ABOUT AUTHOR:
Akshay Rajgaria
Kanak Manjari Institute of Pharmaceutical Sciences
akshaykrish2007@gmail.com
ABSTRACT:
Darier’s disease, also known as keratosis follicularis or dyskeratosis follicularis, is a rare disorder of keratinization. It is an autosomal dominant genodermatosis with high penetrance and variable expressivity. Its manifestation appears as hyperkeratotic papules, primarily affecting seborrhea areas on the head, neck, and thorax and less frequently on the oral mucosa. When oral manifestations are present, the palatal and alveolar mucosas are primarily affected.
REFERENCE ID: PHARMATUTOR-ART-1996
INTRODUCTION:
Darier's disease (DAR), also known as Darier disease, Darier–White disease, Dyskeratosis follicularis and Keratosis follicularis, is an autosomal dominant disorder discovered by French dermatologist Ferdinand-Jean Darier. Darier's is characterized by dark crusty patches on the skin, sometimes containing pus. The crusty patches are also known as keratotic papules, keratosis follicularis or dyskeratosis follicularis.The disease is caused by mutations in the ATP 2A gene, which encodes the sarcoendoplasmic reticulum Ca2+ATPase.
PATHOPHYSIOLOGY:
Mutations in the gene ATP2A2 cause keratosis follicularis (Darier disease). ATP2A2, located on 12q23-24.1, encodes the sarcoplasmic/ endoplasmic reticulum Ca2+ -ATP isoform 2 protein (SERCA2), which is a calcium pump. This pump maintains a low cytoplasmic Ca2+ level by actively transporting calcium ions from the cytosol into the lumen of the endoplasmic reticulum. Although more than 113 familial and sporadic mutations in ATP2A2 have been identified in keratosis follicularis (Darier disease) patients, attempts at genotype-phenotype correlation have not been successful. Family members with confirmed identical ATP2A2 mutations can exhibit differences in the clinical severity of disease, suggesting that other genes or environmental factors affect the expression of keratosis follicularis (Darier disease) A wide variety of ATP2A2 mutations in Darier disease have been identified.
The mechanisms by which specific ATP2A2 mutations impact the function of the ATP2A2 protein have been investigated using an in vitro model. Investigators transfected a fibroblast cell line with 51 different mutations seen in keratosis follicularis (Darier disease) pedigrees. The investigators found that the resultant transfected cells showed defects in ATP2A2 protein expression (15 mutants), ATP hydrolysis (29 mutants), calcium transport (4 mutants), and calcium binding and kinetics (3 mutants). In a different study, in which researchers systematically analyzed mutations identical to those found in patients with Darier disease, mutant SERCA2 protein aggregates were found to cause stress to the endoplasmic reticulum, subsequently inducing cell apoptosis Thus, diverse biochemical mechanisms are responsible for altered protein function.
Although expressivity is variable, penetrance of keratosis follicularis (Darier disease) is high, estimated at 95%. Because the disease-causing mutations inATP2A2 affect functional domains of the gene, the mechanism of autosomal dominant transmission is believed to be haplo insufficiency, in which a single wild-type functioning ATP2A2 is insufficient to prevent disease. No unique phenotype for genetic homozygote has been reported.
Abnormal keratinocyte-keratinocyte adhesion and aberrant epidermal keratinization are the primary histological features of keratosis follicularis (Darier disease). Electron microscopy reveals loss of desmosomes (epithelial intercellular junctions formed by membrane and sub membrane protein complexes), breakdown of desmosome-keratin intermediate filament attachment, and perinuclear aggregates of keratin intermediate filaments. The mechanism by which decreased activity of the SERCA2 calcium pump leads to these changes is still under investigation.[However, a significant correlation exists between the clinical presentation of keratosis follicularis (Darier disease) and the intensity of histologic features.
