{ DOWNLOAD AS PDF }
ABOUT AUTHORS
Muthyala Nagavamsidhar*1, Qadrie ZL.2, Suman A.1
*1 Department of Pharmacy Practice,
Pratishta Institute of Pharmaceutical Sciences,
Suryapet, Hyderabad, Telangana, India
nagavamsi.muthyala@gmail.com
ABSTRACT: Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. The WHO has rated migraine amongst the top 20 most disabling life time conditions. Migraine is a pervasive and debilitating, chronic neurological painful disorder, affecting from 15% to 29% of the general population. It is the second most common cause of headache characterized by recurrent episodes of headache and associated symptoms i.e. nausea, sensitivity to light and noise that typically last from 4 to 72 hours which is divided into four phases. Migraine is well explained with three hypothesis i.e., vascular, platelet, central nervous system. It affects people of all groups, sexes, races and social classes around the globe. Migraine can occur due to various trigger factors and can be managed with both pharmacological and non-pharmacological treatment.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-2580
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 6, Issue 4 Received On: 05/02/2018; Accepted On: 12/02/2018; Published On: 01/04/2018 How to cite this article: Muthyala N, Qadrie ZL, Suman A; Migraine & Migraine Management: A Review; PharmaTutor; 2018; 6(4); 8-17; http://dx.doi.org/10.29161/PT.v6.i4.2018.8 |
INTRODUCTION
Migraine is a pervasive and debilitating, chronic neurological painful disorder, affecting from 15% to 29% of the general population (10% of adult population in United States) (Alvin et. al. 1979). Migraine is the second most common cause of headache characterized by recurrent episodes of headache and associated symptoms i.e., nausea, sensitivity to light and noise that typically last from 4 to 72 hours. Pain management of migraine includes both non-pharmacological and pharmacologic methods for acute episodes and prophylaxis. Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage (Terry J. Baumann,2005). Pain is a dynamic complex process which is generally classified in terms of nociceptive and neuropathic pathways, migraine pain is a neuropathic pathways which is quiet different from nociceptive pain which is sustained by abnormal processing of sensory input by peripheral or CNS, a large number neuropathic pain syndromes exist and clinically ,they are often difficult to treat (pasero et al ,1999) patients presents with spontaneous pain transmissions often described as tingling, burning, shockline or shooting, exaggerated painful response to normally non-noxious stimuli (Allodynia) (pasero et al 1999,Elliott,1994)or painful repoint to noxious stimuli (hyperalgesia).
On an average a migraineur experiences around 13 attacks per year which may vary from person to person. The WHO has rated migraine amongst the top 20 most disabling life time conditions. It affects people of all groups, sexes, races and social classes around the globe. Migraine can occur due to various trigger factors like stress, emotions, environmental factors, genetic factors, diet, sleep disturbances hormonal factors (menstruation, oral contraceptives) (migraine.org.uk/triggers).
PATHOPHYSIOLOGY:
According to vascular hypothesis proposed by Harold Wolff in 1938, the migraine aura is caused by intracerebral arterial vasoconstrictions that is followed by reactive extra-cranial vasodilatation and associated headache. Migraine without aura is a neurobiological disorder (J Olesen et al,2004) and pain is believed to result from activity within trigeminal nucleus results in release of vasoactive neuropeptides, particularly calcitonin gene-related peptide (CGRP), Neurokinin A, and substance P, from perivascular axons. The released neuropeptides interact with dural blood vessels to promote vasodilatation and dural plasma extravasations, resulting in perivascular inflammation. Orthodromic conduction alone trigeminovascular fibres transmits pain impulses to the trigeminal nucleus caudalis where the information is relayed further to higher cortical pain centres (www.hartp.neurology.ucla.edu).
Migraine genes identified by studying families with familial hemiplegic migraine (FHM) which involves gene mutations CACNA1A of calcium voltage gated (50%) and SCN1A of Na+/K+ ATPase (20%). Data also support a role for dopamine in pathophysiology of certain sub types of migraine which induces stimulation so dopaminergic antagonists show effective therapeutic agents against migraine. Pharmacological data supports the serotonin (5-HT) as antimigraine therapy (Peter J Goadsby et al,2005). Coming to platelet hypothesis, which involves abnormal platelet activation with relevant characteristics like:
a. They do not adhere to one another unless precipitated;
b. Certain stimuli (catecholamines, thromboxane A2 and ADP.
c. Once aggregates form; they release a portion of contents (eg. Serotonin, adenosine and its phosphate derivatives).
