{ DOWNLOAD AS PDF }
ABOUT AUTHOR
AK MOHIUDDIN
Faculty of Pharmacy, World University of Bangladesh
Dhanmondi, Dhaka, Bangladesh
ABSTRACT
Medication errors are basic all in all training and in healing facilities. The two errors in the demonstration of writing (prescription/administering/administration errors) and endorsing deficiencies because of imperfect medicinal choices can result in mischief to patients. Any progression in the endorsing procedure can ignite errors. Slips, passes, or missteps are wellsprings of errors, as in unintended oversights in the account of medications. Blames in portion determination, discarded transcription, and poor handwriting are normal. Lacking mindfulness or ability and deficient data about clinical qualities and past treatment of individual patients can bring about endorsing issues, including the utilization of possibly mistaken medications. A perilous workplace, intricate or indistinct techniques, and deficient correspondence among human services staff, especially among specialists and medical attendants, have been distinguished as huge basic factors that add to prescription errors and endorsing issues. Dynamic intercessions went for diminishing prescription and endorsing issues are emphatically prescribed. This ought to be committed on the instruction and preparing of prescribers and the utilization of on-line helps. The unpredictability of the endorsing methodology ought to be decreased by presenting mechanized frameworks or uniform recommending diagrams, so as to abstain from account and exclusion errors. Input control frameworks and quick audit of prescriptions, which can be performed with the help of a healing center drug specialist, are additionally useful. Reviews ought to be performed occasionally.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-2644
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 7, Issue 02 Received On: 08/12/2018; Accepted On: 12/01/2019; Published On: 01/02/2019 How to cite this article: Mohiuddin, A.K. 2019. Framework for Patient Safety. PharmaTutor. 7, 2 (Feb. 2019), 21-34. DOI:https://doi.org/10.29161/PT.v7.i2.2019.21 |
Objective: Discussion and projection of medication safety and the strategies to improve its efficiency.
Methods: The research is conducted through secondary data search from several sources from books, technical newsletters, newspapers, journals, and many other sources. The present study was started from the start of 2018. PubMed, ALTAVISTA, EMBASE, Scopus, Web of Science, and the Cochrane Central Register of was thoroughly searched. The keywords were used to explore different publishers’ journals like Elsevier, Springer, Willey Online Library, Wolters Kluwer were extensively followed.
Findings: A medication intervention is a sophisticated technique of both arts and science. Improvement is valued when the total system co-ordination brings an overall improvement in every aspect of prescribing, dispensing, administration and monitoring. Error in any stage ruins the effort of the total system.
INTRODUCTION
Medicines are the commonest medicinal interruptions utilized in social insurance and safe use is important. Over the previous 20 years, various activities went for enhancing drug wellbeing have been brought into doctor's facilities. Clinicians, policymakers and patients presently need to realize whether advance has been made and where further upgrade might be required. Blunder offered a comparable end in respect to security: defects are unsuitable and normal. As indicated by a 2000 report referring to UK medicinal protection associations, 25% of all claim guarantees by and large restorative practice were because of prescription blunders and included recommending and apportioning mistakes (counting a wrong, contraindicated or unlicensed medication, a wrong measurement, or wrong organization); continue endorsing without legitimate checks; inability to screen advancement; and inability to caution about unfriendly impacts (which may, nonetheless, not be viewed as a drug mistake). The powerful cure isn't to frighten the medicinal services workforce by requesting that they invest more energy to give safe consideration, when truth be told, the valor, diligent work, and vow of social insurance specialists are the main genuine intends to stem the tide of blunders inactive in the human services framework. Development in information and innovations has never been so significant and productive. Nonetheless, look into on the nature of consideration discovers that the human services framework misses the mark in its capacity to make an interpretation of learning to rehearse and to apply new innovations securely and suitably. These standards medicinal services associations could take now or as quickly as time permits to considerably enhance tolerant security incorporate (1) offering authority; (2) concerning human points of confinement in process plan; (3) advancing powerful group working; (4) foreseeing the unforeseen; and (5) making a learning milieu.
Important Definitions
Active Error: Dynamic mistakes are those occurring between an individual and a part of a bigger framework at the purpose of contact. Dynamic blunders are made by individuals on the bleeding edge, for example, doctors and medical attendants. For instance, working on the wrong eye or removed the wrong leg are exemplary instances of a functioning mistake.
Adverse Event: Untoward occasions might be preventable when there is an inability to pursue acknowledged practice at a framework or individual dimension. An unfriendly occasion owing to a mistake for the most part is a preventable unfavorable occasion.
Latent Error: These are blunders in framework or process plan, flawed establishment or upkeep of gear, or incapable regulatory structure. These are available, yet may go unnoticed for quite a while with no evil impact.
Medical Error (ME): The failure to complete the intended plan of action or implementing the wrong plan to achieve an aim. An unintended act or one that fails to achieve the intended outcome. This definition is clearly oriented to the outcome of the error. However, it does not take into account catastrophes that can occur during the whole process of prescribing, independently of any potential or actual harm.
Prescription Error: Prescription Errors incorporate those identified with the demonstration of composing a remedy, though recommending shortcomings include nonsensical endorsing, improper endorsing, under-recommending, overprescribing, and inadequate endorsing, emerging from mistaken therapeutic judgment or choices concerning treatment or treatment checking. Proper endorsing results when blunders are limited and when the prescriber effectively tries to achieve better recommending: the two activities are required.
Negligent Adverse Events: A subcategory of preventable, unfriendly occasions that fulfill the lawful criteria utilized in characterizing carelessness. The damage caused by substandard medicinal administration.
