 About Authors: N. V. R. Praveen Kumar. T, Mohanta. G. P, Sudarshan. S# and Parimalakrishnan. S.
About Authors: N. V. R. Praveen Kumar. T, Mohanta. G. P, Sudarshan. S# and Parimalakrishnan. S.
Department of Pharmacy, Annamalai University,
Annamalai Nagar – 608002.Tamil Nadu, India.
# Department of Medicine, Rajah Muhtiah Medical College and Hospital, Annamalai University,
Annamalai Nagar – 608002.Tamil Nadu, India.
Reference ID: PHARMATUTOR-ART-1079
Abstract
Objective
The study was conducted to identify and evaluate the Prescription Monitoring of Antihypertensive Drug Utilization for Uncomplicated Hypertension Patients.
Methodology
This was a prospective observational study and was approved by IRB. The study was conducted in tertiary care teaching hospital, which is located at southern part of India having 1210 beds. Totally 1262 prescriptions were studied.
Results
Total distribution of patients with respect to age group showed that highest number of patients was found in the age group of 60-69 years (31.3%) and least was found between 20-29 years age group (1.1%). Majority of males in the study population (43.29%) were found to have both the habits of smoking and alcohol. Among concomitant diseases that were related to hypertension Coronary artery disease was highest (67.78%) and giddiness was least (1.7%). In case of diseases unrelated to hypertension Type II diabetes mellitus was observed as highest (38.7%) and acute gastroenteritis was recorded least (5.68%). Overall 43.5% patients were treated with single antihypertensive drug and 53.8% were treated with antihypertensive drug combinations.
Introdution
Hypertension or high blood pressure is a condition in which the blood pressure in the arteries is chronically elevated. With every heart beat, the heart pumps blood through the arteries to the rest of the body. Blood pressure is the force of blood that is pushing up against the walls of the blood vessels. If the pressure is too high, the heart has to work harder to pump, and this could lead to organ damage and several illnesses such as heart attack, stroke, heart failure, aneurysm, or renal failure. According to Medilexicon's medical dictionary, hypertension means "High blood pressure; transitory or sustained elevation of systemic arterial blood pressure to a level likely to induce cardiovascular damage or other adverse consequences [1]."
Cardiovascular diseases have emerged as an important health problem in India. High blood pressure (BP) is a major risk factor and better control can lead to prevention of 300,000 of the 1.5 million annual deaths from cardiovascular diseases in India. Epidemiological studies demonstrate that prevalence of hypertension is increasing rapidly among Indian urban populations and using the current definitions more than two-fifths of the Indian urban adult population has hypertension [2].
The normal level for blood pressure is below 120/80, where 120 represents the systolic measurement (peak pressure in the arteries) and 80 represents the diastolic measurement (minimum pressure in the arteries). Blood pressure between 120/80 and 139/89 is called prehypertension and a blood pressure of 140/90 or above is considered hypertension. Hypertension may be classified as essential or secondary. Essential hypertension is the term for high blood pressure with unknown cause. It accounts for about 95% of cases. Secondary hypertension is the term for high blood pressure with a known direct cause, such as kidney disease, tumors, or birth control pills [3,4].
Reviews of studies on hypertension epidemiology in India have shown high prevalence in both urban and rural areas [5]. In population-based studies, Joseph et al. reported it in 31% men and 41% women in Thiruvananthapuram, [6] while Mohan et al. reported a crude prevalence rate of 21% in Chennai [7].
High blood pressure may be treated medically, by changing lifestyle factors, or a combination of the two. Important lifestyle changes include losing weight, quitting smoking, eating a healthful diet, reducing sodium intake, exercising regularly, and limiting alcohol consumption. Medical options to treat hypertension include several classes of drugs. ACE inhibitors, ARB drugs, beta-blockers, diuretics, calcium channel blockers, α-blockers, and peripheral vasodilators are the primary drugs used in treatment [8]. These medications may be used alone or in combination, and some are only used in combination. In addition, some of these drugs are preferred to others depending on the characteristics of the patient (diabetic, pregnant, etc.).
The guidelines differ with regard to which drug class is to be considered as first choice for the initial treatment of hypertension with no complications [9]. Thiazide diuretics have been recommended by the seventh report of the joint National Committee [10] and the British Hypertension society as the preferred first-line antihypertensive due to its affordability [11] and evidence on its efficacy in the prevention of cardiovascular events in those with hypertension [12]. The objectives of this study are to monitor prescription pattern of antihypertensive medications of uncomplicated hypertension and to identify the determinants of the choice of first-line drug therapy was undertaken in the inpatient department. Physicians’ compliance with the existing guidelines is described.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Job Alerts by Email
Methodology
Study Design
This is a prospective cross-sectional study done between November 2009 and May 2010, in tertiary medical teaching hospital situated in the South India. The Institutional Human Ethical Committee of Annamalai University, Chidambaram approved the study.
