the hospital and between clinical areas are risk points for medication errors. All type of medication errors can be reduced by improving communication at each transition point of care. Medication histories are often recorded inaccurately by physicians at the time of hospital admission (Mazhar et.al, 2018). Even one third of prescribing errors that occur in hospitals are a consequence of an incorrect medication history taken at the time of admission (Boostani et.al, 2019; Petrov et.al, 2018). Studies have shown that for 50 to 70% of admitted patients, the initial medication history contains at least one error (Schepel et.al, 2019). In a recent similar study, a nearly 90% of the patients experienced at least one ME during their hospital stay which is lower than reported MEs rates by other studies in patients admitted to internal wards (Boostani et.al, 2019; Petrov et.al, 2018). Approximately half of all hospital medication errors and one third of ADEs occur as a result of miscommunication at interfaces of care (Petrov et.al, 2018; Almanasreh et.al, 2016). In addition, almost 60% of MEs occur at admission, transfer, or discharge from the hospital (Abu Farha et.al, 2018). The average ME rate was 1.5 errors per patient at admission and 1.3 at discharge. Medication-related problems (MRPs) are common among home care patients who take many medications and have complex medical histories and health problems. In the case of older adults, ADRs contribute to already existing geriatric problems such as falls, urinary incontinence, constipation, and weight loss (Mohiuddin et.al, 2019). However, the most common MEs were omissions, wrong dose and frequency, and inappropriate added medications. More than 35% of patients experienced serious or very serious MEs and almost 40% potentially moderate MEs (Breuker et.al, 2017). ADEs are a major cause of morbidity and mortality, with more than 50% of ADEs being preventable (Naicker et.al, 2018). A thorough and accurate admission medical record is an important tool in ensuring patient safety during the hospital stay (Amirian et.al, 2014). Inaccurate medication history at admission to hospitals leads to preventable ADEs, which in turn increase mortality, morbidity, and health care costs (McShane et.al, 2018).
Medication Discrepancies
Medication discrepancies are unintended differences between a patient's outpatient and inpatient medication regimens. The rate of discrepancy of medications is estimated to be between 38% and 50% for newly hospitalized patients (Abuyassin et.al, 2011). Penm et.al, 2019 reported that medication discrepancies occur in up to 80% of hospitalized patients during transitions of care, either at admission or discharge. They affect up to 60% of patients admitted to hospital (Stockton et.al, 2017). Older patients are especially at risk, as polypharmacy, comorbidities, and longer hospital stays are associated with increased MEs. Furthermore, it has been shown that incomplete medication lists at admission can result in medication errors at discharge (Graabæk et.al, 2019). Insight into potential risk factors associated with these discrepancies would be helpful to focus the second medication reconciliation on high-risk patients (Ebbens et.al, 2018). Patient history data from electronic medical record (EMR) may not accurately represent a patient’s full prescription drug profile. An infrastructure to provide medication history services appears essential (Frisse et.al, 2010). In the patient’s eyes, the ability to communicate well forms a major component of a provider’s clinical competence. The ability to communicate effectively with patients can contribute significantly to improved patient outcomes (Berman et.al, 2016).
Keeping Medical Records
A modest relationship exists between the quality of medical-record keeping and patient perception of hospital care (Dang et.al, 2014). The nursing assessment includes gathering information concerning the patient's individual physiological, psychological, sociological, and spiritual needs. It is the first step in the successful evaluation of a patient (Toney-Butler et.al, 2019). Some studies conducted in the United States, India, and Brazil also reported that history-taking was responsible for nearly 80% of all diagnoses made and that investigations played complementary roles in excluding other diagnostic options and increased physicians’ self-confidence (Benseñor et.al, 2004; Roshan et.al, 2000; Peterson et.al, 1992). Additionally, a less equipped primary health care center may still arrive at a correct diagnosis in about 88% of cases following brief history-taking and physical examination, and treatment can be commenced based on these findings (Oyedokun et.al, 2016). Clinical record keeping is an integral component in good professional practice and the delivery of quality healthcare. Consequently, clinical records should be updated, where appropriate, by all members of the multidisciplinary team that are involved in a patient’s care (physicians, surgeons, nurses, pharmacists, physiotherapists, occupational therapists, psychologists, chaplains, administrators or students) (Mathioudakis et.al, 2016).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Effective Patient Communication and Physical Exam Skills
Gathering sufficient medical data from a patient’s history and empathetic communication are two completely separate sides of the coin of history taking (Ohm et.al, 2013). According to the Nobel Peace laureate Bernard Lown medical history provides sufficient information in about 75% of patient encounters to make the diagnosis before performing a physical examination and additional tests (Lown, 1999). Poor physical exam skills are a noteworthy threat to patient safety as they can lead to incorrect as well as missed diagnoses, causing delays in timely implementation of life-saving treatments (Asif et.al, 2017). Again, Patient history and physical examination cannot be used to limit the need of a diagnostic block (Maas et.al, 2017). Chronic medication is often temporarily stopped at the ICU. Unfortunately, when the patient improves, the restart of this medication is easily forgotten. Moreover, temporal ICU medication is often unintentionally continued after ICU discharge (Bosma et.al, 2018). Medical records include a variety of documentation of patient's history, clinical findings, diagnostic test results, preoperative care, operation notes, post-operative care, and daily notes of a patient's progress and medications (Thomas et.al, 2009). A properly obtained consent will go a long way in proving that the procedures were conducted with the concurrence of the patient (Kadam et.al, 2017). Medical records form an important part of the management of a patient. A properly written operative note can protect a surgeon in case of alleged negligence due to operative complications (Pandit et.al, 2009). Medical recording needs the concerted effort of a number of people involved in patient care. The doctor is the prime person who has to oversee this process and is primarily responsible for history, physical examination, treatment plans, operative records, consent forms, medications used, referral papers, discharge records, and medical certificates (Mathioudakis et.al, 2016; Kadam et.al, 2017). Hypersensitivity reactions, ADRs and all forms of complementary and alternative medicine (CAM) are often poorly documented or not explored in detail, which may lead to unnecessary avoidance of a drug (Shenfield et.al, 2001; Cockayne et.al, 2005; Fitzgerald et.al, 2009).