Near Miss: Any occasion that could have had an unfavorable patient result however did not. Close botches give chances to creating preventive systems and activities and ought to get indistinguishable dimension of examination from unfriendly occasions.
Noxious Episode: Untoward occasions, inconveniences, and disasters that outcome from adequate symptomatic or remedial measures intentionally initiated. For instance, sending a hemodynamically unsteady injury tolerant for determined imaging examines rather than the working room. The outcome could be an awful capture and passing.
Patient Safety: The procedure of enhancement, shirking, and anticipation of antagonistic wounds or results that emerge because of the human services process (Rodziewicz et.al., 2018).
Scope of Safety Problems
The arrangement of high caliber, moderate, social insurance administrations is a continuously troublesome test. Because of the complexities of social insurance administrations and frameworks, researching and translating the utilization, costs, quality, openness, conveyance, association, financing, and results of medicinal services administrations is vital to educating government authorities, safety net providers, suppliers, supporters, and others settling on choices about wellbeing related issues. Suitable prescription use is a mind-boggling process including numerous associations and callings from different orders joined with a working learning of meds, access to precise and finish understanding data and combination of interrelated choices over some undefined time frame. The rising multifaceted nature of science and innovation requires human services suppliers to know, oversee, screen and include like never before previously. Current techniques for arranging and conveying care are not ready to meet the new desires for patients and families in light of the fact that the information, aptitudes, care alternatives, gadgets, and drugs have propelled more quickly than the medicinal services framework's capacity to convey them wellbeing, viably, and effectively. The potential for blunders of oversight or commission to crawl into the procedure is extraordinary. Work process investigation has frequently been utilized with the objective of prosperous effectiveness. Because of monetary weight and motivating forces driving supplier associations, limiting slack time has turned out to be critical (Steinwachs et.al., 2008, Smith et.al., 2006)
Understanding Error
Clinicians' feelings of dread of claims and their self-impression of incompetence could be scattered by hierarchical societies accentuating security instead of fault. To understand what is or isn't thought about prescription related unfavorable occasions, normal definitions must be set up and comprehended. Associations must go to a typical comprehension in regards to MEs, detailing prerequisites, and dangers to catch and follow up on mistake potential inside their own drug use frameworks. The potential advantages of intra-institutional and Web-based databases may help drug specialists and different suppliers to avoid comparative dangers and advance patient security (Wolf et.al., 2008). These meanings of ADE, PADE, ADR give the accompanying experiences with respect to untoward occasions and drug use:
• MEs are viewed as preventable while unfriendly medication responses are for the most part are definitely not.
• If a mistake happens, however is hindered by somebody simultaneously, it probably won't result in an unfriendly occasion. These potential untoward occasions are frequently alluded to as close misses.
• Capturing data with respect to close misses could yield indispensable data in regards to framework execution
Identifying Risk
Two approaches to deal with the issue of human frailty are conceivable: the individual and the framework approach. The individual methodology accentuations on the blunders of people, charging them for absent mindedness, messiness or good shortcoming. The framework approach focuses on the conditions under which people work and endeavors to construct barriers to deflect mistakes or relieve their belongings. Medicinal services experts are human and can commit errors. Announcing a mistake is frequently viewed as expert disappointment or carelessness and is trailed by authorize or punishment of the people included. Meds are characteristically poisonous, and there is a hazard to taking them and, maybe, not taking them. Each time a specialist endorses an item, a treatment chance versus advantage must be surveyed. In the event that a patient takes recommended prescriptions in an unexpected strategy in comparison to endorsed or if over-the-counter items and elective operators are included, there are extra dangers. Symptoms and heartbreaking uncommon responses are additionally hard to foresee. This outcomes in social insurance laborers stressing always over the ever-present truth of mistake. Lamentably, in numerous associations, the reaction to blunder focuses on the general population as opposed to the framework engaged with the generation of a mistake (Smith et.al., 2006; Pietra et.al., 2005). Reason has identified that there are a variety of defenses put into systems to provide the following functions:
• Create comprehension or familiarity with dangers
• Give direction on the best way to work securely
• Provide cautions and admonitions when hazard or threat is clear
• Place obstructions among risks and people or different frameworks