Some preliminary studies of keratosis follicularis (Darier disease) have suggested that alterations in calcium regulation may affect the synthesis, folding, or trafficking of desmosomal proteins. In particular, studies have revealed that keratosis follicularis (Darier disease) keratinocytes displayed abnormal trafficking of the desmosomal protein desmoplakin and abnormal expression of cytokeratins 10 and 14. Alternatively, another hypothesis, based on a canine model of keratosis follicularis (Darier disease), is that keratosis follicularis (Darier disease) calcium dysregulation leads to impaired control of cell cycle checkpoints, leading to increased epidermal sensitivity to skin trauma and subsequent keratinocyte apoptosis. Two particular ATP receptors recently been reported to abnormally localize in vivo in keratosis follicularis (Darier disease) and are speculated to play a role in apoptosis as well as abnormal calcium signaling.
CHARACTERISTICS:
DAR affects both men and women and is not contagious. The disease often starts during or later than the teenage years, typically by the third decade. Short stature is common. The symptoms of the disease are thought to be caused by an abnormality in the desmosome-keratin filament complex leading to a breakdown in cell adhesion.
Worldwide prevalence is estimated at between 1: 30,000 and 1: 100,000. Case studies have shown estimated prevalence by country to be 3.8: 100,000 in Slovenia, 1: 36,000 in north-east England, 1: 30,000 in Scotland, and 1: 100,000 in Denmark
It most commonly affects the chest, neck, back, ears, forehead, and groin, but may involve other body areas. The rash associated with Darier's disease often has a distinct odor. Palms & soles may become thickened, intra oral papules can be found. Finger nails become fragile and this helps in diagnosis of the disease. The rash can be aggravated by heat, humidity, and exposure to sunlight. In some cases, sunlight makes it better, especially in the forehead.
Minor forms of the disease are the most common, and may remain undiagnosed throughout life. These consist mainly of minor rashes without odor that are aggravated by heat, humidity, stress and sunlight. Poorly formed fingernails containing vertical striations are diagnostic.
A recent study examined neuropsychiatric conditions in a non-random sample of 100 British individuals assessed as having DAR. There were high lifetime rates for mood disorders (50%), including depression (30%), bipolar disorder (4%), suicidal thoughts (31%) and suicide attempts (13%), suggesting a possible common genetic link. Scattered case studies also suggest a possible link to learning disorders (not yet confirmed).
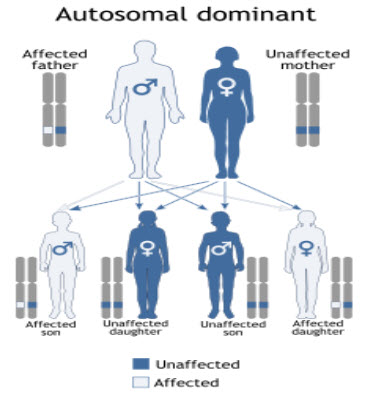
GENETICS: Darier's disease has an autosomal dominant pattern of inheritance. DAR is inherited in an autosomal dominant manner, which indicates that the defective gene responsible for a disorder is located on an auto some, and only one copy of the gene is sufficient to cause the disorder, when inherited from a parent who has the disorder. The disorder is caused by a mutation in the gene ATP2A2. Family members with confirmed identical ATP2A2 mutations can exhibit differences in the clinical severity of disease, suggesting that other genes or environmental factors affect the expression of Darier's disease. With the discovery of the ATP2A2 gene, performing genetic tests to confirm the diagnosis of Darier's disease is now possible.
DIAGNOSIS: Usually Darier disease is diagnosed by its appearance and the family history, but it is often mistaken for other skin problems.
The symptoms and signs of Darier disease vary between individuals. Some have very subtle signs that are found only on careful inspection. Others have extensive lesions. In an affected person the severity of the disease can fluctuate over time.
Skin rash: The skin lesions are greasy, scaly papules (small bumps) which tend to occur over the oily areas of the face (scalp margins, forehead, ears, around the nostrils and sides of nose, eyebrows, and beard area), neck, and central chest and back. The flexures (within natural folds of the skin around joints such as armpits and groins) and skin under breasts and between buttocks are also commonly affected. The papules have a firm, harsh feel like coarse sandpaper and may be skin colored, yellow-brown or brown in color. If several of the small papules grow together they may form larger warty lesions which can become quite smelly within skin folds. The scalp is often affected with a heavily crusted rash which can be similar to seborrhea dermatitis but is usually harsher to the touch. Some patients may have flat, freckle-like lesions. Others may have very large, raised, warty lesions. Cystic acne may occur.