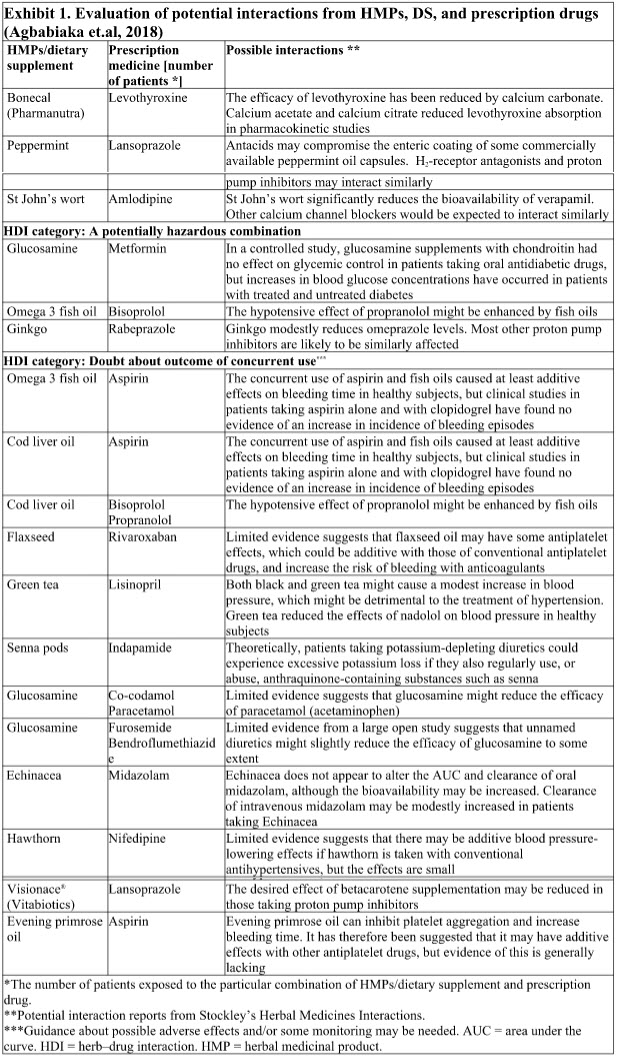
OTC/Herbal medications
Once the prescribed medications have been added to the list, physicians must ask their patients explicitly whether they take OTC, particularly “CAM” products. Patients might have decided to take these on their own and might not necessarily think them worth reporting. Often these nonprescription choices are unknown to health care practitioners and thus are often not included as part of patients' health records. The exclusion of these therapies can pose risks to patient safety. There is a significant need to address the capture of OTC medication use in both the physician and pharmacy electronic health records (EHRs) and during the practitioner-patient medication history and reconciliation process. Green tea showed 85% decrease in plasma concentration of nadolol, for example (Awortwe et.al, 2019). Although some patients may not consider these as medicines, their use is fairly common – a review of published surveys identified an average prevalence rate of 37% (Posadzki et.al, 2013). This result in herb or herb-drug interaction induced unfavorable clinical outcomes without crucial documentation on their temporal relations and concomitant use. Herb-drug interaction related morbidity is thus an emerging serious public health issue with broad implications for clinicians, pharmaceutical industries and health authorities (Parvez et.al, 2019).
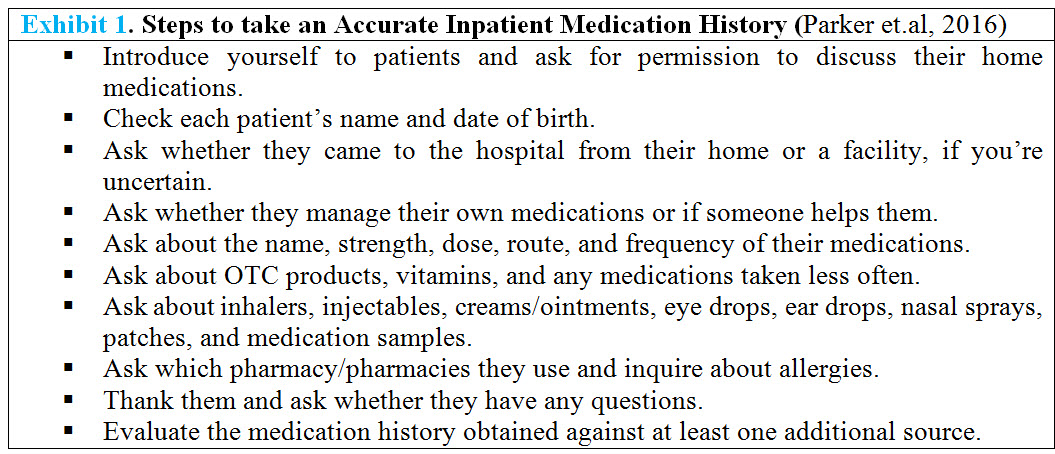
Pharmacy Personnel-led Patient History & Medical Record Keeping
A pharmacy personnel-based medication history program in the ICU is feasible and assists in the discovery of medication discrepancies with the potential for patient harm (Kram et.al, 2019). Obtaining an accurate medication history is an essential part of medicine reconciliation and a process that pharmacists play a vital role in (Nickless et.al, 2016). Several studies show that pharmacists, pharmacy technicians and pharmacy students have all demonstrated improved accuracy in completing the home medication history (Petrov et.al, 2018; Bowman et.al, 2017). Both pharmacists and trained pharmacy technicians were significantly superior to the other Allied Health Professionals (AHPs) in terms of unintentional discrepancies and success index for medication reconciliation (Johnston et.al, 2010). Pharmacists-acquired medication histories are often free of error of commission, omission and more frequently document past prescription/ OTC medicines, allergy history and use of alcohol (Fitzgerald et.al, 2009; Yusuff et.al, 2010). Pharmacy technicians are supervised by pharmacists, using a defined accountability plan based on a set of medical staff approved rules for what medications comprise a best possible medication history. Medication history accuracy and completeness rates have been consistently over 90% and rates of provider compliance with medication reconciliation rose from under 20% to 100% since medication history program implementation (Cooper et.al, 2014). Medication histories have traditionally been documented in the ‘Drug history’ section of a doctor’s clerking; if pharmacists identified any errors with this list, they would usually document these in the subsequent progress notes (Bolster, 2019). Any redistribution of duties has potential problems. If nurses feel that pharmacists' desire to provide this service stemmed from the belief that nurses were doing it inadequately, they might feel alienated or insulted. On the contrary, the nursing staff strongly supported the prospect of pharmacists' role and expertise in conducting medication history interviews (Nester et.al, 2002). The aptitude of a patient as a historian of medications can vary depending on a multitude of factors, including but not limited to physical condition upon ED admission. Some patients have their medications managed by a facility or family member, while others come in with bottles of their medications. Even when these puzzle pieces are presented, however, they must be reviewed with a discerning eye given to dates, dosage regimens, and details (Hughes, 2016). Accurate history collection is integral to medication reconciliation. Also, Pharmacist involvement in ED medication reconciliation leads to time savings during the admission process (Chhabra et.al, 2018).
Throughout the information-gathering process, physicians must try to foster patients’ participation. They should also take time to ask whether patients are having any problems with their drug regimens. If they are, physicians should work with them to try to find concrete solutions adapted to their particular circumstances. At this point in the interview, physicians should also inquire explicitly whether their patients have noticed any ADRs that they associate with the medications (Lussier et.al, 2007). Medication lists and structured medication counselling (SMC) including “brown bag reviews” (BBR) are important instruments for medication safety. Medication errors are the most common preventable cause for these undesired events and comprise the prescribing, dispensing, and administration of the medicine (Jäger et.al, 2015).
Data to be obtained during Medication History Interview
Previous Medication: The medication history should not be restricted to current therapies that a patient is taking – include any recently stopped or changed medicines (Royal Pharmaceutical Society Great Britain, 2011). Patients may not be able to remember the names of all their medications. If this is the case, obtain a detailed description of each medication, including the dosage form (e.g., tablet, capsule, liquid, topical formulation); size, shape, and color of the dosage form; and any words, letters, and numbers on the dosage form that the patient can remember or that can be seen on the dosage form. If the patient cannot remember the dosage of the drug, the pharmacist may be able to identify the drug and/or dosage from other details the patient provides. However, clearly document the patient’s description and note that the medication might be a specific product. Example: The patient cannot remember the name of the medication but describes it as a purple capsule with yellow rings around the capsule. This description is consistent with Nexium (esomeprazole) 40 mg. The medication history is an important document for communication among pharmacists and between pharmacists and other health care professionals. Many physicians, nurses, and other health care professionals typically know the proprietary (trade) name of the medication but are less familiar with the nonproprietary (generic) medication names (Summers et.al, 2017). Therefore, when a patient identifies a medication by the proprietary name, document both the proprietary and nonproprietary names. If the patient identifies a medication by the nonproprietary name, document the nonproprietary name. For combination medications, document the nonproprietary names of all active ingredients in the combination product. Example: Lanoxin (digoxin) 0.25 mg orally once daily. Example: Ibuprofen 200 mg orally every 4 to 6 hours prn headache. Example: Tylenol with Codeine No. 3 (acetaminophen 300 mg, codeine 30 mg) 1-2 tablets every 4 hours prn pain.