Prostaglandin produced by platelets (thromboxane A2) and vascular endothelium (prostacyclin) produces vasoconstriction and vasodilatation (Deshmukh 1977, Meyer). This platelet hyperaggregability forms micro-emboli that lodge in microvasculature release their contents cause changes in vasomotor tone which induce tissue response leading to migraine pain. Platelets which is a primary blood source of serotonin where a rapid decline in plasma levels occur in initiation and during migraine attack which is indicated with increase in metabolite of serotonin, urinary 5-hydroxyindoleacetic acid which indicate serotonin release during migraine attackswhere as this does not occur in other headache types and not a reaction to pain, stress and vomiting (Rydzewski 1978, Saito et al 1987). Serotonin enhance sensitivity to pain receptors leading to vacular permeability where pain producing substance release at site leading to inflammatory response in migraine attacks (Glover et al, 1982), according to central nervous system hypothesis it is a disturbance with secondary vasomotor changes in CNS, it is initiation of neurologic symptoms occurs primarily in cerebral cortex and progressed gradually with cerebral depression (Olesen ,1985). Migraine attacks can be precipitated centrally with psychological stress, fatigue excitation of neural pathways by environmental stimuli (i.e., Noise, Glare).
From above discussion it is evident that no complete satisfying description of pathologic events associated with migraine exists. Migraine is general classified by International Headache Society shown below in flowchart (Olesen et al, 2004, ihs.org).
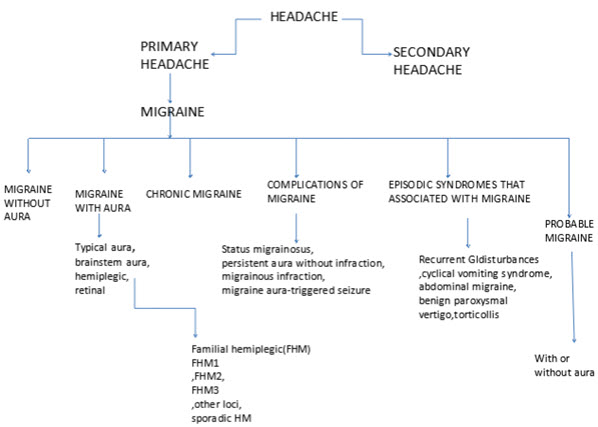
Flow-chart 1: Based on IHS Classifications, Types of Migraine
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
TRIGGER ZONES AND FACTORS:
Migraine occurs at five trigger zones:
Medials border of the supraciliar arch, close to the insertion. Medial part of the proximal/anterior fibres of temporal muscle, close to its insertion surrounding the saggital suture. Sub occipital area at the level of insertion of thick muscles of neck. Occipital area surrounding the emergence of the Arnold’s nerve, medial area of the superior trapezius in the neck. With the above number of trigger points and location of these points along with the accompanied characteristics features of unilateral location, photophobia and phonophobia (Calandre et al, 2006).
Migraine occurs with many triggers like:
a. Stress (relief of stress)
b. Lack of Food or Infrequent Meals (missing meals)
c. Certain Foods (including of products like caffeine, tyramine, alcohol, monosodium glutamate)
d. Changing Sleep Patterns (weekend lie-ins or shift work)
e. Hormonal Factors (menstrual cycles, oral contraceptives)
f. Over tiredness /Over-exertion (both physical or mental)
g. Extreme Emotions (anger and grief)
h. Environmental Factors (loud noise, bright lights, strong smells, hot stuffy atmosphere)
i. Climatic conditions (strong winds, extreme cold or hot)
j. Obesity is a risk for migraine(progress from episodic to chronic migraine) (Scher et al 2003)
Stages of Migraine Attack:
In human beings, migraine is different, which includes five stages that distinguish migraine from another headache.
Premonitory or warning phase:
It is also known as prodrome phase were certain physical and mental changes such as tiredness, mood changes, feeling thirsty and a stiff neck. This symptom lasts about 1 to 24 hrs.
Aura phase:
This stage includes a wide range of neurological symptoms lasting for 5 to 60 minutes, where migraine without aura does not include. Symptoms include dark or colored spots, numbness, vertigo, speech and hearing disturbance, confusion, partial paralysis. Around 20% children and young people experience “aura”.
Main attack:
In this phase, you will have cephalgia or abdominal pain, nausea, vomiting decrease in concentration and sensitive to light or sound.
Resolution /Postdrome stage:
This phase is the final stage of attack; symptoms mimic first stage and lasting about hours or days to disappear the feeling of hangover or tiredness (migrainetrust.org).
Diagnosis of Migraine:
Migraine can be diagnosed on the basis of frequency and number of attacks and associated with typical warning signs and symptoms. It is typically manifest by episodic headache though it is more than just head pain
Differential Diagnosis:
Migraine is typically diagnosed from Tension Type Headache (TTH) as it lasts about hours or days as TTH is chronic present more often. Migraine varies from cluster headache with unilateral headache with autonomic dysfunction and other type is medication overuse headache (MOH) which is transformed into chronic daily headache similar to that of chronic TTH with some migrainous features.