• Restore framework to a protected state when conditions are not ordinary
• Contain or killed risks if the boundary isn't satisfactory
• Establish techniques for getaway and protect should risk regulation come up short
Targeting Medication Safety at The Microsystem Level
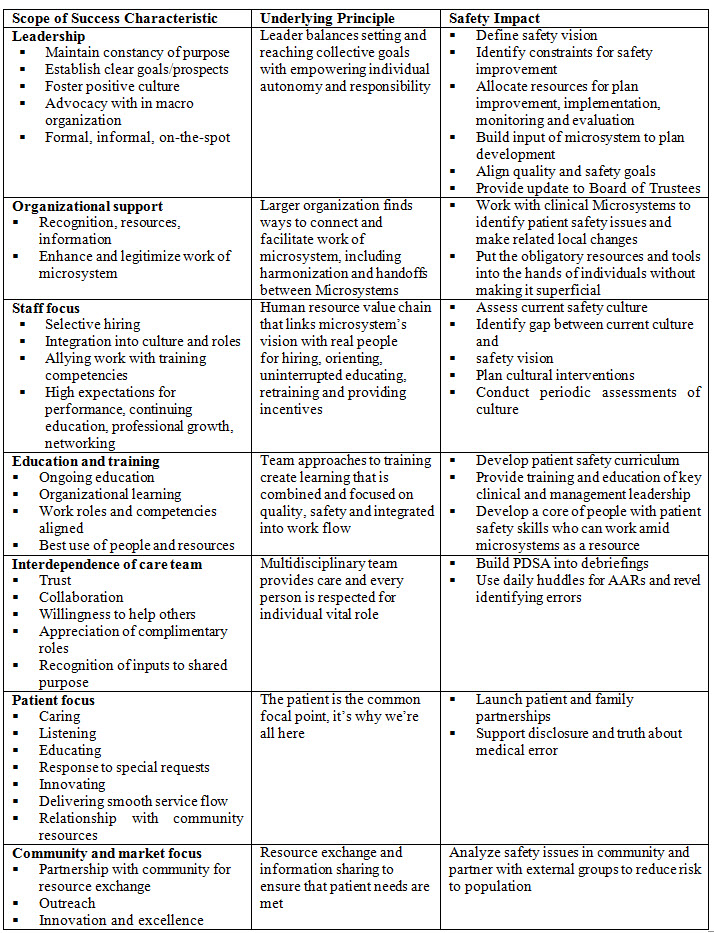
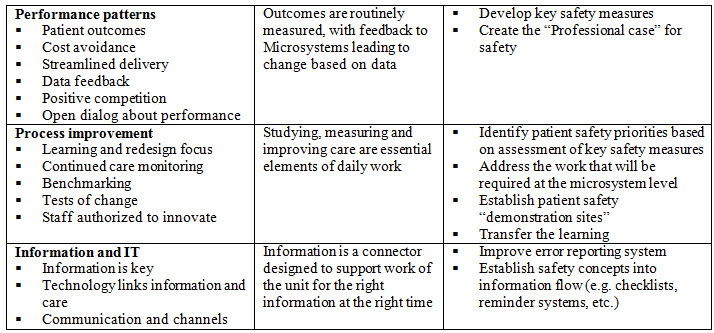
Nelson and colleagues suggest that understanding and nurturing clinical microsystems (Table 1) may create an opportunity for leverage toward the goal of a safety and more effective health care system (Nelson et.al., 2002).
Table 1. Scope of Ten Success Characteristics, Underlying Principles, and Safety Impact
Collaboration Across the Medication Use Process
Collaboration is basic to decrease tolerant hazard in the drug use process. Human services suppliers inside the association need to comprehend and distinguish how these parts capacity and who is engaged with making these means safe. Clear thought of the basic wellbeing issues at every single one of these means are of specific importance in light of the fact that the essential objective of antagonistic occasion distinguishing proof is unfavorable occasion avoidance. Each progression can be viewed as a hazard point and gives chances to inside balanced governance. At each progression in the drug use process, usually accepted doctors, attendants, drug specialists, and other human services suppliers in the affiliation assume a job in patient assessment (Kohn et.al., 2000). This assessment would incorporate gauging understanding qualities, prescription choice, simultaneous meds, drug measurement determination, and medicine organization techniques reasonable for the condition to be dealt with. The present arrangement of endorsing, apportioning, directing, and observing, be that as it may, frequently puts the responsibility on the person to abstain from committing the error (Hughes et.al., 2008; Thomas et.al., 2003) Because this expectation seems unreasonable, organizations should focus efforts to improve medication use safety by using a systems-based approach that identifies:
• Errors that occur most often
• Possible root causes of errors
• Error preclusion strategies to make it harder for the same or similar errors to occur
• If the organization has a system that makes it harder to commit an error, it will be more difficult for errors to go on undetected and for harm to come to patients (Smith et.al., 2006)
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
System Failures in the Medication Use Process
Varieties of systems failures have been identified in hospitals that have studied factors associated with adverse events (Smith et.al., 2006). These system failures are listed below:
• Deficiencies in medicine learning, including endorsing of erroneous meds, portions, structures, recurrence, or courses of organization
• Failure to confirm the character or portion of prescription managed, regularly because of twin bundling or similitudes between medicine names
• Inaccessibility of patient data including research facility test results, momentum prescriptions, and data on the patient's flow condition
• Incorrect recording of requests, regularly because of indecipherability of the doctor's penmanship
• Failure to note known prescription sensitivities
• Inefficient arrange following, making it hard to decide when a prescription has been given, missed/ceased or changed
• Poor correspondence between administrations, including in the midst of medical attendants and drug specialists
• Improper utilization of organization gadgets
• Lack of steady dosing calendars or dismissal of existing guidelines
• Lack of predictable framework for drug dispersion
• Lack of predictable system crosswise over units
• Errors in planning of intravenous prescriptions (when performed in the patient consideration zone)
• Poor data exchange when patients are moved starting with one patient consideration zone then onto the next
• Inadequate or anecdotal framework for settling clashes identified with drug orders
• Lack in staffing or work assignments prompting intemperate remaining burdens, conflicting accessibility of staff or insufficient administration
• Lack of input and follow-up data on watched untoward medication occasions
Classification of Medication Errors
The most ideal approach to see how medication errors occur and how to forestall them is to think about their arrangement, which can be logical, modular, or mental. Relevant arrangement manages the explicit time, place, meds, and individuals concerned. Modular characterization inspects the manners by which mistakes happen (e.g. by oversight, replication, or substitution). Be that as it may, characterization dependent on mental hypothesis is to be picked, as it clarifies occasions as opposed to simply relating them. Its bad mark is that it focuses on human instead of frameworks wellsprings of blunders. These arrangements have been talked about in detail somewhere else (Reason et.al., 1990; Ferner et.al., 2006)
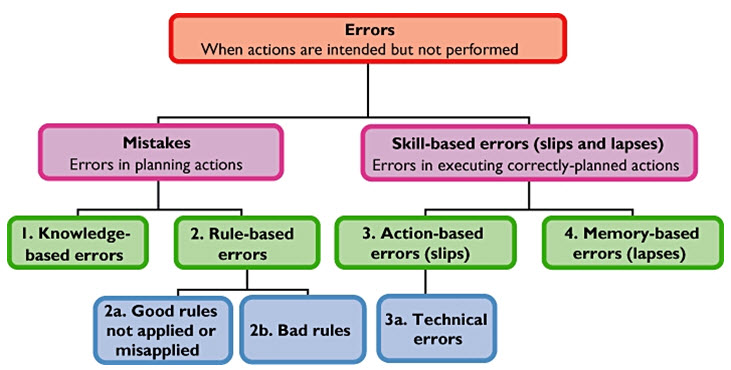
Figure: The classification of medication errors based on a psychological approach [11]