PRN Medications: For as needed (prn, on demand) prescription and nonprescription, document the possible use as well as the patient’s actual use of the medication. Quantification is important; do not accept imprecise descriptive terms. For example, the term occasional may mean anything from one dose of the medication every few months to one or more doses per day depending on the patient. Patients may or may not be able to describe their frequency of use but may be able to describe how often they get the prescription refilled or buy a new supply of nonprescription medication; both give an indirect indication of frequency of use. One approach to quantifying the amount of medication actually consumed by the patient is to inquire how often the patient has to obtain a new supply of the medication. Example: Acetaminophen 325-650 mg every 4 to 6 hours as needed for headache for 50 years. The patient takes one to two doses per month; very effective. Last taken 2 weeks ago. The patient buys a small bottle of acetaminophen about once a year.
Dietary Information: Dietary information includes specific dietary restrictions and any supplements, stimulants, or depressants used. For example, patients with diabetes may follow a reduced-carbohydrate diet; other patients may be consuming recommended or self-imposed low-fat, low-sodium, low-calorie, low-fiber, or high-fiber diets. The majority of clinically relevant food-drug interactions are caused by food-induced changes in the bioavailability of the drug. Patients taking warfarin are at particular risk of interactions with dietary supplements, yet approximately 30% use herbal or natural product supplements on a regular basis. Patients placed on anti-hypertensive drugs will benefit from concomitant moderate sodium restricted diets. Propranolol serum levels may be increased if taken with rich protein food (Bushra et.al, 2011)
Social Habits: Social habits include the use of tobacco, alcohol, and illicit drugs. Document the duration of use, amount of each agent consumed, frequency of use, and reasons for use of each agent without being judgmental. Determine the type, quantity, pattern, and duration of alcohol use. Alcohol intake can increase risk of liver damage or stomach bleeding. Smoking may decrease propranolol plasma levels of by increasing its metabolism (Simpson et.al, 2019; Maideen et.al, 2019). To assess tobacco use, note at what age the patient first started smoking tobacco and when the patient quit smoking (if applicable). Because the effects of smoking on drug metabolism may be clinically important for weeks to months after the patient has stopped smoking, note approximately when the patient stopped smoking. Pharmacists in acute care settings should be especially sensitive to these issues. Patients often quit smoking just before hospitalization and may consider themselves nonsmokers when asked about their smoking habits. Non-disclosure of DS is even higher among racial and ethnic minorities. Barriers in medical encounters may not facilitate disclosure of DS use. Lack of DS disclosure, particularly of self-care practices among minority populations, represents a serious challenge for medical encounter communications. As the use of DS gains popularity among prescription medication users and patients with chronic conditions, there is concern that medical providers may miss diagnosis or make a medical prescribing error (Gardiner. Et.al, 2015)
Concurrent Prescription Medications: The medication history in the hospital medical record is often incomplete, as 25% of the prescription drugs in use are not recorded and 61% of all patients have one or more drugs not registered (Wang et.al, 2012). It is important to obtain a complete list of the patient’s current prescription medications, including the name and dosage of the drug, dosing schedule (prescribed and actual), duration of therapy (start date), reason the patient is taking the medication, and outcome of therapy. Patients sometimes change dosing schedules to fit their work schedules and lifestyles or to conserve medication to reduce the expenses of long-term medications. Determine when the patient started taking the prescription medication and the reason the patient gives for taking the medication. Exact dates are important in determining whether an adverse or allergic reaction is a result of a specific medication and whether the prescribed medication is effectively treating or controlling a specific condition. For example, a patient with elevated blood pressure may claim to adhere to his or her blood pressure medication regimen yet still have elevated blood pressure. The decision to continue or discontinue the medication depends on when the patient started the current regimen. The regimen would continue unchanged if the patient had just started the medication the previous week but would need to be changed if the patient had been taking the medication for 2 months. Some patients may not know the specific reason they are taking their medications because they forgot or misunderstand the reason it has been prescribed. Document the reasons the patient gives for taking the medication and clarify any discrepancies regarding customary uses of medications with the prescriber, not the patient (Patel et.al, 2013; Samaranayake et.al, 2018). Example: Hydrochlorothiazide (Esidrex) 50 mg daily for 5 years for high blood pressure. The patient reports that her blood pressure has been well controlled with this regimen. Example: The patient takes a small oblong pink tablet twice daily for treatment of high blood pressure. The patient cannot remember the name of the medication or when she started taking it. The patient doesn’t think it works very well because her blood pressure is always high.
Current Non-Prescription Medications: Obtain a complete description of current nonprescription medications from the patient. Document the name and dosage of the drug, recommended and actual dosing schedule, dates and duration of therapy, reason the patient is taking the medication, and outcome of therapy. Knowledge of current nonprescription medications allows the pharmacist to determine whether drug interactions may occur between prescribed and self-administered medications, whether the patient is self-medicating to relieve an adverse drug reaction from a prescribed medication or in an attempt to obtain better relief from symptoms than that provided by the prescribed regimen, and whether a nonprescription medication is the cause of a patient’s complaint or is exacerbating a concurrent medical condition (Ansari et.al, 2010; Kim et.al, 2018; Shetty et.al, 2018). Example: The patient is currently using bacitracin ointment on a cut on his finger. He washes the cut with soap and water and applies a thin layer of bacitracin to the cut twice a day. He started using the bacitracin ointment 2 days ago when he accidentally cut himself. The wound is healing well. Current and Past Complementary and Alternative Medicines: Use of complementary and alternative medicine (CAM) in the US is prevalent, with over one-third of adults reporting CAM use in 2012 (e.g., herbal remedies, megavitamins, homeopathic medicine, folk remedies) (Johnson et.al, 2015). However, the majority of people do not discuss these therapies with their physicians. Many of these medicines interact with traditional medicines. Some have significant side effects. Therefore, it is important to document the use of these medicines. Obtain a complete description of current and past alternative medicine use (Bent et.al, 2008; Tachjian et.al, 2010). Document the name and dosage of the product, dosing schedule, duration of therapy, reason the patient is taking the product, start and stop dates or approximate duration and timing of use, and outcome of therapy. Ask the patient follow-up questions to clarify why the patient is taking the alternative medicine. For example, if a patient state that he or she is taking an alternative medicine to boost the immune system, ask the patient whether anyone has ever told the patient that he or she has a weakened immune system and whether the patient gets more infections than most people. As with many prescription and nonprescription medications, many alternative remedies are taken prn. Quantification of the exact amount of product consumed by the patient may be difficult. Common herbal remedies that produce adverse effects on the cardiovascular system include St. John’s wort, motherwort, ginseng, gingko biloba, garlic, grapefruit juice, hawthorn, saw palmetto, danshen, echinacea, tetrandrine, aconite, yohimbine, gynura, licorice, and black cohosh (Tachjian et.al, 2010; Cohen et.al, 2010; Ronis et.al, 2018). A study of 25 available ginseng products found a 15- to 200-fold variation in the concentration of 2 ingredients believed to have biological activity: ginsenosides and eleuthrosides.8 Therefore, it may be difficult for patients to ascertain with certainty the precise contents of the products they may be interested in taking. Two case reports suggest a possible increase in the risk of bleeding with garlic use (Bent et.al, 2008).