Patient Enrollment
Patients were enrolled for the study after explanation about the study with pictorials and pamphlets and they were not compelled to participate. Patients with hypertension of either sex, above 18 years of age, with or without co morbidities who met the inclusion criteria were included in the study. Oral informed consent was obtained from all patients. The following exclusion criteria applied: age below 16 years, acute medical condition making the screening procedure unacceptable on ethical grounds, dementia or other cognitive or sensory deficits that would make it unlikely that the self-reported measures could be completed or would provide meaningful information. Physicians were asked neither to change their routine-practice behaviors nor to selectively invite patients for participation.
Patient Data Collection Form
The demographic and clinical data was collected from each patient enrolled for the study. The data collection proforma includes the following information such as age, gender, documented blood pressure at the time of first clinic attendance or admission, blood pressure at subsequent visits, and the anti-hypertensive medications were recorded.
Blood Pressure Measurement
Blood pressure was measured at the end of the interview using a mercury sphygmomanometer on the right arm, at the level of the heart of the patient, who was in a sitting position and at rest for at least 10 min. After a 10-min interval, the blood pressure was measured once again, and the average of two measurements was recorded.
Therapeutic Management
Medicines that are prescribed to patients were recorded. Active substances were classified as ACEIs, angiotensin-receptor blockers (ARBs), BBs, Ds, CCBs and other antihypertensives. In addition, fixed dose combinations were also determined separately. The single active medicine treatment is called as monotherapy or a fixed-dose combination of two various diuretics. Polypharmacy with two or more medicine combinations were categorized into two subcategories: free combination, when two active agents are used as separate pharmaceutical preparations, or fixed-dose combination, when a fixed-dose preparation of two agents from different antihypertensive classes is used.
Statistical Analysis
Continuous variables are presented as mean values ± standard deviation (SD), and categorical variables are presented as percentages. Continuous variables were compared with the Student t-test; categorical variables were compared with the chi-square test. Statistical analyses were performed with SPSS software ver. 11.0 (SPSS, Chicago, Ill.). Statistical significance was defined as P < 0.05.
Results
Prescription Frequencies by Age and Gender
A total of 1262 patients were monitored during the entire study period, of which 63% were males and 37% were females. Total distribution of patients with respect to age group showed that highest number of patients was found between the age group of 60-69 years 395 (31.7% of males and 30.5%of females) followed by 347 (28.6% of males and 25.6% of females) between the age group of 50-59 years and least number of patients were found between 20-29 age group with 14(1.3% of males and 1.05% of females). Majority of males in the study population were found to have both habits of smoking and alcohol 342(42.00% of males) followed by habit of only alcohol consumption 169(20.29% of males and 1.06% of females), only smoking 149(16.86% of males and 1.36%). Only 2.68% of males and 15.77% of females were found to be non smokers and non alcoholics. The data are represented in the Table No. 1.
Table No. 1: Demographic data based on sex, distribution of study population with respect to age group and social habits
|
Characteristics |
Males |
Females |
P |
|
N |
63.98% |
36.02% |
|
|
20-29 years |
1.30 |
1.05 |
NS |
|
30-39 years |
12.17 |
14.91 |
< 0.05 |
|
40-49 years |
18.76 |
18.08 |
NS |
|
50-59 years |
28.62 |
25.60 |
< 0.05 |
|
60-69 years |
31.79 |
30.59 |
< 0.01 |
|
70-79 years |
29.43 |
28.57 |
< 0.05 |
|
80 years and more |
23.06 |
19.69 |
< 0.05 |
|
Smokers& Alcohol consumers |
41.98 |
None |
< 0.0001 |
|
Alcohol consumers only |
20.29 |
01.06 |
< 0.001 |
|
Smokers only |
16.86 |
01.36 |
< 0.001 |
|
None Smokers & Alcohol Consumers |
02.68 |
15.77 |
< 0.005 |
Prescription Frequencies by Reason for Admission and Co-Morbidities
It was found that majority of the study population were admitted to the hospital with chief complaints of chest pain 318(36.25%), followed by Breathlessness 202(23.03%), and cough with breathlessness 115(13.11%). The other reasons for admission were vertigo, epistaxis, and weakness. These reasons were related to hypertension and as cardiac disease is major risk factor for hypertension more patients were admitted with complaint of chest pain.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Job Alerts by Email
Among the reasons unrelated to hypertension diabetes mellitus was found highest with 43.75% followed by cough with expectoration 111(28.83%), abdominal pain 48(12.46%) and others 15.06%. In the concomitant diseases that were related to hypertension it was found that coronary artery disease was highest 568(67.78%) followed by CVA 173(20.64%) and least was found to be giddiness with 1.7%. Coming to diseases unrelated to hypertension Type II diabetes mellitus was highest 125 (38.7%) followed by COPD 48 (14.9%), BA 44 (13.62%) and least was to be both acute gastroenteritis and lower respiratory tract infections with 24 (7.43%). Systemic hypertension cases were found to be 101. Overall, 549 (69% of males and 31% of females) patients were treated with a Single antihypertensive drug and 679 (46% of males and 32% of females) were treated with antihypertensive drug combinations. The data are represented in the Table No. 2.
