ABOUT AUTHORS:
Ashutosh Kumar Dubey*[1], Vishal Jackob[1], Srishti Srivastava[1], Anusha Srivastaav[2]
1Institute of Foreign Trade and Management
2Rajiv Academy of Pharmacy
*srishtiiftm@gmail.com
ABSTRACT:
The aim of the study was to determine the developed depression during chemotherapy. Depression is a common symptom in cancer patients, which is difficult to be detected and consequently to be treated. It deteriorates over the the course of cancer treatment, persists long after the end of therapy and influences negatively the quality of life. Early diagnosis of depression consists a matter of great importance for a medical treatment. Patients with depressive symptoms scored significantly higher in behavioral disengagement and self-blame as their coping strategies compared to those who were not depressed. The final rationale for this study was to produce research which could be used to educate oncology nurses to create an awareness of psychological side effects in chemotherapy patients.
REFERENCE ID: PHARMATUTOR-ART-1850
INTRODUCTION:
Depression as a disease should be clearly differentiated from depressive symptoms or depressive moods, which are an integral part of human emotions. There are qualitative as well as quantitative differences between a state of unhappiness in reaction to the adverse events in the world outside, and depression as a disease state. It is essential for doctors, the general public and health planners to understand that depression as a disease, unlike depressive moods, is neither a normal variation of mood nor an appropriate reaction to severe stress. Also, depression does not constitute a failure of "will power" or "weak character" in a person.There are some people who periodically or chronically remain in a depressed state in spite of their having all social privileges and material comforts, severely compromising all their functions, culminating in about 15% of cases in suicide.
Major depression is a common psychiatric disorder among cancer patients and is associated with psychosocial impairment and decreased quality of life. Although some research has explored psychological interventions with cancer patients, outcome studies investigating the benefits of behavior therapy among cancer patients with well diagnosed depression are nonexistent.Depressed cancer patients also experience a more rapid progression of cancer symptoms, increased mortality, more metastasis and pain, and increased medical utilization. Thus, the need to explore effective psychosocial and pharmacological interventions for depressed cancer patients has been highlighted as a pressing need.[1]. Major depression may represent a spectrum of disorders, varying in severity from mild and self-limited conditions to extraordinarily severe, psychotic, incapacitating, and deadly diseases. Physiological and pharmacological modifications of these brain regions may have important behavioral consequences and useful clinical effects regardless of the underlying cause of any mental disorder. Clinical depression must be distinguished from normal grief, sadness, disappointment, and the dysphoria or demoralization often associated with medical illness.[2].In the last 50 years, rapid strides have been made in the treatment of depression. Newer drugs have been discovered with better efficacy, less side-effects and better tolerance, and are being used for short-term and long-term treatment. Besides drugs, non- pharmacological therapies like psychotherapy and cognitive therapy have been found beneficial. In the modern day and age, there is absolutely no reason why people anywhere in the world should continue to suffer from depression.When the negative reactions to life`s situations become repetitively intense and frequent we develop symptoms of depression. Life throws up innumerable situations, which we greet with both negative and positive emotionssuch as excitement, frustration, fear, happiness, anger, sadness, Depressionis prevalent among all age groups, in almost all walks of life. In the last 50 years, rapid strides have been made in the treatment of depression. Newer drugs have been discovered with better efficacy, less side-effects and better tolerance, and are being used for short-term and long-term treatment. Besides drugs, non-pharmacological therapies like psychotherapy and cognitive therapy have been found beneficial. In the modern day and age, there is absolutely no reason why people anywhere in the world should continue to suffer from depression.
When the negative reactions to life`s situations become repetitively intense and frequent we develop symptoms of depression. Life throws up innumerable situations, which we greet with both negative and positive emotionssuch as excitement, frustration, fear, happiness, anger, sadness, Depressionis prevalent among all age groups, in almost all walks of life.