Past Nonprescription Medications: Obtain as much information as possible about past nonprescription medications, including name and description, dosage, prescribed or recommended and actual dosing schedule, dates and duration of therapy, reason for taking, reason for stopping, and outcome. Knowledge of past nonprescription regimens gives the pharmacist insight regarding past medical problems or attempts to treat current medical problems. As with prescription medications, patients are unlikely to remember all of these details for past medications. Document the details the patient can remember; avoid excessive “grilling” of the patient. OTC drugs are not currently considered by many clinicians to be medications, and thus are often not included in the medication record. As interactions can occur between prescribed medication, over-the-counter medications, or dietary supplements, all medications and supplements should be part of a patient’s medication history and included in the reconciliation process (Tesfamariam et.al, 2019). Lau et.al, 2000 compared community pharmacy drug lists with hospitalized patients and found 25% of prescription drugs in use at home were not recorded on the hospital admission record. Some of the patient’s daily medications may be discontinued during a hospital stay, and when there is a lack of a formal reconciliation process on discharge, the need to restart medications upon discharge may be overlooked. One example would be discontinuing an anticoagulant during a hospital stay and neglecting to restart it upon discharge. Another example is when orders from one unit of care (such as ICU) are discontinued and new orders are written when the patient moves to another unit of care (such as a general care unit) (Bonaudo et.al, 2018)
Immunizations: Vaccinations are important for the health of individuals and the public. The Centers for Disease Control and Prevention (CDC) immunization recommendations are complex and difficult for an individual patient to understand. Traditionally, patients have relied on their primary care providers to maintain their immunization records, but now that all 50 states allow certified licensed pharmacists to vaccinate patients, pharmacists can provide this service. This increases the importance of the pharmacist’s obtaining and maintaining an accurate immunization record as part of the medication history. Current pediatric immunization schedules include the administration of several vaccines simultaneously, therefore increasing the potential for immune interference (both positively and negatively) to the antigens administered. This has been termed bystander interference and may influence responses to non-conjugated antigens administered simultaneously, or even sequentially. The mechanism suggested for this interference is competition for limited resources within the lymph nodes (Harig et.al, 2018). Caution should be used when administering a vaccine to a child with an acute moderate to severe illness, with or without a fever (Informed Health Online, 2017).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Medication Allergies: People who have a drug allergy are often no longer sure which medications they can take, and which medications they can’t take. Immediate allergic reactions can be treated using steroids or antihistamines. More severe reactions are treated with adrenaline (epinephrine) injections and steroids. Sometimes people have to take a medication that they are allergic to – such as a medication for cancer or a serious infection – because there are no alternatives (Willeboordse et.al, 2014). Many physicians, nurses, and other health care professionals as well as patients may be unable to differentiate between a drug allergy and an adverse drug reaction. But it is very important to try to distinguish between the two reactions. Once a medication allergy is documented for a patient, it is highly unlikely that the patient will receive the medication or a similar medication again. Drug-induced allergic reactions include anaphylaxis, contact dermatitis, and serum sickness. Tripp et al. found documented allergies reported 28% after a pharmacist-conducted patient interview. There is an increased chance of medication error if allergy details are not properly documented. Lack of details surrounding an allergic reaction, especially severe reactions, may cause an allergy to be overlooked or the severity underestimated. Inaccurate or incomplete information about a patient’s drug allergies may also result in a change in drug therapy for the patient that may be unnecessary or is less tolerated (Kim t.al, 2017). Example: The patient is allergic to penicillin. The patient had an itchy rash over his whole body after taking a couple of doses of penicillin 20 years ago. His doctor told him to stop taking the medication and that he was allergic to the drug. He remembers taking some kind of oral medication that stopped the itching but doesn’t remember the name of that medication. He has not taken penicillin since that episode.
Concurrent ADRs: ADRs include drowsiness from first-generation antihistamines, constipation from codeine-containing medications, nausea from theophylline, and diarrhea from ampicillin. The patient may identify some adverse drug reactions during the discussion of medication allergies. A total of 1841 cases were analyzed in Korean Children with complex chronic conditions (CCC), among which 68.3% were mild, 26.8% moderate, and 4.9% cases were severe. Hence, clinicians need to be aware of the common types of ADRs and the management of serious ADRs and should be vigilant upon their occurrence. In cases of severe ADRs, these are more frequently observed in vulnerable groups such as CCCs and younger children, especially in the infants/toddler group (Lam et.al, 2015). Example: The patient felt dizzy and had strange dreams after taking one dose of Darvon (propoxyphene) 10 years ago for pain after some dental work. He threw out the rest of the prescription and has not taken Darvon since then.
Adherence: WHO reported that adherence among patients with chronic diseases averages only 50% in developed countries. One of the goals of the medication history interview is to determine whether the patient is adherent to prescribed or recommended medication regimens. Knowledge regarding patient adherence is useful in evaluating the effectiveness of prescribed or recommended medication regimens. Medications may be ineffective if the patient does not comply with the prescribed or recommended regimen. Nonadherence may result in additional diagnostic evaluations, procedures, hospitalizations, and unnecessary combination medication regimens. While noncommunicable and mental illnesses are expected to exceed 65% of the global burden of disease in 2020, approximately 50%–60% of patients are nonadherent to the medicine that they have been prescribed, especially those suffering from chronic diseases. As a result, more than 30% of medicine-related hospital admissions occur due to medication nonadherence (Wang et.al, 2018). Medication non-adherence has been reported in over 60% of patients with CVD, the leading cause of morbidity and mortality worldwide. Medication non-adherence contributes to poor achievement of treatment goals, increased patient morbidity and mortality, and an estimated cost of $564 billion in 2012 to $637 billion in 2015 (Toich, 2016; Mack, 2016)). healthcare expenditures. According to the Office of the National Coordinator for Health IT (ONC), approximately 74% of physicians have adopted certified EHR systems. However, approximately 51% of physicians are only using basic EHR functionalities, such as inputting patient demographic information. EHRs also introduce work-flow disruptions for clinical staff that have been shown to lead to productivity losses of up to 20% in internal medicine clinics within the first month of implementation. These studies illustrate that EHRs are not yet being used to their greatest potential (Jonikas et.al, 2012). Sympathetic confrontation may help the pharmacist obtain information regarding patient adherence. Patients are more likely to be truthful when describing their difficulties with complying with the medication regimen if the pharmacist acknowledges that the dosage regimen is complex and difficult to follow and that taking medication regularly is hard. Pharmacies use prescription-filling data to target poor adherers with programs aimed at reducing gaps in medication possession, including mail order programs with refill reminders through email, phone or text, proactive interactive phone calls, counseling by pharmacists, and education on adherence for pharmacists (Pourrat et.al, 2014). Example: The patient is nonadherent. She admits that she picks and chooses which medication to take and that she takes the medications the way she wants to, not as prescribed. Example: The patient is adherent. He knows the names and descriptions of all of his medications and is able to describe his usual routine for taking the medications. He says his wife helps him remember to take the medications.
Conclusion
The clinical pharmacists were able to identify the patients with clinically relevant drug-related problems by using the agreed criteria. Communicating the patient's medical history to other medical professionals is important and can have significant implications in preventing medical errors. When recording the patient's medical history in the chart, accuracy may reduce medical errors or improper diagnoses. An accurate medical history will cross through all aspects of the interdisciplinary team involved in the care of the patient. Though there is no single way to eliminate all drug errors, healthcare workers can reduce the errors by becoming more cautious and interacting closely with other practitioners, pharmacists, and patients. Open and direct communication is one way to bridge the safety gap. Clinical records are also valuable documents to audit the quality of healthcare services offered and can also be used for investigating serious incidents, patient complaints and compensation cases. Everyone responsible for using data has to make sure the information is used fairly, lawfully and for limited, specifically stated purposes in a way that is adequate, accurate, relevant and not excessive. It is not only medical notes that are important; well-written medical records will provide qualitative comment on treatment outcomes.
REFERENCES
1. Ansari J. Drug interaction and pharmacist. J Young Pharm. 2010 Jul;2(3):326-31. doi: 10.4103/0975-1483.66807. PubMed PMID: 21042495; PubMed Central PMCID: PMC2964764.
