About Authors:
Varsha Tanaji Jadhav1*, 2Joyeeta Sanyal
Cilicant Chem.Pvt.Ltd., Microbiologist, Pune
Rasayani Biologic.Ltd., Microbiologist
*varsha.jadhav6@gmail.com
Abstract:-
Nephrotoxcity is the injury or damage to the one or both of the kidneys due to a toxic material. Usually toxic material taken orally results in nephrotoxicity. The kidneys are the most essential organs of the urinary system. They are responsible for the quality, quantity and filtration of the fluids in the body. Every day, the kidneys filter about 180 litres of blood, and about four times as much as the amount that passes through any other organ. Hence the kidneys are more often exposed to toxic substances in the blood and are very vulnerable to damage from those materials. They also help to control blood pressure and other direct cell activities and homeostasis as they produce vitamins and hormones for example hormones erythropoietin, rennin. Other important functions performed by them are regulation of calcium, chloride, sodium ions, and pH control (Taferner B, et al., 2009). The kidneys functional units are the nephrons. Diseases of the kidney are diverse, but they commonly display some characteristic clinical features. These include chronic diseases, acute injuries, urinary tract obstruction and infection, renal damage or failure. Epidemiological results suggest that environmental toxins like heavy metals plays significant role in the development of these diseases. Particularly large amounts of these are disposed of as industrial by-products which are not biodegradable. The incidences of chronic and acute renal failures have risen in past few years. In the America only, kidney diseases are the ninth leading cause of death (Ernesto Sabath et al., 2012). Hence identifying the risk factors associate with these diseases is important to prevent it.This report aims to discuss the physiopathological mechanisms and the consequences of kidney injury due to arsenic and Non Steroidal Anti Inflammatory Drugs (NSAID).
REFERENCE ID: PHARMATUTOR-ART-1838
Introduction:-
Arsenic Nephrotoxicity:-
Arsenic is one of the most widely spread environmental pollutant, and millions of people mainly in Asia and Latin America suffer from its exposure. It is the commonly spread in drinking water via industrial wastes. Approximately average daily human exposure of arsenic is 20µg via food and water (WHO, 2001).Other forms of the exposure are the medicines used in treatment of cancer, sleeping sickness, and compounds used in Silicon-based computer chips, manufacturing of glass, feed additive (poultry and swine), and wood preservative(Jarup, 2003).
Clinical manifestations:-
Since ancient times in organic arsenic has been recognized as human poison. Periodically arsenic related consequences have been reviewed. The arsenic toxicity is systematic and involves number of organ system. These effects can be acute, sub-acute and chronic as well (Chen et al., 1997). The acute and sub acute effects of the arsenic toxicity are shown in the table 1
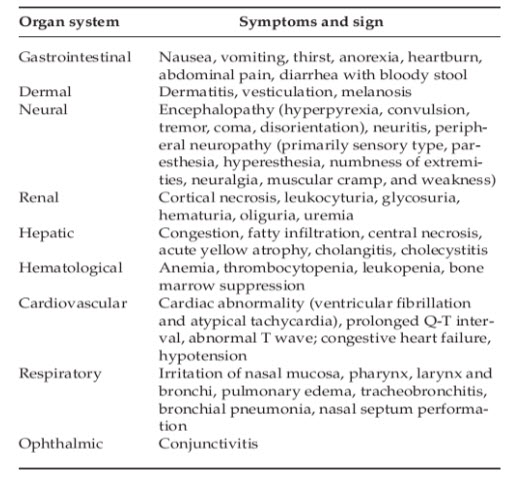
Table 1 Acute and Sub acute Toxicity of Arsenic
(Source: -WHO, 1981, 2001; ATSDR, 2005, Chen et al. 1997)
Most studies on arsenic do not have exact details of dose response relationship details. Inorganic arsenic is easily absorbed from intestine compared to the organic one. Earliest symptoms of acute toxicity are dry mouth and burning lips. The sites of kidney damage are glomeruli, capillary and tubules (Chen et al., 1997). As the kidneys are affected, it shut downs there is no hemodynamic balance. It results innecrosis and rapid cell death. Hyperkeratosis or Blackfoot disease is characteristic vascular disease due to arteriosclerosis, is observed in long term exposure to arsenic (Figure1). It binds to red blood cells andsulfhydryl-containing proteins. The literature does not offer much information on manifestations of arsenic toxicity in the kidneys. But on the basis of available data it concludes that it results in damage to tubules, low molecular weight proteinuria, glycosuria, aminoaciduria and deterioration of renal function (Huang M et al., 2009). It affects the filtration process, salt and water balance in the body due to injury to the kidneys.Hence long term effects are mostly seen on the cardiovascular system. Table 2 shows the chronic long term effects of the arsenic via ingestion and inhalation.