We all go through ups and downs in our mood. Sadness is a normal reaction to life’s struggles, setbacks, and disappointments. Many people use the word “depression” to explain these kinds of feelings, but depression is much more than just sadness. Some people describe depression as “living in a black hole” or having a feeling of impending doom. However, some depressed people don't feel sad at all—instead, they feel lifeless, empty, and apathetic. Rates of depression in women are twice as high as they are in men.[3]
What is depression
Depression is a common mental disorder that presents with depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration. These problems can become chronic or recurrent and lead to substantial impairments in an individual's ability to take care of his or her everyday responsibilities. At its worst, depression can lead to suicide, a tragic fatality associated with the loss of about 850 000 lives every year.
A depressive disorder is a syndrome (group of symptoms) that reflects a sad and/or irritable mood exceeding normal sadness or grief. More specifically, the sadness of depression is characterized by a greater intensity and duration and by more severe symptoms and functional disabilities than is normal. .Depression is a prolonged and persistent state of sadness –
- Pathological/morbid condition.
- Depression is a significant public health problem because of its high prevalence, the suffering, and sometimes death, that it causes.
- Depression leads to considerable dysfunction in all areas of life in an affected person.
- Depression is seen in many medical disorders, and persons with depression are more prone to develop secondary medical disorders.
- Suicide is a major risk during the course of depression.
Despite effective treatment being available, a large number of depressed patients receive no treatment.
Facts about Depression:
a. Depression is common, affecting about 121 million people worldwide.
b. Depression is among the leading causes of disability worldwide.
c. Depression can be reliably diagnosed and treated in primary care.
d. Fewer than 25 % of those affected have access to effective treatments.
Depression can be reliably diagnosed in primary care. Antidepressant medications and brief, structured forms of psychotherapy are effective for 60-80 % of those affected and can be delivered in primary care. However, fewer than 25 % of those affected (in some countries fewer than 10 %) receive such treatments. Barriers to effective care include the lack of resources, lack of trained providers, and the social stigma associated with mental disorders including depression.[4]
Primary care based quality improvement programs for depression have been shown to improve the
- quality of care,
- satisfaction with care
- health outcomes,
- functioning,
- economic productivity,
- household wealth at a reasonable cost
Depression is a common mental disorder, characterized by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy and poor concentration. These problems can become chronic or recurrent, substantially impairing an individual’s ability to cope with daily life. At its most severe, depression can lead to suicide. Most cases of depression can be treated with medication or psychotherapy
Types of Depression:[5]
There are several forms of depressive disorders. The most common and major depressive disorder are following.
Atypical Depression:Atypical depression is a type of depression that overwhelms an individual almost to the point of emotional paralysis. The name atypical depression comes from the fact that many of its symptoms are opposite to those of some severe depressions. For example people with atypical depression tend to overeat and oversleep. In contrast, people with depression can't eat or sleep. People with atypical depression are externally validated. They feel good when people give them positive compliments and they feel bad when someone criticizes them. Their moods change and shift as quickly as the wind depending if they are isolated and lonely or with a group of friends enjoying a night out on the town.
Bipolar Depression:This depression is a mood disorder with manic episodes. Bipolar disorder normally begins in adolescence or early adulthood and continues throughout life. Consequently, those who have it may suffer needlessly for years without treatment. This illness can be effectively treated and must be as it is very serious. Without treatment, marital breakups, job loss, alcohol and drug abuse, and suicide may result from the chronic, episodic mood swings. This is a serious judgment problem. As the manic episode progresses, concentration becomes difficult, thinking becomes more grandiose, and problems develop. Many individuals with bipolar disorder abuse drugs or alcohol during manic episodes, and some of these develop secondary substance abuse problems.
Cyclothymic Disorder:Cyclothymic disorder is when a person has mild and alternating mood swings of elation and depression occurring over a long time period. Because the mood swings are mild, and the elation is often enjoyable, frequently people with cyclothymic disorder do not seek medical help. The periods of elation and depression can last for lengthy periods, such as a few months. Often, a person with cyclothymic disorder has a relative with bipolar disorder, or they may develop bipolar disorder themselves.
