About Authors:
Dipal Patel*1, Dr. Kamal Singh Rathore1, Twinkal Patel2
Department of Pharmacology
1B.N. Institute of Pharmaceutical Science, Udaipur (Rajasthan), 313001
2Shri Sarvajanik college of Pharmacy, Mehsana (Gujarat).
*dipalpatel786@gmail.com
Abstract:
Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in mood, energy, activity levels and the ability to carry out day-to-day tasks. Symptoms of bipolar disorder are severe. They are different from the normal ups and downs that everyone goes through from time to time. Bipolar disorder symptoms can result in damaged relationships, poor job or school performance, and even suicide. But bipolar disorder can be treated, and people with this illness can lead full and productive lives. Bipolar disorder often develops in a person’s late teens or early adult years. At least half of all cases start before age 25.Some people have their first symptoms during childhood, while others may develop symptoms late in life. Bipolar disorder is not easy to spot when it starts. The symptoms may seem like separate problems, not recognized as parts of a larger problem. Some people suffer for years before they are properly diagnosed and treated. Like diabetes or heart disease, bipolar disorder is a long-term illness that must be carefully managed throughout a person’s life.
REFERENCE ID: PHARMATUTOR-ART-1897
INTRODUCTION:
Bipolar disorder (also known as manic depression) causes serious shifts in mood, energy, thinking, and behavior–from the highs of mania on one extreme, to the lows of depression on the other. More than just a fleeting good or bad mood, the cycles of bipolar disorder last for days, weeks, or months. And unlike ordinary mood swings, the mood changes of bipolar disorder are so intense that they interfere with your ability to function.
During a manic episode, a person might impulsively quit a job, charge up huge amounts on credit cards, or feel rested after sleeping two hours. During a depressive episode, the same person might be too tired to get out of bed and full of self-loathing and hopelessness over being unemployed and in debt.
The causes of bipolar disorder aren’t completely understood, but it often runs in families. The first manic or depressive episode of bipolar disorder usually occurs in the teenage years or early adulthood. The symptoms can be subtle and confusing; so many people with bipolar disorder are overlooked or misdiagnosed–resulting in unnecessary suffering. But with proper treatment and support, you can lead a rich and fulfilling life.
Definition and Etiology
Bipolar affective disorder (BPD), classified as a mood disorder,[1]is a chronic, recurrent illness associated with high rates of morbidity, disability, and premature death from suicide. The disturbance of mood in BPD is episodic and recurrent, cycling at varying intervals from one mood state to another. Current classification schemes are based on the predominant pattern of mood (i.e., depression, mania, hypomania, or mixed states), the intensity of mood, and the rate of cycling from one mood to another (Fig. 1). Disturbed mood in BPD is typically accompanied by reckless and impulsive behavior, psychotic symptoms (e.g., delusions, hallucinations, and disorganized thinking), and cognitive disturbances.
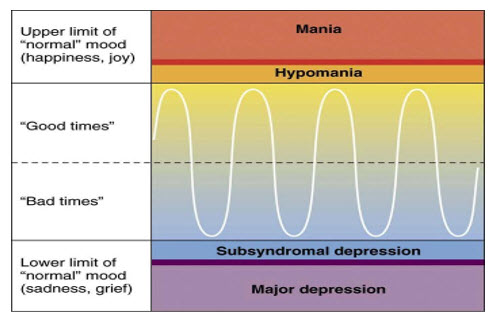
Figure; 1)Rate of cycling from one mood to another
Signs and Symptoms of Bipolar disorder
The symptoms vary widely in their pattern, severity, and frequency. Some people are more prone to either mania or depression, while others alternate equally between the two types of episodes. Some have frequent mood disruptions, while others experience only a few over a lifetime.
Figure; 2) Bipolar Disorder
There are four types of mood episodes in bipolar disorder: mania, hypomania, depression, and mixed episodes.