2. Agbabiaka TB, Spencer NH, Khanom S, Goodman C. Prevalence of drug-herb and drug-supplement interactions in older adults: a cross-sectional survey. Br J Gen Pract. 2018 Oct;68(675):e711-e717. doi: 10.3399/bjgp18X699101. PubMed PMID: 30249608; PubMed Central PMCID: PMC6145997.
3. Almanasreh E, Moles R, Chen TF. The medication reconciliation process and classification of discrepancies: a systematic review. Br J Clin Pharmacol. 2016 Sep;82(3):645-58. doi: 10.1111/bcp.13017. Epub 2016 Jun 29. Review. PubMed PMID: 27198753; PubMed Central PMCID: PMC5338112.
4. Abu Farha R, Abu Hammour K, Al-Jamei S, AlQudah R, Zawiah M. The prevalence and clinical seriousness of medication discrepancies identified upon hospital admission of pediatric patients. BMC Health Serv Res. 2018 Dec 14;18(1):966. doi: 10.1186/s12913-018-3795-1. PubMed PMID: 30547782; PubMed Central PMCID: PMC6295069.
5. Amirian I, Mortensen JF, Rosenberg J, Gögenur I. Admission medical records made at night time have the same quality as day and evening time records. Dan Med J. 2014 Jul;61(7):A4868. PubMed PMID: 25123118.
6. Abuyassin BH, Aljadhey H, Al-Sultan M, Al-Rashed S, Adam M, Bates DW. Accuracy of the medication history at admission to hospital in Saudi Arabia. Saudi Pharm J. 2011 Oct;19(4):263-7. doi: 10.1016/j.jsps.2011.04.006. Epub 2011 May 7. PubMed PMID: 23960767; PubMed Central PMCID: PMC3745046.
7. Asif T, Mohiuddin A, Hasan B, Pauly RR. Importance Of Thorough Physical Examination: A Lost Art. Cureus. 2017 May 2;9(5):e1212. doi: 10.7759/cureus.1212. PubMed PMID: 28589061; PubMed Central PMCID: PMC5453739.
8. Awortwe C, Bruckmueller H, Cascorbi I. Interaction of herbal products with prescribed medications: A systematic review and meta-analysis. Pharmacol Res. 2019 Mar;141:397-408. doi: 10.1016/j.phrs.2019.01.028. Epub 2019 Jan 17. Review. PubMed PMID: 30660822.
9. Al-Bassam SM. Misconduct in Medical Records Documentation of Patients Admitted to Surgical Department at Basrah General Hospital. A Cross Sectional Study Of 250 Medical Records. Bas J Surg, June, 22, 2016. Available From: https://www.iasj.net/iasj?func=fulltext&aId=111179
10. Bowman C, McKenna J, Schneider P, Barnes B. Comparison of Medication History Accuracy Between Nurses and Pharmacy Personnel. J Pharm Pract. 2019 Feb;32(1):62-67. doi: 10.1177/0897190017739982. Epub 2017 Nov 6. PubMed PMID: 29108459.
11. Breuker C, Macioce V, Mura T, Castet-Nicolas A, Audurier Y, Boegner C, Jalabert A, Villiet M, Avignon A, Sultan A. Medication Errors at Hospital Admission and Discharge: Risk Factors and Impact of Medication Reconciliation Process to Improve Healthcare. J Patient Saf. 2017 Sep 4. doi: 10.1097/PTS.0000000000000420. [Epub ahead of print] PubMed PMID: 28877049.
12. Berman AC, Chutka DS. Assessing effective physician-patient communication skills: "Are you listening to me, doc?". Korean J Med Educ. 2016 Jun;28(2):243-9. doi: 10.3946/kjme.2016.21. Epub 2016 Feb 25. PubMed PMID: 26913771; PubMed Central PMCID: PMC4951737.
13. Bent S. Herbal medicine in the United States: review of efficacy, safety, and regulation: grand rounds at University of California, San Francisco Medical Center. J Gen Intern Med. 2008 Jun;23(6):854-9. doi: 10.1007/s11606-008-0632-y. Epub 2008 Apr 16. Review. PubMed PMID: 18415652; PubMed Central PMCID: PMC2517879.
14. Benseñor IM. Do you believe in the power of clinical examination? The answer must be yes! Sao Paulo Med J. 2003 Nov 6;121(6):223. Epub 2004 Jun 28. PubMed PMID: 14989136.
15. Bonaudo M, Martorana M, Dimonte V, D'Alfonso A, Fornero G, Politano G, Gianino MM. Medication discrepancies across multiple care transitions: A retrospective longitudinal cohort study in Italy. PLoS One. 2018 Jan 12;13(1):e0191028. doi: 10.1371/journal.pone.0191028. eCollection 2018. PubMed PMID: 29329310; PubMed Central PMCID: PMC5766134
16. Bolster L. Technician Medication Reconciliation in Primary Care Is An Overlooked Opportunity. Pharmacy Times® January 28, 2019
17. Boostani K, Noshad H, Farnood F, Rezaee H, Teimouri S, Entezari-Maleki T, Najafiazar R, Hassanpouri-Olia A, Gharekhani A. Detection and Management of Common Medication Errors in Internal Medicine Wards: Impact on Medication Costs and Patient Care. Adv Pharm Bull. 2019 Feb;9(1):174-179. doi: 10.15171/apb.2019.020. Epub 2019 Feb 21. PubMed PMID: 31011571; PubMed Central PMCID: PMC6468220.
18. Bushra R, Aslam N, Khan AY. Food-drug interactions. Oman Med J. 2011 Mar;26(2):77-83. doi: 10.5001/omj.2011.21. PubMed PMID: 22043389; PubMed Central PMCID: PMC3191675.
19. Bosma LBE, Hunfeld NGM, Quax RAM, Meuwese E, Melief PHGJ, van Bommel J, Tan S, van Kranenburg MJ, van den Bemt PMLA. The effect of a medication reconciliation program in two intensive care units in the Netherlands: a prospective intervention study with a before and after design. Ann Intensive Care. 2018 Feb 7;8(1):19. doi: 10.1186/s13613-018-0361-2. PubMed PMID: 29417295; PubMed Central PMCID: PMC5803169.
20. Chae SY, Chae MH, Isaacson N, James TS. The patient medication list: can we get patients more involved in their medical care? J Am Board Fam Med. 2009 Nov-Dec;22(6):677-85. doi: 10.3122/jabfm.2009.06.090059. PubMed PMID: 19897697.
21. Cordant Health Solutions. Patient Overdose Underscores Importance of Thorough Communication on Patient History. Web cordantsolutions, September 10, 2015.
22. Cohen PA, Ernst E. Safety of herbal supplements: a guide for cardiologists. Cardiovasc Ther. 2010 Aug;28(4):246-53. doi: 10.1111/j.1755-5922.2010.00193.x. Review. PubMed PMID: 20633025.
23. Cockayne NL, Duguid M, Shenfield GM. Health professionals rarely record history of complementary and alternative medicines. Br J Clin Pharmacol. 2005 Feb;59(2):254-8. PubMed PMID: 15676051; PubMed Central PMCID: PMC1884759.
24. Cooper JB, Lilliston M, Brooks D, Swords B. Experience with a pharmacy technician medication history program. Am J Health Syst Pharm. 2014 Sep 15;71(18):1567-74. doi: 10.2146/ajhp130590. PubMed PMID: 25174017.
25. Chhabra A, Quinn A, Ries A. Evaluation of Time Spent by Pharmacists and Nurses Based on the Location of Pharmacist Involvement in Medication History Collection. J Pharm Pract. 2018 Jan 1:897190017753783. doi: 10.1177/0897190017753783. [Epub ahead of print] PubMed PMID: 29357729.
26. Dang VM, François P, Batailler P, Seigneurin A, Vittoz JP, Sellier E, Labarère J. Medical record-keeping and patient perception of hospital care quality. Int J Health Care Qual Assur. 2014;27(6):531-43. PubMed PMID: 25115055.