Dysthymia Depression:The Greek word dysthymia means "bad state of mind" or "ill humor." As one of the two chief forms of clinical depression, it usually has fewer or less serious symptoms than major depression but lasts longer. Dysthymia refers to a prevalent form of sub threshold depressive pathology with gloominess, anhedonia, low drive and energy, low self-esteem and pessimistic outlook. Although co-morbidity with panic, social phobic and alcohol use disorders has been described, the most significant association is with major depressive episodes. Dysthymia and major depression naturally have many symptoms in common, including depressed mood, disturbed sleep, low energy, and poor concentration. Like major depression, it is more common in women than in men, but it tends to arise earlier in life.
Major Depression:Major depression is a serious medical illness. Unlike normal emotional experiences of sadness, loss, or passing mood states, major depression is persistent and can significantly interfere with an individual's thoughts, behavior, mood, activity, and physical health. Approximately twice as many women as men suffer from major depression. This is partially because of hormonal changes throughout a woman's life: During menstruation, pregnancy, miscarriage and menopause.. Major depression, also known as clinical depression or unipolar depression, is only one type of depressive disorder.
Postpartum Depression:A rare form of depression occurring in women within approximately one week to six months after giving birth to a child. After pregnancy, hormonal changes in a woman's body may trigger symptoms of depression. Tiredness, problems sleeping, stronger emotional reactions, and changes in body weight may occur during pregnancy and after pregnancy. But these symptoms may also be signs of depression. Researchers think the fast change in hormone levels may lead to depression, just as smaller changes in hormones can affect a woman's moods before she gets her menstrual period.
Premenstrual Dysphoric Disorder:This is an uncommon type of depression affecting a small percentage of menstruating women. It refers to the variation of physical and mood symptoms that appear during the last one or two weeks of the menstrual cycle and disappear by the end of a full flow of menses. It is a cyclical condition in which women may feel depressed and irritable for one or two weeks before their menstrual period each month. If you have unpleasant, disturbing emotional and physical symptoms before your monthly menstrual periods and these symptoms disrupt your life and interfere with your usual activities and your relationships with others and the symptoms go away when your flow begins or shortly thereafter, only to return before your next period then this condition is known as Premenstrual Dysphoric Disorder.
Psychotic Depression:This is a more serious form of depression which is frequently seen by psychiatrists though it is rather rare, compared to the wider context of general medical practice. Patients may develop beliefs about themselves and the world, which are false at times bizarrely and obviously so. Psychotic depression has a very low spontaneous remission rate. It responds only to physical treatments (such as antidepressant drugs). The defining features of psychotic depression are:
- More severely depressed mood
- More severe psychomotor disturbance than is the case with melancholic depression
- Psychotic symptoms like either delusions or hallucinations and over-valued guilt ruminations.
Cause of Depression
There is no single known cause of depression. Rather, it likely results from a combination of genetic, biochemical, environmental, and psychological factors.
Research indicates that depressive illnesses are disorders of the brain. Brain-imaging technologies, such as magnetic resonance imaging (MRI), have shown that the brains of people who have depression look different than those of people without depression. The parts of the brain responsible for regulating mood, thinking, sleep, appetite and behavior appear to function abnormally. In addition, important neurotransmitters—chemicals that brain cells use to communicate—appear to be out of balance. But these images do not reveal whythe depression has occurred.
Some types of depression tend to run in families, suggesting a genetic link. However, depression can occur in people without family histories of depression as well.Genetics research indicates that risk for depression results from the influence of multiple genes acting together with environmental or other factors.[6]
In addition, trauma, loss of a lived one, a difficult relationship, or any stressful situation may trigger a depressive episode. Subsequent depressive episodes may occur with or without an obvious trigger.