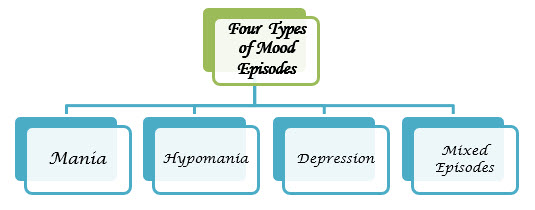
Each type of bipolar disorder mood episode has a unique set of symptoms:
Mania :
Mania is the defining feature of bipolar disorder. Mania is a distinct period of elevated or irritable mood, which can take the form of euphoria, and lasts for at least a week (less if hospitalization is required).[2]People with mania commonly experience an increase in energy and a decreased need for sleep, with many often getting as little as three or four hours of sleep per night. Some can go days without sleeping.[3]A manic person may exhibit pressured speech, with thoughts experienced as racing.[4]Attention span is low, and a person in a manic state may be easily distracted. Judgment may be impaired, and sufferers may go on spending sprees or engage in risky behavior that is not normal for them. They may indulge in substance abuse, particularly alcohol or other depressants, cocaine or other stimulants, or sleeping pills. Their behavior may become aggressive, intolerant, or intrusive. They may feel out of control or unstoppable, or as if they have been "chosen" and are "on a special mission", or have other grandiose or delusional ideas. Sexual drive may increase. At more extreme levels, a person in a manic state can experience psychosis, or a break with reality, where thinking is affected along with mood.[5]This can occasionally lead to violent behaviors.[6]
* Common signs and symptoms of mania include:
- Inflated self-esteem or grandiosity
- Decreased need for sleep (e.g., feels rested after only 3 hours of sleep)
- More talkative than usual or pressure to keep talking
- Flight of ideas or subjective experience that thoughts are racing
- Distractibility (attention too easily drawn to unimportant or irrelevant external stimuli)
- Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation
- Excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g., unrestrained buying sprees, sexual indiscretions, or foolish business investments)
Hypomania :
Hypomania is a mild to moderate level of elevated mood, characterized by optimism, pressure of speech and activity, and decreased need for sleep. Generally, hypomania does not inhibit functioning as mania does.[7]Many people with hypomania are actually more productive than usual, while manic individuals have difficulty completing tasks due to a shortened attention span. Some hypomanic people show increased creativity, although others demonstrate poor judgment and irritability. Many experience hyper sexuality. Hypomanic people generally have increased energy and increased activity levels. They do not, however, have delusions or hallucinations.
Hypomania may feel good to the person who experiences it. Thus, even when family and friends recognize mood swings, the individual often will deny that anything is wrong.[8]What might be called a "hypomanic event", if not accompanied by depressive episodes, is often not deemed as problematic, unless the mood changes are uncontrollable, volatile or mercurial. If left untreated, an episode of hypomania can last anywhere from a few days to several years. Most commonly, symptoms continue for a few weeks to a few months.[9]
* Common signs and symptoms of mania include:
- Feeling unusually “high” and optimistic OR extremely irritable
- Unrealistic, grandiose beliefs about one’s abilities or powers
- Sleeping very little, but feeling extremely energetic
- Talking so rapidly that others can’t keep up
- Racing thoughts; jumping quickly from one idea to the next
- Highly distractible, unable to concentrate
- Impaired judgment and impulsiveness
- Acting recklessly without thinking about the consequences
- Delusions and hallucinations (in severe cases)
Depressive:
Signs and symptoms of the depressive phaseof bipolar disorder include persistent feelings of sadness, anxiety, guilt, anger, isolation, or hopelessness; disturbances in sleep and appetite; fatigue and loss of interest in usually enjoyable activities; problems concentrating; loneliness, self-loathing, apathy or indifference; depersonalization; loss of interest in sexual activity; shyness or social anxiety; irritability, chronic pain (with or without a known cause); lack of motivation; and morbid suicidal thoughts. In severe cases, the individual may become psychotic, a condition also known as severe bipolar depression with psychotic features. These symptoms include delusionsor, less commonly, hallucinations, usually unpleasant. A major depressive episode persists for at least two weeks, and may continue for over six months if left untreated.[10]
* Common symptoms of bipolar depression include:
|
|
Mixed Affective :
In the context of bipolar disorder, a mixed state is a condition during which symptoms of mania and depression occur simultaneously. Typical examples include weeping during a manic episode or racing thoughts during a depressive episode. Individuals may also feel very frustrated in this state, for example thinking grandiose thoughts while at the same time feeling like a failure. Mixed states are often the most dangerous period of mood disorders, during which the risks of substance abuse, panic disorder, suicide attempts, and other complications increase greatly.[11]
* Common symptoms of bipolar depression include:
- depression combined with agitation
- Irritability
- anxiety, insomnia
- distractibility
- racing thoughts
Bipolar Disorder Causes and Triggers
Bipolar disorder has no single cause. It appears that certain people are genetically predisposed to bipolar disorder. Yet not everyone with an inherited vulnerability develops the illness, indicating that genes are not the only cause. Some brain imaging studies show physical changes in the brains of people with bipolar disorder. Other research points to neurotransmitter imbalances, abnormal thyroid function, circadian rhythm disturbances, and high levels of the stress hormone cortisol.