27. Ebbens MM, Gombert-Handoko KB, Al-Dulaimy M, van den Bemt PMLA, Wesselink EJ. Risk factors for medication errors at admission in preoperatively screened patients. Pharmacoepidemiol Drug Saf. 2018 Mar;27(3):272-278. doi: 10.1002/pds.4380. Epub 2018 Jan 10. PubMed PMID: 29318695.
28. Fitzgerald RJ. Medication errors: the importance of an accurate drug history. Br J Clin Pharmacol. 2009 Jun;67(6):671-5. doi: 10.1111/j.1365-2125.2009.03424.x. PubMed PMID: 19594536; PubMed Central PMCID: PMC2723207.
29. Frisse ME, Tang L, Belsito A, Overhage JM. Development and use of a medication history service associated with a health information exchange: architecture and preliminary findings. AMIA Annu Symp Proc. 2010 Nov 13;2010:242-5. PubMed PMID: 21346977; PubMed Central PMCID: PMC3041403.
30. Gardiner P, Sadikova E, Filippelli AC, White LF, Jack BW. Medical reconciliation of dietary supplements: don't ask, don't tell. Patient Educ Couns. 2015 Apr;98(4):512-7. doi: 10.1016/j.pec.2014.12.010. Epub 2015 Jan 14. PubMed PMID: 25636694; PubMed Central PMCID: PMC4404157.
31. Graabæk T, Terkildsen BG, Lauritsen KE, Almarsdóttir AB. Frequency of undocumented medication discrepancies in discharge letters after hospitalization of older patients: a clinical record review study. Ther Adv Drug Saf. 2019 Jun 16;10:2042098619858049. doi: 10.1177/2042098619858049. eCollection 2019. PubMed PMID: 31244989; PubMed Central PMCID: PMC6580721.
32. Hartel MJ, Staub LP, Röder C, Eggli S. High incidence of medication documentation errors in a Swiss university hospital due to the handwritten prescription process. BMC Health Serv Res. 2011 Aug 18;11:199. doi: 10.1186/1472-6963-11-199. PubMed PMID: 21851620; PubMed Central PMCID: PMC3180357.
33. Harig A, Rybarczyk A, Benedetti A, Zimmerman J. Clarification of Drug Allergy Information Using a Standardized Drug Allergy Questionnaire and Interview. P T. 2018 Aug;43(8):480-504. PubMed PMID: 30100688; PubMed Central PMCID: PMC6065492.
34. Hughes A. Obtaining a Best Possible Medication History in Hospitals. Pharmacy Times® July 10, 2016.
35. Informed Health Online [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Drug allergies: Overview. 2017 Jul 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK447110/
36. Jonikas MA, Mandl KD. Surveillance of medication use: early identification of poor adherence. J Am Med Inform Assoc. 2012 Jul-Aug;19(4):649-54. doi: 10.1136/amiajnl-2011-000416. Epub 2011 Nov 19. PubMed PMID: 22101969; PubMed Central PMCID: PMC3384104.
37. Johnson PJ, Kozhimannil KB, Jou J, Ghildayal N, Rockwood TH. Complementary and Alternative Medicine Use among Women of Reproductive Age in the United States. Womens Health Issues. 2016 Jan-Feb;26(1):40-7. doi: 10.1016/j.whi.2015.08.009. Epub 2015 Oct 24. PubMed PMID: 26508093; PubMed Central PMCID: PMC4690756.
38. Jäger C, Steinhaeuser J, Freund T, Szecsenyi J, Goetz K. Medication Lists and Brown Bag Reviews: Potential Positive and Negative Impacts on Patients Beliefs about Their Medicine. Biomed Res Int. 2015;2015:874067. doi: 10.1155/2015/874067. Epub 2015 Oct 11. PubMed PMID: 26539533; PubMed Central PMCID: PMC4619852.
39. Johnston R, Saulnier L, Gould O. Best possible medication history in the emergency department: comparing pharmacy technicians and pharmacists. Can J Hosp Pharm. 2010 Sep;63(5):359-65. PubMed PMID: 22479003; PubMed Central PMCID: PMC2999367.
40. Kim HJ, Yang YM, Choi EJ. Use patterns of over-the-counter (OTC) medications and perspectives on OTC medications among Korean adult patients with chronic diseases: gender and age differences. Patient Prefer Adherence. 2018 Aug 28;12:1597-1606. doi: 10.2147/PPA.S173873. eCollection 2018. PubMed PMID: 30214162; PubMed Central PMCID: PMC6118289.
41. Kadam RA. Informed consent process: A step further towards making it meaningful! Perspect Clin Res. 2017 Jul-Sep;8(3):107-112. doi: 10.4103/picr.PICR_147_16. Review. PubMed PMID: 28828304; PubMed Central PMCID: PMC5543760.
42. Kram BL, Trammel MA, Kram SJ, Wheeley SE, Mancheril BG, Burgess LD, Schultheis JM. Medication Histories in Critically Ill Patients Completed by Pharmacy Personnel. Ann Pharmacother. 2019 Jun;53(6):596-602. doi: 10.1177/1060028018825483. Epub 2019 Jan 17. PubMed PMID: 30654616.
43. Lam WY, Fresco P. Medication Adherence Measures: An Overview. Biomed Res Int. 2015;2015:217047. doi: 10.1155/2015/217047. Epub 2015 Oct 11. Review. PubMed PMID: 26539470; PubMed Central PMCID: PMC4619779.
44. Lau HS, Florax C, Porsius AJ, De Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000 Jun;49(6):597-603. PubMed PMID: 10848724; PubMed Central PMCID: PMC2015045.
45. Lown B. The lost art of healing: practicing compassion in medicine. New York: Ballantine Books; 1999.
46. Lussier MT, Richard C. Communication tips. Medication list: enhancing patients' knowledge and adherence. Can Fam Physician. 2007 Feb;53(2):233-6. PubMed PMID: 17872639; PubMed Central PMCID: PMC1949120.
47. Mack H. Report: Pharma loses $637B annually due to medication nonadherence. MobiHealthNews,
48. McTier L, Botti M, Duke M. Patient participation in medication safety during an acute care admission. Health Expect. 2015 Oct;18(5):1744-56. doi: 10.1111/hex.12167. Epub 2013 Dec 17. PubMed PMID: 24341439; PubMed Central PMCID: PMC5060834.
49. Macchia D, Melioli G, Pravettoni V, Nucera E, Piantanida M, Caminati M, Campochiaro C, Yacoub MR, Schiavino D, Paganelli R, Di Gioacchino M; Food Allergy Study Group (ATI) of the Italian Society of Allergy, Asthma and Clinical Immunology (SIAAIC). Guidelines for the use and interpretation of diagnostic methods in adult food allergy. Clin Mol Allergy. 2015 Oct 5;13:27. doi: 10.1186/s12948-015-0033-9. eCollection 2015. Review. Erratum in: Clin Mol Allergy. 2015;13:31. PubMed PMID: 26441488; PubMed Central PMCID: PMC4593201.
50. Macchia A, Romero M, Comignani PD, Mariani J, D'Ettorre A, Prini N, Santopinto M, Tognoni G. Previous prescription of β-blockers is associated with reduced mortality among patients hospitalized in intensive care units for sepsis. Crit Care Med. 2012 Oct;40(10):2768-72. PubMed PMID: 22824934.
51. Mathioudakis A, Rousalova I, Gagnat AA, Saad N, Hardavella G. How to keep good clinical records. Breathe (Sheff). 2016 Dec;12(4):369-373. doi: 10.1183/20734735.018016. PubMed PMID: 28210323; PubMed Central PMCID: PMC5297955.