Mistakes can be separated into (i) knowledge-based errors and (ii) rule-based errors. Failures of skill can be divided into (iii) action-based errors ('slips', including technical errors) and (iv) memory-based errors (‘lapses’). Knowledge-based errors can be related to any type of knowledge, general, specific, or expert. It is general knowledge that penicillin’s can cause sensitivity reactions; knowing that your patient is sensitive to penicillin is specific knowledge; knowing that co-fluampicil contains penicillins is expert knowledge. Negligence or ignorance of any of these facts could lead to a knowledge-based error. Rule-based errors can further be categorized as (a) the misapplication of a good rule or the failure to apply a good rule; and (b) the application of a bad rule. An action-based error is defined as ‘the performance of an action that was not what was intended’. A slip of the pen, when a doctor intends to write diltiazem but writes diazepam, is an example. Technical errors form a subset of action-based errors. They have been distinct as occurring when ‘an outcome fails to occur or the wrong outcome is produced because the execution of an action was imperfect’. An example is the addition to an infusion bottle of the wrong amount of drug. Memory-based errors occur when something is forgotten; for example, giving penicillin, knowing the patient to be allergic, but forgetting (Norman, 1981; Runciman et.al., 1993; Ferner et.al., 2001).
Prescription and Dispensing Irregularities Worldwide at A Glance
Medication errors are communal in wide-ranging practice and in hospitals. Both errors in the act of writing (prescription errors) and prescribing mistakes due to erroneous medical decisions can result in harm to patients (Giampaolo et.al., 2009). It very well may be expected to endorsing flaws—nonsensical, unacceptable, and remedy mistakes (vain recommending, under endorsing, overprescribing; composing the medicine) (Aronson, 2009). Specialists in US inaccurately recommend anti-infection agents in about 33% of cases. Study discovers the greater part of US populace gets solution yearly and evaluations 'improper' remedies in specialist's office setting at up to 30% (Jessica, 2016). The NHS commits a huge number of endorsing errors and misunderstandings which result 22,300 death per year UK, as per a noteworthy report authorized by the Government (The Independent, 2018). NHS medicine mistakes hoist fears thousands could be passing on a result of 237 million blunders each year, exactly 237 million mistakes are made every year. Mistake rates fluctuated from 7.1 % to 90.5 % for recommending and from 9.4 % to 80 % for organization in the center east (Zayed et.al, 2013). Be that as it may, UAE bans manually written therapeutic solutions because of 7,000 death overall outcome from messy penmanship (Khaleej Times, 2018). Remedy mistakes in LDC nations needs no further talks, as just 13% medication in Bangladesh is sold under solution, an investigation says 96.83% percent of the drug specialist prescribed prescription taking insufficient history (Shuvasis et.al., 2017).
Failure to Give Prescription Orders
The utilization of verbal requests, electronic request transmission through xerox machine, utilization of worldwide medicine requests, for example, continue every single past request give numerous odds to miscommunication. At whatever point conceivable, verbal requests ought to be stayed away from. Just explicit faculty (e.g., doctors, drug specialists, attendants) ought to be permitted to direct and get verbal medicine orders and just in endorsed conditions. Whenever utilized, verbal requests ought to be enunciated gradually and particularly. Troublesome medicine names and guidelines ought to be explained. Equivocalness ought to be cleared up (Drug names can be wrongly changed because of carbon copy or sound alike medications recorded in Table 2). The individual accepting the request ought to decipher the request and afterward quickly read the data back to the prescriber. In the inpatient or long-haul care setting, the prescriber should catchword and confirm the verbal request as quickly as time permits. Numerous human services associations presently use copy transmissions for remedy arrange transmission. Streaked, darkened, or blurred regions and telephone line commotion showing up as irregular markings are regularly present on copy transmissions. Cautious assessment of the duplicate is important to assess if unessential markings meddle with the real request. Recording of remedy arranges as such still can contain indecipherable, vague, or ill-advised shortenings. Inability to compose a solution request can likewise give numerous odds to blunder. At the point when meds are held or continued or persistent consideration is exchanged to another area or supplier, it is imperious that a total audit of prescriptions is happens. Basically, expressing resume all, hold all, or proceed with every single past drug isn't satisfactory practice (Wakefield et.al., 2008; Simonian, 2008; Hsu et.al., 2015). In any case, clinical consideration has turned out to be continuously subject to CPOE frameworks. No investigation has detailed the unfavorable impact of CPOE on doctors' capacity to handwrite remedies. The unintended shutdown of a long-running CPOE framework may results that doctors neglect to handwrite immaculate medicines in the advanced period. The alternate courses of action for PC disasters at social insurance offices may incorporate planning of remain solitary e-recommending programming with the goal that the administration deferral could be kept to the scarcest. Be that as it may, supervision on recommending ought to remain a fundamental piece of restorative training (Timothy, 2002).