Some types of depression run in families, indicating that a biological vulnerability to depression can be inherited. This seems to be the case, especially with bipolar disorder. Families in which members of each generation develop bipolar disorder have been studied. The investigators found that those with the illness have a somewhat different genetic makeup than those who do not become ill. However, the reverse is not true. That is, not everybody with the genetic makeup that causes vulnerability to bipolar disorder will develop the illness. Apparently, additional factors, possibly a stressful environment, are involved in its onset and protective factors are involved in its prevention.Thus, a serious loss, chronic illness, difficult relationship, financial problem, or any unwelcome change in life patterns can trigger a depressive episode. Very often, a combination of genetic, psychological, and environmental factors is involved in the onset of a depressive disorder. Stressors that contribute to the development of depression sometimes affect some groups more than others. For example, minority groups who more often feel impacted by discrimination and are disproportionately represented. Socioeconomically disadvantaged groups have higher rates of depression compared to their advantaged counterparts. Immigrants to the United States may be more vulnerable to developing depression, particularly when isolated by language.[7]
The Signs of Depression
Depression is a loss of an important life goal without anyone to blame. Such a loss affects our behavior, our moods or subjective feelings, our skills, our attitudes or motivations, and our physical functioning and health. Several writers Beck,
Behavioral excesses--complaints about money, job, housing, noise, poor memory, confusion, loneliness, lack of care and love... acting out (adolescents), running away from home, rebellious, aggressive... obsessed with guilt and concern about doing wrong, about being irresponsible, about the welfare of others, and about "I can't make up my mind anymore"... crying... suicidal threats or attempts.
Behavioral deficits--socially withdrawn, doesn't talk, indecisive, can't work regularly, difficulty communicating, slower speech and gait... loss of appetite, weight change, stays in bed... less sexual activity, poor personal grooming, and doing less for fun.
Emotional reactions--feels sad, feels empty or lacks feelings of all kinds, tired ("everything is an effort")... nervous or restless, angry and grouchy (adolescents), irritable, overreacts to criticism... bored, apathetic, "nothing is enjoyable," feel socially abandoned and/or has less interest in relationships, sex, food, drink, music, current events, etc.
Attitudes and motivation--low self-concept, lack of self confidence and motivation, pessimistic or hopeless, feels helpless or like a failure, expects the worst... self-critical, guilt, self-blaming, "People would hate me if they knew me"... suicidal thoughts, "I wish I had never been born."
Physical symptoms --difficulty sleeping or sleeping excessively, awaking early... hyperactivity or sluggishness, diurnal moods (worse in the morning)... low sex drive, loss of appetite, weight loss or gain, indigestion, constipation, headaches, dizziness, pain, and other somatic problems or complaints.[6]
Classification, mode of action, adverse reaction[6]
|
S.no |
Class |
Drug |
MOA |
AdR |
|
|
|
|
||
|
1 |
Reversible inhibitors of MAO-A |
Moclobemide Clorgyline |
Selective MAO-A inhibitor |
Insomnia liver damage |
|
2 A
B
|
TricyclicAntidepresson NA+5HT reuptake inhibitors
Predominatly NA reuptake inhibitors. |
Imipramine
Desipramine |
It inhibited NA and 5-HT reuptake into neurons.
It inhibited NA reuptake into neurons. |
Anticolinergic Sedation Sweating Cardiac arrhythmias Jaundice |
|
3 |
Selective serotonin reuptake inhibitor
|
Fluoxetine |
It inhibits the neuronal uptake of 5-HT. |
Drowsiness Insomnia Diarrhoea Epigastric distress. |
|
4 |
Atypical antidepresson |
Trazodone |
It inhibits the neuronal uptake of 5-HT in CNS. |
Headache Nausea Dizziness Drowsiness |
|
|
||||
Depression in children :
It was earlier believed that children and young adolescents are incapable of experiencing depressive symptoms and hence cannot suffer from depression. It is possible that many cases of childhood depression were being treated as school phobia or behavioural or temperamental aberrations.The risk of occurrence of major depression is between 15 and 20% among children and adolescents, which is almost similar to that of adult populations. Complicating the picture, however, is the fact that a large number of children and adolescents suffering from depression have other associated psychiatric illnesses such as anxiety, disruptive behaviour and drug abuse. The symptoms of depression among this group remain largely the same as in an adult group; however, most of the manifestations due to the illness pertain to adjustment with peers and friends, problems in school, and indifferent or deteriorating scholastic performance. Children also appear sad, cry easily, manifest loss of interest and withdrawal, complain of bodily symptoms, and express pessimistic ideas. However, suicide among children has remained infrequent, yet a disturbing rising trend has been observed in the last one decade, and suicide is reported to be the third leading cause of death among adolescents in the western world.