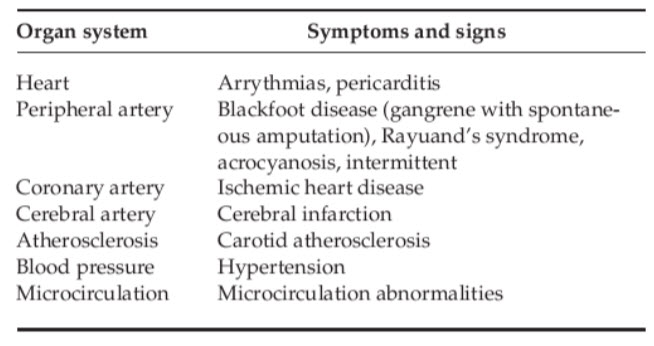
Table 2 Chronic Cardiovascular toxicity of arsenic
(Chen et al., 1997 Chen et al., 2005, ATSDR, 2005)
It has been classified as the group 1 carcinogen based on the literature studies. It shows the significant amount of dose- response relationship in long term exposure between the arsenic in the drinking water and increased risk of cancers lesions in the liver, kidney, skin, urinary bladder, lungs and nasal cavities (IARC, 2004, 2006).
Mechanism of Arsenic Nephrotoxicity:-
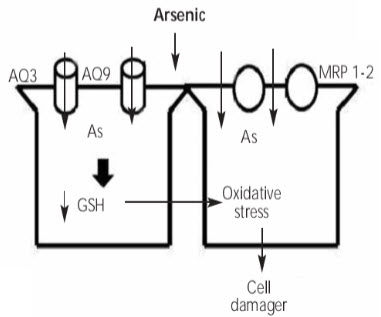
Figure 2 Mechanism of arsenic induced kidney injury
(Ernesto Sabath et al., 2012)
As arsenic is absorbed in the intestine, lungs (inhalation) and in some amount in skin it is transformed from the less toxic pentavalent form to more toxic trivalent form in liver and renal tubules in kidneys (Ellenhorn MJ et al., 1988). Arsenic is methylated in the liver via glutathione (GSH) process which leads to its excretion via biliary excretion (Fig2). In the intracellular medium these are transported in via aquaglyceroporins AQ3 and AQ9. This process causes results in the accumulation of arsenic ions and ultimately results in there excretion. But if there is glutathione stores (GSH) depletion in the body, it results in increase in the oxidative activity reactive free radicals (Carbrey et al., 2009). Another group proteins which are also involved in this process are multi drug resistance proteins (MRP 1-2).These are involved in the transport of arsenic from glutathione (GSH) to the bile for excretion. Binding to the thiol groups causes activation of signal cascade, impairment of antioxidant defence mechanism and triggers apoptosis (Flora et al., 2008).
There have been many cases of toxicity associated with heavy metals. As these are commonly found in our living environment and there are only few treatment options on them, so public awareness should be made to reduce the usage and to limit their exposure. Every precautionary step and safety recommendations while handling heavy metals should be followed.
Nonsteroidal anti-inflammatory drugs (NSAIDs) induced Nephrotoxicity
Introduction :-
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the class of drugs which provide anti-pyretic, analgesic and anti-inflammatory effects. The term non steroidal separates it from other steroids which have range of other similar effects. Aspirin, naproxen and ibuprofen are the most common and prominent members of this group. These are all available over the counters in most countries (Stuart, 2010). The widespread and in certain population daily use of these drugs have become increasingly prevalent. Commonly two main adverse drug reactions associated with Nonsteroidal anti-inflammatory drugs (NSAIDs) are the effects on renal tubules and gastrointestinal (GI) tract. In the 1980s clinical consequences of Nonsteroidal anti-inflammatory drugs (NSAIDs) were well documented (Dunn et al., 1980, 1984). In America only approximately 43% deaths, emergency hospitalization and adverse drug reaction cases every year are due to the Nonsteroidal anti-inflammatory drugs (NSAIDs) (Green, 2001). The controversies regarding their usage led to the discovery of selective cyclo-oxygenase 2 (COX-2) inhibitors.
Clinical Manifestations in Human due to Nonsteroidal anti-inflammatory drugs (NSAIDs):-
Nonsteroidal anti-inflammatory drugs (NSAIDs) are associated with the renal adverse reactions. Common renal adverse drug reactions include:-
Hypertension:
Hypertension or high blood pressure is the chronic medical condition in which the pressure of the blood in the arteries is elevated. It causes heart to work harder than normal to circulate blood through the body. This condition may arise due to adverse drug reactions involving anti-inflammatory drugs like ibuprofen and including cyclo-oxygenase 2 (COX-2) inhibitors as well (Black HR et al., 2003). It can result in myocardial infarction and stroke.