External environmental and psychological factors are also believed to be involved in the development of bipolar disorder. These external factors are called triggers. Triggers can set off new episodes of mania or depression or make existing symptoms worse. However, many bipolar disorder episodes occur without an obvious trigger.
- Stress – Stressful life events can trigger bipolar disorder in someone with a genetic vulnerability. These events tend to involve drastic or sudden changes–either good or bad–such as getting married, going away to college, losing a loved one, getting fired, or moving.
- Substance Abuse – While substance abuse doesn’t cause bipolar disorder, it can bring on an episode and worsen the course of the disease. Drugs such as cocaine, ecstasy, and amphetamines can trigger mania, while alcohol and tranquilizers can trigger depression.
- Medication – Certain medications, most notably antidepressant drugs, can trigger mania. Other drugs that can cause mania include over-the-counter cold medicine, appetite suppressants, caffeine, corticosteroids, and thyroid medication.
- Seasonal Changes – Episodes of mania and depression often follow a seasonal pattern. Manic episodes are more common during the summer and depressive episodes more common during the fall, winter, and spring.
- Sleep Deprivation – Loss of sleep—even as little as skipping a few hours of rest—can trigger an episode of mania.
Bipolar disorder and suicide
The depressive phase of bipolar disorder is often very severe, and suicide is a major risk factor. In fact, people suffering from bipolar disorder are more likely to attempt suicide than those suffering from regular depression. Furthermore, their suicide attempts tend to be more lethal.
The risk of suicide is even higher in people with bipolar disorder who have frequent depressive episodes, mixed episodes, a history of alcohol or drug abuse, a family history of suicide, or an early onset of the disease.
The warning signs of suicide include:
|
|
Basics of bipolar disorder treatment
- Bipolar disorder requires long-term treatment. Since bipolar disorder is a chronic, relapsing illness, it’s important to continue treatment even when you’re feeling better. Most people with bipolar disorder need medication to prevent new episodes and stay symptom-free.
- There is more to treatment than medication. Medication alone is usually not enough to fully control the symptoms of bipolar disorder. The most effective treatment strategy for bipolar disorder involves a combination of medication, therapy, lifestyle changes, and social support.
- It’s best to work with an experienced psychiatrist. Bipolar disorder is a complex condition. Diagnosis can be tricky and treatment is often difficult. For safety reasons, medication should be closely monitored. A psychiatrist who is skilled in bipolar disorder treatment can help you navigate these twists and turns.
Aripiprazole
Carbamazepine ER
Chlorpromazine
Lamotrigine
Lithium
Olanzapine
Olanzapine-fluoxetine combination
Quetiapine
Risperidone
Valproate, Divalproex ER
Ziprasidone
Other treatments
1. Electroconvulsive Therapy (ECT)— for cases in which medication and/or psychotherapy does not work, electroconvulsive therapy (ECT) may be useful. ECT, formerly known as “shock therapy,” once had a bad reputation. But in recent years, it has greatly improved and can provide relief for people with severe bipolar disorder who have not been able to feel better with other treatments.