Lesions affecting the mucous membranes: Mucous membranes are the red, moist linings of all body surfaces except the skin (e.g. mouth, esophagus, rectum, vulva, vagina). Patients with Darier disease may uncommonly have a white cobblestone pattern or small papules affecting the mucous membranes. Overgrowth of the gums is also seen.
Most patients will develop signs of the disease (even if subtle) before the age of 30 years. Many patients will have a mild form of the disease that, although present, will go unnoticed throughout life. Patients with more severe disease will notice a chronic relapsing-remitting pattern to their signs and symptoms although cases of spontaneous resolution of signs have been reported. The rash is often exacerbated by sunlight (a reaction which may be delayed e.g. on return from holiday), and occasionally by steroid use (although this may be useful for other patients). Bacterial infection can cause flares. Widespread infection of the skin with the herpes simplex (cold sore) virus is a well recognized complication. This can cause a severe flare and patients can feel quite unwell. In most patients general health remains good regardless of the severity of the disease.
TREATMENT: Treatment of choice for severe cases is oral retinoid. During flares, topical or oral antibiotics may be administered. Cyclosporine and prescription-only topical corticosteroids, e.g., betamethasone, have been used during acute flares. Some patients are able to prevent flares with use of topical sunscreens and oral vitamin C.
Basic measures for keratosis follicularis (Darier disease) are as follows:
- Sunscreen, cool cotton clothing, and avoidance of hot environments can help prevent flares, especially during the summer.
- Moisturizers with urea or lactic acid can reduce scaling and hyperkeratosis.
- A low- or mid-potency topical steroid is sometimes useful for inflammation.
- When bacterial overgrowth is suspected or crusting is prominent, application of antiseptics such as triclosan or soaks in astringents such as Burrow or Domeboro solution can be helpful.
- Topical medications for keratosis follicularis (Darier disease) are as follows:
SURGICAL CARE:
- Dermabrasion has been used to smooth the hyperkeratosis lesions of keratosis follicularis (Darier disease), with acceptable results.
- Electro surgery and Mohs micrographic surgery have been used to treat localized keratosis follicularis (Darier disease) areas, with good results.
- Amongst newer modalities, laser ablation of recalcitrant plaques has been reported in 7 keratosis follicularis (Darier disease) patients. Of these, 3 patients were treated with carbon dioxide lasers, with Err: YAG lasers and 2 with pulsed-dye lasers. In all of these cases, treatment was successful, with only one patient developing disease recurrence in her axilla 7 months after treatment. Another report describes resolution of disease using 1550-nm erbium-doped fractional fiber laser.
- Carbon dioxide laser ablation with adjunctive dermabrasion, curettage, and shave excision in various combinations has also been reported to cause disease remission for 8 months to 2 years.
- Photodynamic therapy with 5-aminolevulinic acid was used to treat keratosis follicularis (Darier disease) lesions in 6 patients, with 4 patients showing sustained improvement or clearance for a follow-up period of 6 months to 3 years.
CONCLUSION:
Although Darier's disease is a chronic and unremitting burden, most patients manage to lead a relatively normal life.
REFERENCE:
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby.
- Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill.
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders.
- National Organization for Rare Disorders (2002). NORD Guide to Rare Disorders. Lippincott Williams & Wilkins
- Godic A, Miljkovic J, Kansky A, Vidmar G (2005). "Epidemiology of Darier's Disease in Slovenia.". Acta Dermatovenerologica Alpina Panonica ET Adriatica 14 (2): 43–48.
- Munro CS (August 1992). "The phenotype of Darier's disease: penetrance and expressivity in adults and children.” Br J Dermatol. 127 (2): 126–30.
- Tavadia1 S, Mortimer E, Munro CS (January 2002). "Genetic epidemiology of Darier's disease: a population study in the west of Scotland.” Br J Dermatol. 146 (1): 107–9.
- Burg SM, Wilkinson JD. (1992). "Darier-white disease: A review of the clinical features in 163 patients". J Am Acad Dermatol. 27: 40–50.
- Burge S, Monk S, Hovnanian A (September 1999). "Spectrum of novel ATP2A2 mutations in patients with Darier's disease". Hum. Mol. Genet.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