Chronic analgesic nephritis: -
Analgesic nephropathy is a term used to describe the injury to the kidney caused by the use of combinations of analgesic medications like paracetamol, aspirin, and phenacetin. It may arise due to the chronic use of single medication as well. Analgesic drugs affect the blood flow to the kidney and causes oxidative damage to the kidney (McLaughlin et al., 1998).
Obstructive nephropathy:-
This type of adverse drug reaction is mainly associated with the administration of sulphonamides. Sulphonamides the antibacterial drugs are more likely to precipitate in urine, particularly when urine is more acidic. The acetylated forms of drug like sulfadiazine are the least soluble. Crystals of sulphonamide are formed in the renal tubules causing crystalluria (Daudon et al., July 2003).
Allergic Nephropathy:-
Nonsteroidal anti-inflammatory drugs (NSAIDs) like cephalosporins, penicillin’s can cause renal injury by an allergic reaction. It is delayed type of response when reaction occurs after few days of initial drug therapy.
Glomerular nephritis:-
It is a renal disease in which glomeruli or small blood vessels in the kidney (usually both) are damaged in response to inflammation (Couser et al., 1999).
Mechanism of NSAIDs Nephrotoxicity:-
Kidney have high metabolic requirement than any other organ in the body as it receives 20% of cardiac output. Kidney is an active site for prostaglandin production. Prostaglandin, Thromboxanes and Leucotreine are the various inflammatory mediators derived and regulated by the phospholipids in the plasma membrane via lipo-oxygenase and cyclo-oxygenase pathways (Figure 3).
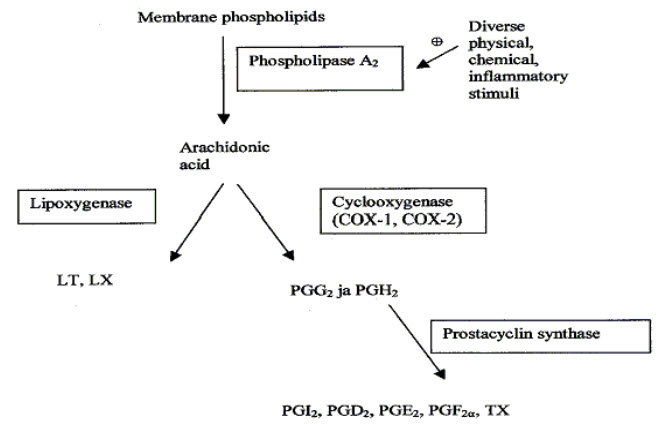
Figure 3 Prostaglandin production (Source: - Maroon et al., 2010)
Kidneys are also major route of excretion to many drug metabolites. Hence kidney tubules are exposed to high concentrations of the drug and drug metabolites. When there is renal compromise for example during dehydration, renal dysfunction, electrolyte depletion. Kidney is dependent on cyclo-oxygenase 1 and 2 (COX 1, COX2) for prostaglandin synthesis to auto regulate water balance, renal blood flow and tubular functions. NSAIDs (for example flunixin, ibuprofen) associated renal toxicity is characterized by sodium and fluid retention, decreased renal function and perfusion. These NSAIDs inhibit the renal prostaglandin synthesis ability by interrupting in between cyclo-oxygenase pathway. Other than Inflammatory mediator’s, the prostaglandins are involved in the regulation and modulation of haemodynamics, gastric mucosal enzymes integrity, tubular salt and water reabsorption, rennin release. Hence when those administered nephrotoxicity is rather inevitable. It can result in renal ischemia. The combination of other drug and NSAIDS can also increase the risk of renal injury. For example combination of anaesthesia and NSAIDs increases risk to renal injury (Gambaro & Perazella, 2003).Persons having any other chronic renal disease or dehydration are at great risk of acute renal failure while taking NSAIDs. According to National Kidney Foundation report nearly 10 % cases are directly correlated to the over use of NSAIDs. The cyclo-oxygenase 2(COX-2) inhibitors like Vioxx have been reported for major gastrointestinal (GI) tract side effects in past few years. Particularly older populations group are at higher risk of gastrointestinal (GI) tract complications. Aspirin is now believed to be responsible for inhibition of both cyclo-oxygenase and NF-kB pathway. NF-kB is transcriptional factor, which controls Deoxy ribose nucleic acid (DNA) transcription during inflammatory immune response. It has ability to detect damaging stimuli for example infectious agents, free radicals and cell injuries. After detection it directs the Deoxy ribose nucleic acid (DNA) to produce inflammatory cytokines and chemokines (Wang et al., 2004).
Conclusion:-
The risk of nephrotoxic injury can be reduced by taking proper precautions and by reducing the dosage of antibiotics. Populations which are at high risk for example elderly persons and infants should be closely monitored to prevent overdose.
References
- ATSDR. (2005). Toxicological Profile for Arsenic. Draft for public comment. Agency for Toxic Substances and Disease Registry, Atlanta, GA. 29–182.