Before ECT is administered, a patient takes a muscle relaxant and is put under brief anesthesia. He or she does not consciously feel the electrical impulse administered in ECT. On average, ECT treatments last from 30–90 seconds. People who have ECT usually recover after 5–15 minutes and are able to go home the same day.[12]
Sometimes ECT is used for bipolar symptoms when other medical conditions, including pregnancy, make the use of medications too risky. ECT is a highly effective treatment for severely depressive, manic, or mixed episodes, but is generally not a fi rst-line treatment. ECT may cause some short-term side effects, including confusion, disorientation, and memory loss. But these side effects typically clear soon after treatment. People with bipolar disorder should discuss possible benefits and risks of ECT with an experienced doctor.[13]
2. Sleep Medications— People with bipolar disorder who have trouble sleeping usually sleep better after getting treatment for bipolar disorder. However, if sleeplessness does not improve, the doctor may suggest a change in medications. If the problems still continue, the doctor may prescribe sedatives or other sleep medications. People with bipolar disorder should tell their doctor about all prescription drugs, over-the-counter medications, or supplements they are taking. Certain medications and supplements taken together may cause unwanted or dangerous effects.
Self-help for bipolar disorder
While dealing with bipolar disorder isn’t always easy, it doesn’t have to run your life. But in order to successfully manage bipolar disorder, you have to make smart choices. Your lifestyle and daily habits have a significant impact on your moods. Read on for ways to help yourself:
- Get educated. Learn as much as you can about bipolar disorder. The more you know, the better you’ll be at assisting your own recovery.
- Keep stress in check. Avoid high-stress situations, maintain a healthy work-life balance, and try relaxation techniques such as meditation, yoga, or deep breathing.
- Seek support. It’s important to have people you can turn to for help and encouragement. Try joining a support group or talking to a trusted friend.
- Make healthy choices. Healthy sleeping, eating, and exercising habits can help stabilize your moods. Keeping a regular sleep schedule is particularly important.
Monitor your moods. Keep track of your symptoms and watch for signs that your moods are swinging out of control so you can stop the problem before it starts.
Reference:
1) American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text rev. Washington, DC: American Psychiatric Association, 2000.
2) Fattal O, Budur K, Vaughan AJ, Franco K. Review of the literature on major mental disorders in adult patients with mitochondrial diseases. Psychosomatics. 2006, 47: 1-7.
3) Ryan MM, Lockstone HE, Huffaker SJ, et al; “Gene expression analysis of bipolar disorder reveals downregulation of the ubiquitin cycle and alterations in synaptic genes”. Mol Psychiatry. 2006, 11: 965-978.
4) Sun X, Wang JF, Tseng M, Young LT; “Downregulation in components of the mitochondrial electron transport chain in the postmortem frontal cortex of subjects with bipolar disorder”. J Psychiatry Neurosci. 2006, 31: (3): 189-196.
5) Baldessarini RJ, Pompili M, Tondo L; “Suicide in bipolar disorder: Risks and management”. CNS Spectrums. 2006, 11: 465-471.
6) Valtonen HM, Suominen K, Mantere O, et al; “Suicidal behaviour during different phases of bipolar disorder”. J Affect Disord. 2007, 97: 101-107.
7) "Hypomania and Mania Symptoms in Bipolar Disorder". WebMD.com. January 10, 2010.
8) "Bipolar Disorder: NIH Publication No. 95-3679". U.S. National Institutes of Health. September 1995. Archived from the original on 2008-04-29.
9) "Bipolar II Disorder Symptoms and Signs". Web M.D. Retrieved 2010-12-06.
10) Goldman E (1999); "Severe Anxiety, Agitation are Warning Signals of Suicide in Bipolar Patients". Clin Psychiatr News: 25.
11) Srivastava, S.; Ketter, T. A. (2010); "The Link between Bipolar Disorders and Creativity: Evidence from Personality and Temperament Studies". Current Psychiatry Reports 12 (6): 522–530.
12) Pandya M, Pozuelo L, Malone D; “Electroconvulsive therapy: what the internist needs to know”. Cleve Clin J Med. 2007 Sep;74(9):679-685.
13) Mental Health: A Report of the Surgeon General. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health. 1999.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