Depression in the elderly :
Depression in the older age group is significant for a variety of reasons. Approximately 20% of elderly people above the age of 60 have some depressive symptoms, but an identifiable diagnosis of depression is made only in 5% of the elderly population. However, depression occurs frequently among the medically ill elderly population where nearly 30% have associated depression. Depression is very common among residents of old age homes also. In spite of its common occurrence, depression among the elderly frequently remains undetected. Very often, depression is attributed to the ageing process and no intervention is sought or provided.
Elderly people have a much higher risk of suicide than the general population. Data from Member Countries of SEAR indicate that suicide rates among the elderly may be lower than in western countries, perhaps because of the protective role of the joint family system. Elderly people in traditional societies do not suffer from isolation and deprivation. However, with social values changing rapidly in the developing countries, elderly people are likely to face increasing stress and strain. With the rapidly increasing elderly population in the countries of this Region, it is imperative that adequate provisions be made for the care of psychiatrically and medically ill elderly people.
Management of depression in cancer patient :
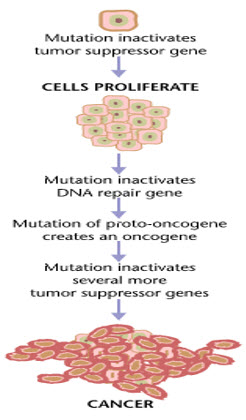
Cancer is the uncontrolled growth of abnormal cells anywhere in a body. The abnormal cells are termed cancer cells, malignant cells, or tumor cells. Many cancers and the abnormal cells that compose the cancer tissue are further identified by the name of the tissue that the abnormal cells originated from. (for example, breast cancer, lung cancer, colon cancer).[7]
Cancer is a class of diseases characterized by out-of-control cell growth. Cancer harms the body when damaged cells divide uncontrollably to form lumps or masses of tissue called tumors (except in the case of leukemia where cancer prohibits normal blood function by abnormal cell division in the blood stream). Tumors can grow and interfere with the digestive, nervous, and circulatory systems, and they can release hormones that alter body function. Tumors that stay in one spot and demonstrate limited growth are generally considered to be benign.[8]
Causes of cancer:
Cancer is ultimately the result of cells that uncontrollably grow and do not die. Normal cells in the body follow an orderly path of growth, division, and death. Programmed cell death is called apoptosis, and when this process breaks down, cancer begins to form. Unlike regular cells, cancer cells do not experience programmatic death and instead continue to grow and divide. This leads to a mass of abnormal cells that grows out of control.
Cancers are primarily an environmental disease with 90-95% of cases attributed to environmental factors and 5-10% due to genetics.[1]Environmental, as used by cancer researchers, means any cause that is not genetic. Common environmental factors that contribute to cancer death include: tobacco(25-30%), diet and obesity(30-35%), infections(15-20%), radiation(both ionizing and non ionizing, up to 10%), stress, lack of physical activity, and environmental pollutants.[9]
Classification, mode of action, adverse reaction[6] :
|
A. |
Drugs acting directly on cells ( Cytotoxic drugs ) : |
||||
|
S. No |
Class |
Drug |
MOA |
Adr |
|
|
|
|
|
|||
|
1. |
Alkylating agents |
Mechlorethamine Cyclophosphaminde Chlorambucil Thio-tepa |
Abnormal base pairing / Cross linking |
Haemodynamic changes,Bone marrow depression |
|
|
2.