52. McShane M, Stark R. Medication Reconciliation in the Hospital: An Interactive Case-Based Session for Internal Medicine Residents. MedEdPORTAL. 2018 Nov 9;14:10770. doi: 10.15766/mep_2374-8265.10770. PubMed PMID: 30800970; PubMed Central PMCID: PMC6342339.
53. Mohiuddin AK. Community and Clinical Pharmacists in Transition Care. Glob J Pharmaceu Sci. 2019; 7(2): 555706. DOI: 10.19080/GJPPS.2019.06.555706.
54. Mazhar F, Haider N, Ahmed Al-Osaimi Y, Ahmed R, Akram S, Carnovale C. Prevention of medication errors at hospital admission: a single-centre experience in elderly admitted to internal medicine. Int J Clin Pharm. 2018 Dec;40(6):1601-1613. doi: 10.1007/s11096-018-0737-2. Epub 2018 Oct 26. PubMed PMID: 30367379.
55. Maideen NMP. Tobacco smoking and its drug interactions with comedications involving CYP and UGT enzymes and nicotine. World J Pharmacol 2019; 8(2): 14-25
56. Maas ET, Juch JN, Ostelo RW, Groeneweg JG, Kallewaard JW, Koes BW, Verhagen AP, Huygen FJ, van Tulder MW. Systematic review of patient history and physical examination to diagnose chronic low back pain originating from the facet joints. Eur J Pain. 2017 Mar;21(3):403-414. doi: 10.1002/ejp.963. Epub 2016 Oct 10. Review. PubMed PMID: 27723170.
57. Nester TM, Hale LS. Effectiveness of a Pharmacist-Acquired Medication History in Promoting Patient Safety. Am J Health Syst Pharm. 2002;59(22)
58. Nichol JR, Nelson G. Medical History. [Updated 2019 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534249/
59. Nickless G, Davies R. How to take an accurate and detailed medication history. The Pharmaceutical Journal 16 February, 2016.
60. Naicker P, Schellack N, Godman B, Bronkhorst E. Creating and evaluating an opportunity for medication reconciliation in the adult population of South Africa to improve patient care. Hosp Pract (1995). 2018 Aug;46(3):110-120. doi: 10.1080/21548331.2018.1461528. Epub 2018 Apr 16. PubMed PMID: 29619837.
61. Oyedokun A, Adeloye D, Balogun O. Clinical history-taking and physical examination in medical practice in Africa: still relevant? Croat Med J. 2016 Dec 31;57(6):605-607. PubMed PMID: 28051286; PubMed Central PMCID: PMC5209934.
62. Ohm F, Vogel D, Sehner S, Wijnen-Meijer M, Harendza S. Details acquired from medical history and patients' experience of empathy--two sides of the same coin. BMC Med Educ. 2013 May 9;13:67. doi: 10.1186/1472-6920-13-67. PubMed PMID: 23659369; PubMed Central PMCID: PMC3661386.
63. Parker L. 10 Steps to Take an Accurate Inpatient Medication History. Pharmacy Times® July 14, 2016.
64. Patel MJ, Khan MS, Ali F, Kazmi Z, Riaz T, Awan S, Sorathia AL. Patients' insight of interpreting prescriptions and drug labels--a cross sectional study. PLoS One. 2013 Jun 3;8(6):e65019. doi: 10.1371/journal.pone.0065019. Print 2014. PubMed PMID: 23755168; PubMed Central PMCID: PMC3670850.
65. Pandit MS, Pandit S. Medical negligence: Coverage of the profession, duties, ethics, case law, and enlightened defense - A legal perspective. Indian J Urol. 2009 Jul;25(3):372-8. doi: 10.4103/0970-1591.56206. PubMed PMID: 19881134; PubMed Central PMCID: PMC2779963.
66. Pourrat X, Roux C, Bouzige B, Garnier V, Develay A, Allenet B, Fraysse M, Halimi JM, Grassin J, Giraudeau B. Impact of drug reconciliation at discharge and communication between hospital and community pharmacists on drug-related problems: study protocol for a randomized controlled trial. Trials. 2014 Jun 30;15:260. doi: 10.1186/1745-6215-15-260. PubMed PMID: 24981605; PubMed Central PMCID: PMC4226949.
67. Posadzki P, Watson LK, Alotaibi A et al. Prevalence of herbal medicine use by UK patients / consumers: a systematic review of surveys. Focus on Alternative and Complementary Therapies 2013;18(1):19–26. doi: 10.1111/fct.12006
68. Porter SC, Kohane IS, Goldmann DA. Parents as partners in obtaining the medication history. J Am Med Inform Assoc. 2005 May-Jun;12(3):299-305. Epub 2005 Jan 31. PubMed PMID: 15684127; PubMed Central PMCID: PMC1090461.
69. Parvez MK, Rishi V. Herb-Drug Interactions and Hepatotoxicity. Curr Drug Metab. 2019;20(4):275-282. doi: 10.2174/1389200220666190325141422. PubMed PMID: 30914020.
70. Peterson MC, Holbrook JH, Von Hales D, Smith NL, Staker LV. Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med. 1992 Feb;156(2):163-5. PubMed PMID: 1536065; PubMed Central PMCID: PMC1003190.
71. Petrov K, Varadarajan R, Healy M, Darvish E, Cowden C. Improving Medication History at Admission Utilizing Pharmacy Students and Technicians: A Pharmacy-Driven Improvement Initiative. P T. 2018 Nov;43(11):676-684. PubMed PMID: 30410283; PubMed Central PMCID: PMC6205119.
72. Penm J, Vaillancourt R, Pouliot A. Defining and identifying concepts of medication reconciliation: An international pharmacy perspective. Res Social Adm Pharm. 2019 Jun;15(6):632-640. doi: 10.1016/j.sapharm.2018.07.020. Epub 2018 Aug 1. PubMed PMID: 30100200.
73. Ronis MJJ, Pedersen KB, Watt J. Adverse Effects of Nutraceuticals and Dietary Supplements. Annu Rev Pharmacol Toxicol. 2018 Jan 6;58:583-601. doi: 10.1146/annurev-pharmtox-010617-052844. Epub 2017 Oct 6. Review. PubMed PMID: 28992429; PubMed Central PMCID: PMC6380172.
74. Regitz-Zagrosek V. Sex and gender differences in health. Science & Society Series on Sex and Science. EMBO Rep. 2012 Jun 29;13(7):596-603. doi: 10.1038/embor.2012.87. PubMed PMID: 22699937; PubMed Central PMCID: PMC3388783.
75. Roshan M, Rao AP. A study on relative contributions of the history, physical examination and investigations in making medical diagnosis. J Assoc Physicians India. 2000 Aug;48(8):771-5. PubMed PMID: 11273467.
76. Rappaport R, Arinzon Z, Feldman J, Lotan S, Heffez-Aizenfeld R, Berner Y. The Need for Medication Reconciliation Increases with Age. Isr Med Assoc J. 2017 Oct;19(10):625-630. PubMed PMID: 29103240.
77. Royal Pharmaceutical Society (RPS) of Great Britain (2011). Medication History: A quick reference guide. Available from: https://www.nicpld.org/courses/fp/assets/MM/RPSMedicationHistoryQuickRefGuide.pdf
78. Shetty V, Chowta MN, Chowta K N, Shenoy A, Kamath A, Kamath P. Evaluation of Potential Drug-Drug Interactions with Medications Prescribed to Geriatric Patients in a Tertiary Care Hospital. J Aging Res. 2018 Oct 9;2018:5728957. doi: 10.1155/2018/5728957. eCollection 2018. PubMed PMID: 30402286; PubMed Central PMCID: PMC6198551.