Table No. 2: Related and unrelated reasons for admission, concomitant and unconcomitant diseases related to hypertension
|
Parameters |
% Distribution |
|
|
Male |
Female |
|
|
Related |
|
|
|
Chest Pain Breathlessness Weakness Chest pain and Breathlessness Giddiness Epistaxis |
21.19 16.58 11.74 10.22 7.48 1.34 |
15.06 6.45 4.79 2.89 1.87 0.39 |
|
Unrelated |
|
|
|
Type II DM Cough with expectoration Abdominal pain Others |
28.37 17.40 8.60 12.20 |
15.28 6.43 3.86 2.86 |
|
Concomitant |
|
|
|
Hypertension CAD CVA Pulmonary edema Cardiomyopathy Giddiness Epistaxis |
2.70 50.16 13.83 1.00 1.43 0.95 1.10 |
0.76 17.62 6.81 0.78 1.43 0.75 0.68 |
|
Un-concomitant |
|
|
|
Type IIDM COPD BA Liver chirosis LRTI Age Others |
22.83 10.43 11.85 9.88 4.43 3.92 3.10 |
15.87 4.47 1.77 2.19 3.00 3.51 2.78 |
Monotherapies and Combinations for New Cases of Uncomplicated Hypertension
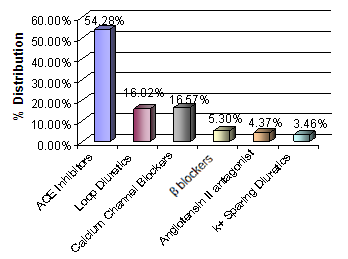
The study revealed that in monotherapy category six classes of drugs were used. These were ACE Inhibitors 298(54.28%), loop diuretics 88(16.02%), calcium channel blockers 91(16.57%), β- Blockers 29(5.3%), followed by Angiotensin II antagonists 24(4.37%) and K? Sparing Diuretics. Among monotherapy, ACE Inhibitors were prescribed most because these are effective and cheaper and K? Sparing diuretics are least used as these were costlier. The data are represented in Fig No. 1.
Fig. No. 1: Distribution of Patients based on single drug therapy
Two Drug Combination Therapy for New Cases of Uncomplicated Hypertension
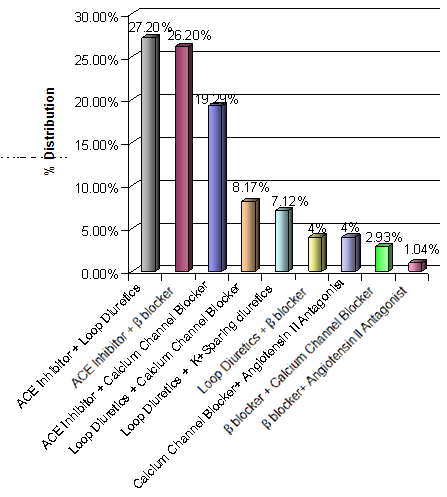
Among those who were treated with drug combinations, 70.25% received two drugs, and a two drug combination of ACE Inhibitors and Loop diuretics were given to majority of patients with 27.25% followed by ACE inhibitors and β-blockers with 26.2% and the drug combination β- blocker and Ag II Antagonist was least prescribed with 1.04%. The data are given in Fig No. 2.