Table 2. Examples of Look Alike and Sound Alike Drugs

Error Potential in The Prescribing Phase
The three most basic types of prescribing mistakes incorporate dosing mistakes, endorsing drugs to which the patient had an unfavorably susceptible history, and blunders including the endorsing of wrong measurements shapes. In the models recorded, convenient access and utilization of data is fundamental to evade unfavorable medication occasions. In spite of the fact that not a panacea, utilization of a mechanized prescription request passage framework can essentially add to the aversion of medicine mistakes (SA Health, 2012). The type of health care information that is best suited for computerization includes:
• General information storage (e.g., patient or medication information, retrieval)
• Repetitive functions (e.g., dosage guidelines, medication names, sensitivity information)
• Complex processes that depend on reproducible results
• Items where legibility is important
• Items that require timely attention
• Items where accuracy is vital.
Guidelines for Prescribers
The following guidelines are recommended for prescribers when writing directions for drug use on their prescription orders:
1. The name and strength of the drug dispensed will be recorded on the prescription label by the pharmacist unless otherwise directed by the prescriber.
2. Whenever possible, specific times of the day for drug administration should be indicated. (For example, take one capsule at 9:00 AM, 1:00 noon, and 10:00 PM is preferable to take one capsule three times daily. Likewise, take one tablet two hours after meals is preferable to take one tablet after meals.)
3. The use of potentially puzzling abbreviations, ie, qid, qod, qd, etc, is discouraged.
4. Vague instructions such as Take as necessary or Take as directed which are confusing to the patient are to be avoided.
5. If dosing at specific intervals around-the-clock is therapeutically significant, this should specifically be stated on the prescription by indicating appropriate times for drug administration.
6. The symptom, indication, or the intended effect for which the drug is being used should be included in the instructions whenever possible. (For example, take one tablet at 8:00 am and 8:00 pm for high blood pressure, or Take one teaspoonful at 9:00 AM, 11:00 AM, 4:00 PM, and 7:00 PM for cough.)
7. The Metric System of weights and measures should be cast-off.
8. The prescription order should indicate whether or not the prescription should be renewed and, if so, the number of times and the period of time such renewal is authorized. Proclamation such as Refill prn or Refill ad lib are discouraged.
9. Either single or multi-drug prescription forms may be used when appropriately designed, and pursuant to the desires of local medical and pharmaceutical societies.
10. When institutional prescription blanks are used, the prescriber should print his/her name, telephone number and registration number on the prescription blank (La Caze, 2018; Jitu et.al., 2010; Veronin, 2011).
Guidelines for Pharmacists
1. Pharmacists should include the following information on the prescription label: name, address and telephone number of pharmacies; name of prescriber; name, strength and quantity of drug dispensed (unless otherwise directed by the prescriber); directions for use; prescription number; date on which prescription is dispensed; full name of patient and any other information required by law.
2. Instructions to the patient regarding directions for use of medication should be concise and precise, but readily understandable to the patient. Where the pharmacist feels that the prescription order does not meet these criteria, he should attempt to clarify the order with the prescriber in order to prevent confusion. Verbal reinforcement and/or clarification of instructions should be given to the patient by the pharmacist when appropriate.
3. For those dosage forms where confusion may develop as to how the medication is to be administered (for example, oral drops which may be wrongly imparted in the ear or suppositories which may be wrongly administered orally), the pharmacist should clearly indicate the intended route of administration on the prescription label.
4. The pharmacist should include an expiration date on the prescription label when suitable.
5. Where special storage conditions are required, the pharmacist should indicate proper instructions for storage on the prescription label (NABP; Texas State Board of Pharmacy; Cheung et.al., 2009)
Error Potential in the Dispensing Phase
A case of the previous sort was an investigation in a UK doctor's facility in which the scientists utilized semi-organized meetings of drug store staff about self-detailed administering blunders. The most well-known causes referenced were: being occupied (21%), being short-staffed (12%), being liable to time requirements (11%), exhaustion of human services suppliers (11%), interferences amid administering (9.4%), and SALAD (8.5%) [30]. The dispensing process has both mechanical and judgmental components. As a result, preclusion of dispensing errors will require a wide-spread approach including evaluation of:
• Work environment: workload, interruptions, physical location of service, hours of operation
• Inventory management: outdated or unused products, SALAD, clutter, labeling, procuring of unit of use products
• Information resources: available references, apprises, consultants, computer or decision support technology
• Performance evaluation: evaluation of staff proficiency and practice skill, knowledge and behaviors, cross-checking redundancies
• Patient involvement: patient education and review with show and tell techniques
Several precarious steps have been advocated for improving dispensing accuracy:
• Secure or sequester high-risk medications
• Develop and implement standardized storage procedures
• Reduce distraction potential and advance workflow in dispensing environment
• Use reminders (labels, computer alerts) to prevent look-alike, sound-alike mix-ups
• Keep prescription order, label, medication and the medication container together throughout dispensing process
• Accomplish a final check on prescription content including verification with original prescription order and label
• Enter a manufacturer identification code into the computer profile and on prescription label
• Accomplish a final check on the prescription label, if possible, using automation such as bar-coding
• Provide patient counseling (Mendes et.al., 2018)
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Error Potential in the Administration Phase
A cross sectional study by Mendes et.al in a university hospital emergency (São Paulo) in 2018 reveals no hand hygiene and use of aseptic technique in more than 70% and 80% respectively. Upon administration, no hand hygiene and no use of aseptic technique in more than 80% and around 85% respectively. In more than 30% of observations, there was more than one medication at the same time for the same patient, of which approximate 18% were compatible, more than 55% and 25% were incompatible and were not tested, according to the Micromedex database, respectively (Weant et.al., 2014). However, the administration phase, serves as a last final check on processing the entire medication order itself and includes:
• Evaluating the written order for appropriateness and completeness