|
Antimetabolites Purine Pyrimidine |
5-Fluorouracil Methotrexate6-Mercaptopurine 6-Thioganine |
Inhibit the Conversion of DHFA to THFA |
Bone marrow depression |
|
|
3. |
Vinca Alkaloids |
Vincristine(Oncovin), Vinblastin |
Mitotic inhibitors |
Bone marrow depression, Neurotoxicity |
|
|
4. |
Taxanes |
Pacitaxel, Docetaxel |
It enhance polymerization of tubulin |
Neutropenia |
|
|
5. |
Epipodophyllotoxin |
Etopside |
Arrest cells in the G2 phase |
g.i.t disturbances |
|
|
6. |
Camptothecin analogues |
Topotecan, Irinotecan |
Arrest cells in the G2 phase |
Neutropenia |
|
|
7. |
Antibiotics |
Actinomycin D, Doxorubicin, Bleomycin, Mitomycin C |
Anti tumour |
Bone marrow depression |
|
|
8. |
Miscellaneous |
Hydroxyurea, Procarbazine, Cisplantin, Carboplatin |
Interferes with DNA synthesis |
Neutropenia |
|
|
B |
Drugs altering hormonal milieu : |
||||
|
1. |
Glucocorticoids |
Prednisolone |
GnRH inhibt |
Hyperglycaemia,Peptic ulceration,Glaucoma |
|
|
2. |
Estrogens |
Fosfestrol ,Ethinylestradiol |
Inhibt ER dimerization |
Suppresion of libido, Gynaecomastia |
|
|
3. |
Selective estrogen receptor modulator |
Tamoxifen, Toremifene |
GnRH inhibt |
Decrease libido,vaginal bleeding,dermatitis |
|
|
4. |
Selective estrogen receptor downregulator |
Fulvestrant |
Inhibt ER dimerization |
Decrease libido,vaginal bleeding,dermatitis |
|
|
5. |
Aromatase inhibitor |
Letrozole, Anastrozole |
Inhibit aromatization |
Diarrhoea,dyspepsia, joint pain |
|
|
6. |
Antiandrogen |
Flutamide, Bicalutamide |
Inhibit androgen |
Liver damage,gynaecomastia |
|
|
7. |
5-α reductase inhibitor |
Finasteride, Dutasteride |
Inhibit conversion of testosterone into dihydrotestosterone |
Impotency,decrease libido |
|
|
8. |
GnRH analogues |
Nafarelin, Triptorelin |
Inhibit androgen and endrogen secretion |
Decrease libido,osteoporosis |
|
|
9. |
Progestins |
Hydroxyprogesterone acetate |
Inhibt ER dimerization |
Esophageal reflux,amenorrhoea |
|
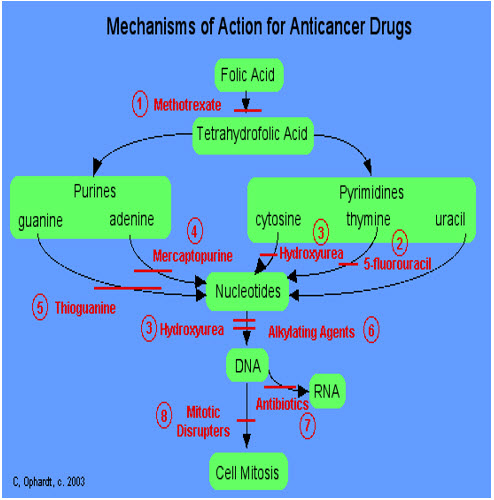
Fig 2 : Mechanisam of action for anticancer drugs :
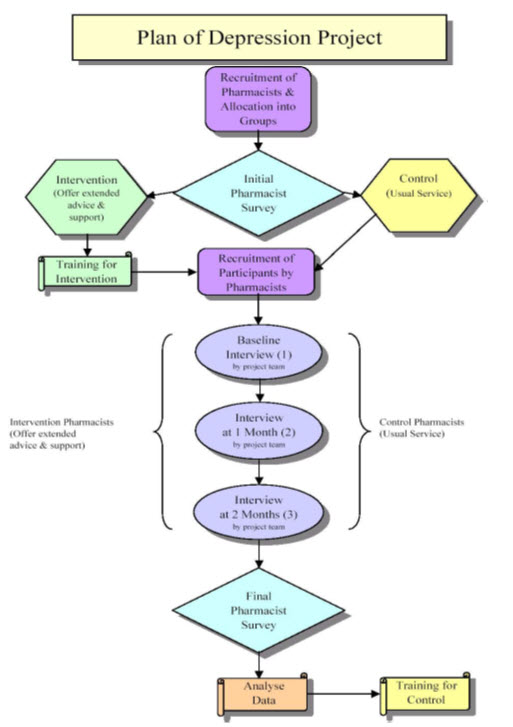
Role of pharmacist :
There is scant knowledge of the involvement of developing country pharmacists in mental healthcare. The World Health Organization (WHO) estimates that 25% of any population will suffer from neuro-psychiatric conditions during their lifetime [10]
Health professionals have identified people with mental illness as among their most challenging patients to manage [11]
Consequently, the primary goal of the pharmacist in mental health provision should be the safety and wellbeing of the patient, ensuring that patients who need medicines receive them and adhere to treatment [12].