Fig. No. 2: Distribution of Patients based on two drug combination Therapy
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Job Alerts by Email
Three and Four Drug Combination Therapy for New Cases of Uncomplicated Hypertension
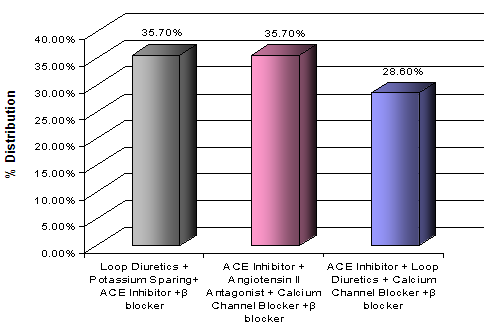
In three drug combination therapy combination of ACE Inhibitors, β-blockers and loop diuretics were prescribed major with 25.54% and least prescribed were combination of Ag II Antagonist, β-blocker and ACE Inhibitor with 2.7%. In combination therapy 27.68% received three drugs, usage of four drugs is uncommon and only 2.06% patients were prescribed four drug combinations. The data are represented as graph and given in Fig No. 3 and 4.
Fig. No. 3: Distribution of Patients based on three drug combination
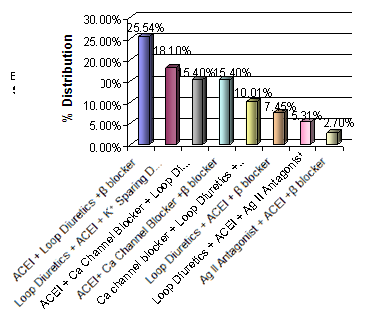
Fig. No. 4: Distribution of Patients based onfour drug combinations
Discussion
The best way to measure and analysis the prescribing pattern of physicians and dispensing of practice of pharmacists is by prescription based study [13]. However, the recommendations of JNC or the WHO/ISH guidelines on hypertension will enrich prescribing pattern. The first line therapy in essential hypertension is with thiazide diuretics medicines at low dosages, which is recommended by JNC in 2003 [10] and NICE 2004, guidelines for antihypertensive therapy published on clinical evidence based [14]. The present study revealed that hypertension was more predominant in males than in females. Single drug and combination therapies were both more used in females 45% and males61%.
In addition, combination therapy looks like more rational to ease the cardiovascular mortality [15]. The results of the present study revealed that mono-drug therapy with ACEIs is prescribed very often, due to cost of the drug, patient’s compliance, adherence and less incidence of adverse events. In the present utilization of diuretics was 19.48%as single drug therapy and overall utilization 56%. Lesser use of diuretics in the present study may be due to adverse effect of diuretics on glucose homeostasis and lipid profile [16]. Renin angiotensin system was activated notably in hypertension patients more efficiently when they are treated with ACEIs [17].
Our study showed that overall drug utilization of ACEIs was 54.28%, as single drug treatment, which was lesser in number as compared to other drugs such as calcium channel blockers 16.5% and β-blockers (5.3%). The data are given in Table No. 3.The previous studies have shown that prescribing thiazides are more economical than treating with other expensive drugs [18,19]. In the present study we can observe a mixed result of the choice of prescribers, patients’ tolerability and effect of antihypertensive medication is because of non availability of guidelines or regulations for prescriber on prescribing pattern.
In our study prescription with diuretics as single drug therapy was found to be 43.5%. In controlling the blood pressure two or more antihypertensive drugs are being used, which were explained in various randomized studies [20,21]. In various international guidelines combination therapies are recommended as the first line treatment for acute hypertension patients [22,23].
TasneemSandozi and Vamsi Krishna Emaniexplained that the hypertension is better controlled by combination therapy but our study revealed that the single drug treatment was found to be widely used and effective [25]. In the present study combination therapy with 2 drugs was frequently used followed by 3 and 4 drugs. Compared to earlier studies of Tiwari H et al who reported the most common drug combination of beta blockers and CCBs the present study shows the combination of ACEIs and diuretics as the most common [26].
Conclusion
In conclusion, our results show that the choices of antihypertensive drugs reasonably comply with the national and international guidelines on the management of hypertension. The benefit of combination therapy over monotherapy as well as possible better efficacy of angiotensin converting enzyme inhibitors over calcium channel blockers in the study population was demonstrated. Under utilization of diuretics and inadequate oral instructions by pharmacists are found to be the limitations of the present prescribing pattern and hence, an intervention study is needed to improve the current prescribing practice in hypertension management.
The study revealed that in monotherapy category six classes of drugs were used that includes ACE Inhibitors, loop diuretics, calcium channel blockers, β- Blockers, followed by Angiotensin II antagonists and K? sparing Diuretics. ACE Inhibitors were prescribed most whereas K? sparing diuretics were least used. From the results of this study, we concluded that there is a considerable scope of improvement for the use of diuretics.
References
1. https://www.medilexicon.com/ accessed on 12 July 2010.