• Ensuring appropriate indication for use
• Evaluating and interpreting use of terminology and order method (abbreviation, units of measure, use of verbal orders)
• Dosing calculation or verification
• Identification of the patient
• Timing of treatment in context of other therapies
• Preparation and possibly dispensing of medication
• Correct use of medication devices
• Patient education
• Documentation of treatment
Medication Error-Prevention Strategies
• Elimination of handwritten medical records and physician orders/ Computerized provider-order entry systems
• Institute fail-safe tracking of medications and laboratory tests to confirm that patients receive correct medications and tests on time
• Automated dispensing cabinets
• Implement bar-coding
• Establish protocols and guidelines that outline standardized practices
• Provide all medications in unit dose packaging, ready for patient administration
• Standardize medication procedures such as protocols for the use of hazardous medications, medication terminology, and medication names
• Make it difficult for someone to do something wrong by error proofing
• Medication reconciliation
• Make relevant patient information available at the point of patient care
• Advance the patient’s knowledge about treatment (McLeod et.al., 2015)
Recommendations for Prescribing Improvements
Many opportunities exist to improve the safety of the medication use process. The prescribing phase of the medication use process, however, encompasses the majority of medication errors that result in preventable ADEs. The knowledge that ADEs can be prevented compels organizations to identify the factors or system failures that contribute to the errors in the prescribing phase. Such factors identified in the prescribing phase include:
• Accessibility of medication information at time of prescribing
• Access to patient information at time of prescribing
• Accessibility of dosing information at time of prescribing
• Accessibility of sensitivity information at time of prescribing
• Accuracy or extensiveness of order by prescriber
• Legibility of handwriting
• Use of abbreviations
• Use of decimals in expressions of weight and measure
• Use of varied units of measure
• SALAD
Changing Systems Within Organizations
The following items have routinely been identified as a top 10 list for improvement in the literature:
• Improving knowledge about medications (availability, access and timeliness)
• Dose/identity tracking of medications (process understanding of distribution)
• Available patient information (availability, access, accuracy and timeliness)
• Order transcription (elimination of process)
• Allergy defense (hard stop capabilities, access to patient information)
• Medication order tracking (streamlining and effective communication of patient needs)
• Communication (patient information, system performance, medication use)
• Device use (standardization and competency regarding use)
• Standardization of medication dose and distribution
Steps for Conducting a Root Cause Analysis
There are several key features for health care organizations to consider as the conduct a root cause analysis:
• Identify a multidisciplinary team to assess the error, failure, or adverse event of interest
• Establish a way to communicate findings and data elements required to conduct the analysis
• Create a plan with target dates, responsibilities, and measurement/data collection strategies required for the investigation
• Define all elements of the process and issues clearly
• Brainstorm all possible causes or potential causes
• Identify interrelationships of causes or potential causes
• Sort, analyze and prioritize cause list
• Determine which processes and systems are part of the investigation
• Determine special and common causes
• Begin the design and implementation of the change while engaging in the root cause analysis
• Repeat each of the steps listed previously as appropriate
• Focus on being thorough (Ask why) and credible (Be consistent, dig deep, and leave no stone unturned!)
• Target system improvement, particularly the larger systems
• Redesign to eliminate root cause(s)
• Measure and assess new design
Barriers Associated with Safety Improvement
There are numerous reasons why associations battle with enhancing security inside their association. Regularly, conventional techniques, for example, prescription blunder or unfavorable medication occasion detailing are unwieldy. Associations have not satisfactorily characterized the procedure, the extent of gathering, and individuals from the medicinal services group don't comprehend why there is a need to gather and talk about the information. Many engaged with the announcing end of the procedure never find out about the data gathered from the investigation. Furthermore, information accumulation and talk about drug mistakes or antagonistic occasions are frequently divided. Drug store may gather and talk about a portion of the information, while nursing might be in charge of different parts and hazard the board or QA may get included for different issues. Accordingly, disappointment happens because of an absence of correspondence, coordination, and information. Documentation frameworks are additionally lumbering and regularly don't fit in well with other everyday consideration duties. What happens with every one of these occasions announced? Frenzy that people will be reprimanded for the blunder and that corrective move will be made additionally restricts singular investment all the while. Having an arrangement and an authoritative comprehension of the point with respect to security enhancement is fundamental. Numerous parts of the social insurance group add to the utilization of meds inside the association. All individuals inside the association must know about the significance of drug use security, aware of the potential for blunder and their job in deflecting it and what the association has set up to guarantee that wellbeing is a need. Absorption all things considered and related information with respect to prescription use is required. The reconciliation of existing information, including ADR, drug mistake, drug store/nursing intercessions, and medicine communication information, into one association wide database is the way to a viable ADE quality administration program. The general effect of the database could be estimated by analyzing the effect that the decreased rate of ADEs has on wellbeing results: clinical, monetary, quiet fulfillment, and wellbeing status results. Explicit objectives for antagonistic occasion enhancement exercises for the most part incorporate:
• Increase documentation
• Aggregate data effectively
• Organizational education and training regarding prevention and detection
• Use data to improve the medication use system
• Minimize patient risk
• Maximize health outcomes
• Create an open and authentic environment where there is a focus on system improvement and reporting
• Remove focus on individual and punitive process
• Meet regulatory standards
Many groups have identified methods to improve the safety of the medication use process. National and local groups have strategies to share and stories to tell. It is important to learn and replicate best practice and build on the success of others (Alduais et.al., 2014; Handler et.al., 2007; Hartnell et.al., 2012; Haw et.al., 2014; Koohestani, 2009).