Indeed, WHO has acknowledged pharmacists as dynamic members of the mental healthcare team who should assist in improving psychotropic medication use [13].
In developed countries, pharmacists are involved in both in-patient and out-patient psychiatric settings. Pharmacists routinely participate as pharmacotherapy experts and consultants, manage individual patient drug regimens, obtain drug histories, lead patient education discussion groups, and coordinate the use of drug assistance programs. A retrospective chart review has indicated that duties performed by pharmacists in psychiatric settings can improve physician prescribing practices and enhance treatment outcomes [14].
Pharmacists in the United Kingdom play a role at every stage of the patient's recovery, whether patients are being cared for in an acute setting or in the community.
CONCLUSION :
Now a days, cancer is considered to be a chronic disease, causes emotional problems to the patient, induces important changes to the functional capability, the body image and the social or familial role.
Health professionals should be aware of the consequences of depression in all dimensions of patients’ lives who undergo chemotherapy.
Early diagnosis of depression and the cognition of its impact, consist a matter of great importance for the evaluation, the medical treatment and the planning of personal care.
The survey demonstrated that local pharmacists in community practice play any significant role in the management of mental illness, were restricted by several barriers in involving themselves in the management of mental illness and would welcome regular workshops on mental health
REFERENCE:
1. en.wikipedia.org/wiki/depresson
2. Goodman & Gilman’s. (2008) “ Manual of Pharmacology and Therapeutics” McGraw-Hill Companies, United States of America.,pp 289.
3. helpguide.org/mental/depression_signs_types_diagnosis_treatment.htm
4. ncbi.nlm.nih.gov/pubmed/979301
5. Brown E, Harris T. Social Origins of Depression. London: Tavistok; 1978.
6. Tripathi KD (2008) ‘Essentials of Medical Pharmacology’Jaypee Brothers Medical Publishers, New Delhi,6th edition.,pp New Delhi page no.439-452,820-834.
7. medicinenet.com/cancer/page2.htm.
8. medicalnewstoday.com/info/cancer-oncology/
9. en.wikipedia.org/wiki/Cancer
10. Sirey JA, Bruce ML, Alexopoulos GS: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services 2001, 52:1615-1620.
11. WHO: The world health report 2001 - Mental Health: New Understanding, New Hope. 2001 [who.int/whr/2001/ chapter1/en/index.html].
12. Bryant SG, Guernsey BG, Pearce EL: Pharmacists' perceptions of mental health care, psychiatrists, and mentally ill patients. American Journal of Hospital Pharmacy 1985, 42:1366-1369.
13. WHO: Improving access and use of psychotropic medicines. [bipolarworld.net/pdf/ Improving_Access_Use_Psychotropic_Medicine.pdf].
14. Finley PR, Crismon ML, Rush JA: Evaluating the Impact of Pharmacists in Mental Health: A Systematic Review. Pharmacotherapy 2003, 23:1634-1644.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org