- Carbrey JM, Song L, Zhou Y, Yoshinaga M, Rojek A. Reduced arsenic clearance and increased toxicity in aquaglyceroporin-9-null mice. Proc Natl Acad Sci U S A 2009;106:15956-60.
- Chen, C. J., Hsueh, Y. M., Chiou, H. Y., et al. (1997b). In“Arsenic: Exposure and Health Effects.” (C. O. Abernathy, R. L. Cal-deron, and W. R. Chappell, Eds.), pp. 232–242. Chapman & Hall, London.
- Chobanian AV, Bakris GL, Black HR et al. (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension 42 (6): 1206–52.
- Couser WG (May 1999). "Glomerulonephritis". Lancet 353 (9163): 1509–15. doi:10.1016/S0140-6736(98)06195-9. PMID 10232333.
- Daudon M, Cohen-Solal F, Barbey F, Gagnadoux MF, Knebelmann B, Jungers P (July 2003). "Cystine crystal volume determination: a useful tool in the management of cystinuric patients". Urol. Res. 31 (3): 207–11. doi:10.1007/s00240-003-0319-0. PMID 12748836.
- Dunn MJ, Zambraski EJ: Renal effects of drugs that inhibit prostaglandin synthesis. Kidney Int 18:609-622, 1980.
- Dunn MJ: Nonsteroidal anti-inflammatroy drugs and renal function. Annu Rev Med 35:411-428, 1984.
- Sabath Ernesto, 2012. Renal health and the environment: heavy metal nephrotoxicity. Spanish Nephrology Society. 32, 279-86 [Online] Available at: revistanefrologia.com [Accessed 02 December 2012].
- Ellenhorn MJ, Barceloux DG. Arsenic in medical toxicology: diagnosis and treatment of human poisoning. New York: Elsevier. 1988: 1012-6.
- Gambaro G, Perazella MA: Adverse renal effects of anti-inflammatory agents: Evaluation of selective and nonselec-tive cyclooxygenase inhibitors. J Intern Med 253: 643–652, 2003.
- Glodny B, Unterholzner V, Taferner B, et al. (2009). "Normal kidney size and its influencing factors - a 64-slice MDCT study of 1.040 asymptomatic patients". BMC Urology 9: 19. doi:10.1186/1471-2490-9-19. PMC 2813848. PMID 20030823.
- Green, Ga (2001). "Understanding NSAIDs: from aspirin to COX-2". Clinical cornerstone 3 (5): 50–60. doi:10.1016/S1098-3597(01)90069-9. ISSN 1098-3597. PMID 11464731.
- Huang M, Choiu SJ, Kim DW, Kim NY, Park CH, Yu SD et al. Risk assessment of low-level cadmium and arsenic on the kidney. J Toxicol Environ Health A 2009; 72:149.
- IARC Monographs. (2004). “Evaluation of Carcinogenic Risks to Humans: Some Drinking-water Disinfectants and Contaminants, including Arsenic.” Vol. 84. 512 pp. International Agency for Re-search on Cancer, Lyon.
- IARC Monographs. (2006). “Evaluation of the Carinogenic Risks to Humans: Cobalt in Hard Metals and Cobalt Sulfate, Gallium Arsenide, Indium Phosphide and Vanadium Pentoxide.” Vol. 86. 330 pp. International Agency for Research on Cancer, Lyon.
- Jarup L. Hazards of heavy metal contamination. British Medical Bulletin. 2003. 68:167-182.
- Maroon J C, Bost JW, Maroon A, Natural anti-inflammatory agents for pain relief Surg Neurol Int 2010,I:80.
- McLaughlin JK, Lipworth L, Chow WH, Blot WJ (September 1998). "Analgesic use and chronic renal failure: a critical review of the epidemiologic literature". Kidney Int. 54 (3): 679–86. doi:10.1046/j.1523-1755.1998.00043.x. PMID 9734593
- Warden, Stuart J. (April 2010). "Prophylactic Use of NSAIDs by Athletes: A Risk/Benefit Assessment". The Physician and Sports Medicine 38 (1): 132138. doi:10.3810/psm.2010.04.1770. PMID 20424410.
- Wang C, Chung M, Lichtenstein A, Balk E, Kupelnick B, DeVine D, Lawrence A, Lau J. Effects of omega-3 fatty acids on cardiovascular disease. Evid Rep Technol Assess (Summ). 2004 Mar;(94):1-8. Review. PubMed PMID: 15133888.
- WHO. (1981). “Environmental Health Criteria, Arsenic.” pp. 1–174. World Health Organization, Geneva.
- WHO. (2001). “Environmental Health Criteria, 224, Arsenic and Arsenic Compounds.” 2nd ed. pp. 385–392. World Health Organi-zation, Geneva.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