79. Samaranayake NR, Bandara WG, Manchanayake CM. A narrative review on do's and don'ts in prescription label writing - lessons for pharmacists. Integr Pharm Res Pract. 2018 Jun 13;7:53-66. doi: 10.2147/IPRP.S163968. eCollection 2018. Review. PubMed PMID: 29942789; PubMed Central PMCID: PMC6005331.
80. Schepel L, Lehtonen L, Airaksinen M, Ojala R, Ahonen J, Lapatto-Reiniluoto O. Medication reconciliation and review for older emergency patients requires improvement in Finland. Int J Risk Saf Med. 2019;30(1):19-31. doi: 10.3233/JRS-180030. PubMed PMID: 30103352; PubMed Central PMCID: PMC6294607.
81. Simpson RF, Hermon C, Liu B, Green J, Reeves GK, Beral V, Floud S; Million Women Study Collaborators. Alcohol drinking patterns and liver cirrhosis risk: analysis of the prospective UK Million Women Study. Lancet Public Health. 2019 Jan;4(1):e41-e48. doi: 10.1016/S2468-2667(18)30230-5. Epub 2018 Nov 22. PubMed PMID: 30472032; PubMed Central PMCID: PMC6323353.
82. Stockton KR, Wickham ME, Lai S, Badke K, Dahri K, Villanyi D, Ho V, Hohl CM. Incidence of clinically relevant medication errors in the era of electronically prepopulated medication reconciliation forms: a retrospective chart review. CMAJ Open. 2017 May 5;5(2):E345-E353. doi: 10.9778/cmajo.20170023. PubMed PMID: 28476877; PubMed Central PMCID: PMC5498425.
83. Séroussi B, Bouaud J. Adoption of a Nationwide Shared Medical Record in France: Lessons Learnt after 5 Years of Deployment. AMIA Annu Symp Proc. 2017 Feb 10;2016:1100-1109. eCollection 2016. PubMed PMID: 28269907; PubMed Central PMCID: PMC5333332.
84. Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014 Jul 22;36:e2014009. doi: 10.4178/epih/e2014009. eCollection 2014. Review. PubMed PMID: 25078382; PubMed Central PMCID: PMC4154347.
85. Summers A, Ruderman C, Leung FH, Slater M. Examining patterns in medication documentation of trade and generic names in an academic family practice training centre. BMC Med Educ. 2017 Sep 22;17(1):175. doi: 10.1186/s12909-017-1015-z. PubMed PMID: 28938883; PubMed Central PMCID: PMC5610475.
86. Shenfield GM, Robb T, Duguid M. Recording previous adverse drug reactions--a gap in the system. Br J Clin Pharmacol. 2001 Jun;51(6):623-6. PubMed PMID: 11422023; PubMed Central PMCID: PMC2014491.
87. Toich L. The Cost of Medication Adherence to Pharma. Specialty Pharmacy Times, December 30, 2016.
88. Tesfamariam S, Anand IS, Kaleab G, Berhane S, Woldai B, Habte E, Russom M. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health. 2019 Feb 6;19(1):159. doi: 10.1186/s12889-019-6470-5. PubMed PMID: 30727984; PubMed Central PMCID: PMC6364400.
89. Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol. 2010 Feb 9;55(6):515-25. doi: 10.1016/j.jacc.2009.07.074. Review. PubMed PMID: 20152556; PubMed Central PMCID: PMC2831618.
90. Taib IA, McIntosh AS. On the integration and standardization of medication error data: taxonomies, terminologies, causes and contributing factors. Ther Adv Drug Saf. 2010 Dec;1(2):53-63. doi: 10.1177/2042098610389850. PubMed PMID: 25083195; PubMed Central PMCID: PMC4110805.
91. Toney-Butler TJ, Unison-Pace WJ. Nursing Admission Assessment and Examination. [Updated 2019 Jun 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493211/
92. Thomas J. Medical records and issues in negligence. Indian J Urol. 2009 Jul;25(3):384-8. doi: 10.4103/0970-1591.56208. PubMed PMID: 19881136; PubMed Central PMCID: PMC2779965.
93. Vicente Oliveros N, Gramage Caro T, Pérez Menendez-Conde C, Álvarez-Díaz AM, Martín-Aragón Álvarez S, Bermejo Vicedo T, Delgado Silveira E. Effect of an electronic medication administration record application on patient safety. J Eval Clin Pract. 2017 Aug;23(4):888-894. doi: 10.1111/jep.12753. Epub 2017 Apr 18. PubMed PMID: 28418101.
94. Vassilev I, Rogers A, Kennedy A, Koetsenruijter J. The influence of social networks on self-management support: a metasynthesis. BMC Public Health. 2014 Jul 15;14:719. doi: 10.1186/1471-2458-14-719. Review. PubMed PMID: 25023948; PubMed Central PMCID: PMC4223639.
95. WHO (2006). Medical Records Manual: A Guide for Developing Countries. Available From: http://www.herai.in/admin/upload/resouce/7751185308Medical%20Records%20Manual.pdf
96. Wang T, Biederman S. Enhance the accuracy of medication histories for the elderly by using an electronic medication checklist. Perspect Health Inf Manag. 2012;9:1-15. Epub 2012 Oct 1. PubMed PMID: 23209450; PubMed Central PMCID: PMC3510644.
97. Wang J, Wongvibulsin S, Henry K, Fujita S. Quantifying and Visualizing Medication Adherence in Patients Following Acute Myocardial Infarction. AMIA Annu Symp Proc. 2018 Apr 16;2017:2299-2303. eCollection 2017. PubMed PMID: 29854272; PubMed Central PMCID: PMC5977657.
98. Worm M, Reese I, Ballmer-Weber B, Beyer K, Bischoff SC, Classen M, Fischer PJ, Fuchs T, Huttegger I, Jappe U, Klimek L, Koletzko B, Lange L, Lepp U, Mahler V, Niggemann B, Rabe U, Raithel M, Saloga J, Schäfer C, Schnadt S, Schreiber J, Szépfalusi Z, Treudler R, Wagenmann M, Watzl B, Werfel T, Zuberbier T, Kleine-Tebbe J. Guidelines on the management of IgE-mediated food allergies: S2k-Guidelines of the German Society for Allergology and Clinical Immunology (DGAKI) in collaboration with the German Medical Association of Allergologists (AeDA), the German Professional Association of Pediatricians (BVKJ), the German Allergy and Asthma Association (DAAB), German Dermatological Society (DDG), the German Society for Nutrition (DGE), the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS), the German Society for Oto-Rhino-Laryngology, Head and Neck Surgery, the German Society for Pediatric and Adolescent Medicine (DGKJ), the German Society for Pediatric Allergology and Environmental Medicine (GPA), the German Society for Pneumology (DGP), the German Society for Pediatric Gastroenterology and Nutrition (GPGE), German Contact Allergy Group (DKG), the Austrian Society for Allergology and Immunology (Æ-GAI), German Professional Association of Nutritional Sciences (VDOE) and the Association of the Scientific Medical Societies Germany (AWMF). Allergo J Int. 2015;24:256-293. Epub 2015 Nov 7. PubMed PMID: 27069841; PubMed Central PMCID: PMC4792347.
99. Willeboordse F, Hugtenburg JG, Schellevis FG, Elders PJ. Patient participation in medication reviews is desirable but not evidence-based: a systematic literature review. Br J Clin Pharmacol. 2014 Dec;78(6):1201-16. doi: 10.1111/bcp.12398. Review. PubMed PMID: 24698145; PubMed Central PMCID: PMC4256610.
100. Yusuff KB, Tayo F, Aina BA. Pharmacists' participation in the documentation of medication history in a developing setting: An exploratory assessment with new criteria. Pharm Pract (Granada). 2010 Apr;8(2):139-45. Epub 2010 Mar 15. PubMed PMID: 25132882; PubMed Central PMCID: PMC4133068.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