2. Rajeev G and Gupta VP. Hypertension epidemiology in India: Lessons from Jaipur heart watch. Curr Sci. 2009; 97(3):349 – 355.
3. Alexander M, Tekawa I, Hunkeler E et al. Evaluating hypertension control in a managed care setting. Arch Intern Med. 1999; 159:2673–2677.
4. Stockwell D, Madhavan S, Cohen H, Gibson G and Alderman M. The determinants of hypertension awareness, treatment, and control in an insured population. Am J Public Health. 1994; 84:1768–1774.
5. Gupta R. Trends in hypertension epidemiology in India. J. Hum. Hypertens. 2004; 18:73–78.
6. Joseph A, Kutty VR and Soman CR. High risk for coronary heart disease in Thiruvanthapuram City: a study of serum lipids and other risk factors. Indian Heart J. 2000; 52:29–35.
7. Mohan V, Gukulkrishnan K, Unnikrishnan R and Deepa R. Epidemiology of hypertension in India: Lessons from the Chennai urban population study. In type 2 diabetes in South Asians. In: Mohan V and Rao GHR, eds. Epidemiology risk factors and prevention. New Delhi, Jaypee Brothers; 2007: 317–330.
8. Adnan A, Omer K, Aytekin O, et al. Prescribing pattern of antihypertensive drugs in primary care units in Turkey: Results from the TURKSAHA study. Eur J ClinPharmacol. 2007; 63:397–402.
9. Messerli HF, Grossman E and Goldbourt U. Are beta-blockers are efficacious as first line therapy for hypertension in the elderly? : A Systemic review. JAMA. 1998; 279:1903 – 1907.
10. Chobanian AV, Bakris GL, Black HR, et al. 7th report of the JNC on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003; 289:2560 – 2572.
11. Lawrence ER, Bryan W, Dennis JG, et al. British hypertension society guidelines for hypertension management 1999: Summary. BMJ. 1999; 319:630 – 635.
12. Amery A, Birkenhager W, Brixko P, et al. Mortality and morbidity results from the European working party on high blood pressure in the elderly trial. Lancet. 1985; 1:1349–1354.
13. Tiwari H, Kumar A and Kulkarni SK. Prescription monitoring of antihypertensive drug utilisation at the Punjab University Health Centre in India. Singapore Med J. 2004; 45(3):117 – 120.
14. NIH and Clinical Excellence: Essential hypertension: managing adult patients in primary care. https://www.nice.org.uk/nicemedia/pdf/CG18background.pdf. Accessed on December 20, 2009.
15. Mancia G and Grassi G. Antihypertensive treatment: past, present and future. J Hypertens. 1998; 16:1 – 7.
16. Prisant LM, Beall SP, Nicholads GE, et al. Biochemical, endocrine, and mineral effects of indapamide in black women. J Clin Pharmacol. 1990; 30:121 – 126.
17. Hansson L. The place of beta-blockers in the treatment of hypertension in 1993. Clin Exp Hypertens. 1993; 15:1257-1262.
18. Fretheim A, Aaserud M, Oxman AD. The potential savings of using thiazides as the first choice antihypertensive drug: cost-minimization analysis. BMC Health Serv Res. 2003; 3:18.
19. Xu KT, Moloney M and Phillips S. Economics of suboptimal drug use: cost-savings of using JNC-recommended medications for management of uncomplicated essential hypertension. Am J Manag Care. 2003; 9:529-536.
20. Hansson L, Zanchetti A, Carruthers S, et al. Effects of intensive blood-pressure lowering and low dose aspirin in patients with hypertension: Principal results of the Hypertension optimal Treatment (HOT) randomized trial. Lancet. 1988; 351:1755–1762.
21. Cushman WC, Ford CE, Cutler JA et al. ALLHAT Collaborative Research Group – Success and predictors of blood pressure control in diverse North American settings: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) J Clin Hypertens. 2002; 4:393–405.
22. Chobanian AV, Bakris GL, Black HR, et al. 7th report of the JNC on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003; 289:2560 – 2572.
23. Guidelines Committee ESH-ESC. European Society on Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003; 21:1011 – 1053.
24. Tasneem Sandozi and Vamsi KE. Survey of prescription pattern of anti-hypertensive drugs in hypertensives& hypertension associated diabetics. Int J Pharma and Bio Sci. 2010; 1(4):23 – 26.
25. Tiwari H, Kumar A and Kulkarni SK. Prescription monitoring of antihypertensive drug utilisation at the Punjab University Health Centre in India. Singapore Med J. 2004; 45(3):117 – 120.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org