Sources of Learning About Patient Safety
• The Agency for Healthcare Research and Quality (AHRQ)
• The American Hospital Association (AHA)
• Anesthesia Patient Safety Foundation (APSF)
• Annenberg Patient Safety Conferences
• Institute for Healthcare Improvement (IHI)
• Institute for Safe Medication Practices (ISMP)
• Joint Commission on Accreditation of
• Healthcare Organizations (Joint Commission, JCAHO)
• Leapfrog Group
• Malcolm Baldrige National Quality Program
• Massachusetts Coalition for the Prevention of Medical Errors
• Minnesota Hospital and Healthcare Partnership (MHHP)
• National Academy for State Health Policy (NASHP)
• National Coalition on Health Care (NCHC)
• National Committee for Quality Assurance (NCQA)
• National Patient Safety Foundation (NPSF)
• National Quality Forum (NQF)
• United States Pharmacopeial Convention (USP)
Role of Patients in Medication Errors
This zone is moderately under-looked into and there stay a few unanswered inquiries. Little is thought about how patients comprehend sedate related issues or how they make attributions of unfavorable impacts. Some exploration recommend that patients' psychological models of unfriendly medication responses bear a cozy relationship to models of sickness discernment. Ongoing NICE rules prescribe that experts ought to inquire as to whether they have any worries about their drugs, and this methodology is probably going to yield data helpful for the recognizable proof of medicine mistakes (Britten, 2009).
CONCLUSION
The way to more secure prescription use and enhancements in patient wellbeing isn't about a goal. This is an adventure that must include iterative learning. There are no supreme arrangements, no mysterious declarations that will instruct the calling of drug store to settle the framework. The issues it countenances won't be tackled by the dimension of reasoning that made them. The calling is compelled to think about new methodologies, new learning and to think about mindsets, acting and being that are outside our customary methodologies. At last, the judge of the nature of work, the administrations conveyed and the results of consideration is an inexorably very much educated patient, and also their payors and controllers from general society and private divisions. Concentrate on patient needs and needs, less on how we do it around here.
REFERENCES
1. Aronson J. K. Medication errors: what they are, how they happen, and how to avoid them QJM Volume 102, Issue 8, 1 August 2009, Pages 513–521, https://doi.org/10.1093/qjmed/hcp052
2. Alduais, A.M., Mogali, S., Shabrain, B.A., Enazi, A.A., & Al-awad, F. (2014). Barriers and strategies of reporting medical errors in public hospitals in Riyadh city : A survey-study. IOSR Journal of Nursing and Health Science (IOSR - JNHS) e - ISSN: 2320 – 1959.p - ISSN: 2320 – 1940 Volume 3, Issue 5 Ver. III (Sep. - Oct. 2014), P P 72 – 85
3. Britten N. Medication errors: the role of the patient. Br J Clin Pharmacol. 2009 Jun; 67(6): 646–650. doi: [10.1111/j.1365-2125.2009.03421.x] PMID: 19594532
4. Cheung K, Marcel LB, De Smet AGMP. Medication errors: the importance of safe dispensing. Br J Clin Pharmacol. 2009 Jun; 67(6): 676–680. doi: [10.1111/j.1365-2125.2009.03428.x] PMID: 19594537
5. Ferner RE, Aronson JK. Clarification of terminology in medication errors: definitions and classification. Drug Saf. 2006; 29(11):1011-22.
6. Ferner RE, Langford NJ, Anton C, Hutchings A, Bateman DN, Routledge PA. Random and systematic medication errors in routine clinical practice: a multicentre study of infusions, using acetylcysteine as an example. Br J Clin Pharmacol. 2001;52:573–7.
7. Flanagan ME, Ramanujam R, Doebbeling BN. The effect of provider- and workflow-focused strategies for guideline implementation on provider acceptance. Implement Sci. 2009;4:71. Published 2009 Oct 29. doi:10.1186/1748-5908-4-71
8. Giampaolo P.V., Pietro M. Medication errors: prescribing faults and prescription errors Br J Clin Pharmacol. 2009 Jun; 67(6): 624–628. doi: [10.1111/j.1365-2125.2009.03425.x] PMID: 19594530
9. Hughes RG; Blegen MA. Chapter 37Medication Administration Safety. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Hughes RG, editor. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.
10. Hsu CC, Chou CL, Chen TJ, Ho CC, Lee CY, Chou YC. Physicians Failed to Write Flawless Prescriptions When Computerized Physician Order Entry System Crashed. Clin Ther. 2015 May 1;37(5):1076-1080.e1. doi: 10.1016/j.clinthera.2015.03.003. Epub 2015 Apr 1. PMID: 25841544
11. Handler SM, Perera S, Olshansky EF, et al. Identifying modifiable barriers to medication error reporting in the nursing home setting. J Am Med Dir Assoc. 2007;8(9):568-74.
12. Hartnell N, MacKinnon N, Sketris I, et alIdentifying, understanding and overcoming barriers to medication error reporting in hospitals: a focus group studyBMJ Qual Saf 2012;21:361-368.
13. Haw C, Stubbs J, Dickens GL. Barriers to the reporting of medication administration errors and near misses: an interview study of nurses at a psychiatric hospital. J Psychiatr Ment Health Nurs. 2014;21(9):797-805. doi: 10.1111/jpm.12143. Epub 2014 Mar 20. PubMed PMID: 24646372.
14. Jeetu G, Girish T. Prescription drug labeling medication errors: a big deal for pharmacists. J Young Pharm. 2010;2(1):107-11.
15. Jessica G. Doctors in US incorrectly prescribe antibiotics in nearly a third of cases The Guardian May, 03 2016
16. Khaleej Times. UAE bans handwritten medical prescriptions 7,000 deaths worldwide result from illegible handwriting. March 6, 2018
17. Kohn LT, Corrigan JM, Donaldson MS, editors. Chapter 8. Creating Safety Systems in Health Care Organizations. To Err is Human: Building a Safer Health System. Institute of Medicine (US) Committee on Quality of Health Care in America. Washington (DC): National Academies Press (US); 2000.
18. Koohestani, Hamid Reza and Baghcheghi, Nayereh. Barriers to the Reporting of Medication Administration Errors among Nursing Students [online]. Australian Journal of Advanced Nursing, The, Vol. 27, No. 1, Sept/Nov 2009: 66-74.
19. La Caze A. Safer dispensing labels for prescription medicines. Aust Prescr. 2018;41(2):46-49.
20. Mendes JR, Lopes MCBT, Vancini-Campanharo CR, Okuno MFP, Batista REA. Types and frequency of errors in the preparation and administration of drugs. Einstein (Sao Paulo). 2018;16(3):eAO4146. Published 2018 Sep 10. doi:10.1590/S1679-45082018AO4146
21. McLeod M, Barber N, Franklin BD. Facilitators and Barriers to Safe Medication Administration to Hospital Inpatients: A Mixed Methods Study of Nurses' Medication Administration Processes and Systems (the MAPS Study). PLoS One. 2015;10(6):e0128958. Published 2015 Jun 22. doi:10.1371/journal.pone.0128958
22. Nelson EC, Batalden PM, Huber TP, et al. Jt Comm J Qual Improv 2002; 28:472.
23. Norman DA. Categorization of action slips. Psychol Rev. 1981;88:1–15.
24. NABP. Report of the Task Force on Uniform Prescription Labeling Requirements. National Association of Boards of Pharmacy • (P) 847/391-4406 • (F) 847/391-4502
25. Pietra LL, Calligaris L, Molendini L, Quattrin R, Brusaferro S. Medical errors and clinical risk management: state of the art. Acta Otorhinolaryngol Ital. 2005 Dec; 25(6): 339–346. PMID: 16749601
26. Reason JT. Human Error. New York: Cambridge University Press; 1990.
27. Runciman WB, Sellen A, Webb RK, Williamson JA, Currie M, Morgan C, Russell WJ. The Australian incident monitoring study. Errors, incidents and accidents in anaesthetic practice. Anaesth Intensive Care. 1993;21:506–19
28. Rodziewicz TL, Hipskind JE. Medical Error Prevention. Treasure Island (FL): StatPearls Publishing; 2018 Jan URL: https://www.ncbi.nlm.nih.gov/books/NBK499956/
29. SA Health. Pharmacist legal obligations when handling, dispensing and supplying drugs of dependence. © 2012 SA Health (Govt. of South Australia). ABN 97 643 356 590. Last Modified: 23 Nov 2018
30. Steinwachs DM; Hughes RG. Chapter 8. Health Services Research: Scope and Significance. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Hughes RG, editor. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr
31. Smith KE, Enright SM. Providing a Framework for Ensuring Medication Use Safety. Chapter 102. Providing a Framework for Ensuring Medication Use Safety. Remington: The Science And Practice Of Pharmacy. Author: Joseph P Remington; Paul Beringer Publisher: Philadelphia: Lippincott Williams & Wilkins, ©2006.
32. Shuvasis S., Tawhid M.H. Evaluation of medicines dispensing pattern of private pharmacies in Rajshahi, Bangladesh. BMC Health Serv Res. 2017; 17: 136. doi: [10.1186/s12913-017-2072-z]. PMID: 28193274
33. Simonian AI. Medication order communication using fax and document-imaging technologies. Am J Health Syst Pharm. 2008 Mar 15;65(6):570-3. doi: 10.2146/ajhp070461. PubMed PMID: 18319505.
34. Thomas JE, Petersen LA. Measuring Errors and Adverse Events in Health Care. J Gen Intern Med. 2003 Jan; 18(1): 61–67. doi: [10.1046/j.1525-1497.2003.20147.x] PMID: 12534766
35. The Independent. NHS medication errors contribute to as many as 22,000 deaths a year, major report shows 23 February 2018
36. Timothy S. L. Prescribing Errors Involving Medication Dosage Forms J Gen Intern Med. 2002 Aug; 17(8): 579–587. doi: [10.1046/j.1525-1497.2002. 11056.x] PMID: 12213138
37. Veronin M. Packaging and labeling of pharmaceutical products obtained from the internet. J Med Internet Res. 2011;13(1):e22. Published 2011 Feb 15. doi:10.2196/jmir.1441
38. Weant KA, Bailey AM, Baker SN. Strategies for reducing medication errors in the emergency department. Open Access Emerg Med. 2014; 6: 45–55. doi: [10.2147/OAEM.S64174] PMID: 27147879
39. Wakefield DS, Ward MM, Groath D, Schwichtenberg T, Magdits L, Brokel J, Crandall D. Complexity of medication-related verbal orders. Am J Med Qual. 2008 Jan-Feb;23(1):7-17. doi: 10.1177/1062860607310922. PubMed PMID: 18187586.Dahl FC, Davis NM. A survey of hospital policies on verbal orders. Hosp Pharm. 1990 May;25(5):443-7. PubMed PMID: 10104823.
40. Website. Texas State Board of Pharmacy. (Tab 30) Operation Standards. Prescription dispensing and delivery. URL: https://www.pharmacy.texas.gov/files_pdf/BN/Aug13/Tab_30.pdf
41. Wolf ZR; Hughes GR. Chapter 35Error Reporting and Disclosure. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Hughes RG, editor. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.
42. Zayed A., Sharon C., Imti C. Medication errors in the Middle East countries: A systematic review of the literature European Journal of Clinical Pharmacology April 2013, Volume 69, Issue 4, pp 995–1008.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