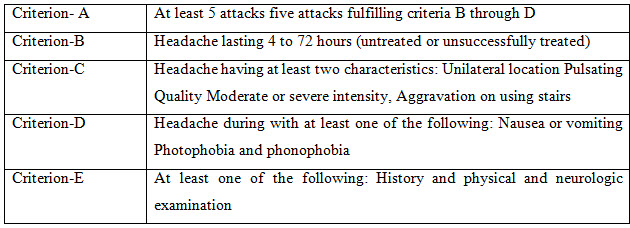
According to International Headache Society Criteria, migraine is of two types: Migraine with Aura (Table No.: 1) and Migraine without Aura (Table No.: 2). Note that trigger factors, family history, treatment response have no additional diagnostic value.
Migraine without Aura (MO) is often known as common migraine characterized with episodic diabling headache lasting about few hours to few days accompanied with gastrointestinal symptoms or by heightened special senses it displays the criteria of IHS with generalized or mild pain and does not have to be severe or unilateral. This is common within patients referred with “intractable migraine” or “status migrainosus”.
Migraine with Aura (MA) is often called as focal or classical migraine. Aura affecting movement, sensation, cognition, vestibular function or consciousness may difficult to distinguish with thromboembolism or epilepsy patient presenting recent onset of MA gives longer history of MO mistakenly diagnosed as “bilious attacks”,” sinusitis” or normal headache.MA often without headache triggers fearing transient ischemic attacks(TIA).
Table No. 1: Diagnostic Criteria for Migraine with Aura (i-h-s.org /2004)
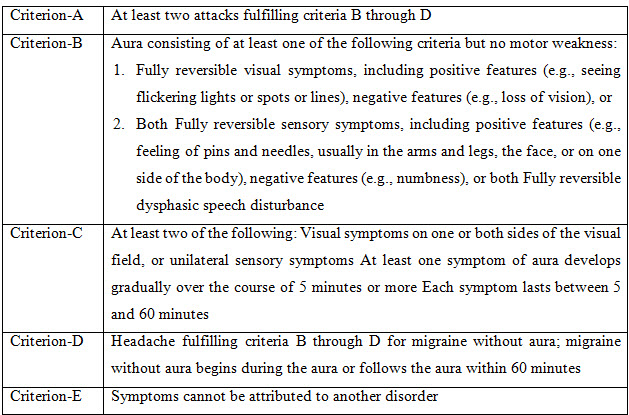
Table No. 2: diagnostic criteria for Migraine without aura (www.i-h-s.org /2004)
Examination and Investigations:
The main goal of examination and investigation is to consider brain disease and to screen out hypertension and depression along with exclusion of causes of migraine like symptoms but no tests to confirm migraine. Investigations include brain scan which is referral to find the early diagnosing of neurological disorders which provides impossible workload of 18% women, 6% men have migraine, 3% have chronic daily headache.
Other tests include erythrocyte sedimentation rate (ESR) in early headache of geriatrics which address temporal arteritis and chest X-ray in smokers to consider metastatic cancer.
Pain Management of Migraine:
Pain is generally cured both non-pharmacologically and pharmacologically with the help to treat acute episodes and prophylaxis. Pharmacological treatment of migraine affects primarily to alleviate head pain, avoiding headache recurrence and immense use of rescue medications (Landy 2004, Stewart et al 1992).
Non-pharmacologic treatment of migraine includes cognitive behavior therapy.
Cognitive Behavioral Therapy (CBT): It is based on principle that anxiety and distress are aggravators of an evolving migraine headache.it is designed to help patient identify and modify maladaptive response that may trigger or aggrevate a migraine headache (Selby,1960). Stress management training is often part of treatment. CBT is usually combined with other behavioural therapies but it is more effective as its own (Bakal et al. 1981, Richardson 1989).These technique are combined with biofeedback therapy (a technique where people learn to sense changes in the body activity and to use relaxation and other methods to control body responses (hartp.neurology.ucla.edu), although uncontrolled studies have shown their efficacy in reducing efficacy, duration and frequency of headache when used alone (Sorbi 1984, Warner 1975).
Complementary Treatments: These includes acupuncture or acupressure (19%), massage (42%), exercise (30%) and chiropractice (15%), herbs (15%) etc. In acupressure with the help of fine metal needles or mechanical pressure the acupuncturist manipulates energy called Chi or Qi. In massage, relaxation of the body releases stress buildup in muscle tissue and teaches body awareness (hartp.neurology.ucla.edu).
Yoga therapy: Yoga, coupling physical exercise and breathing, meditation are the alternative form of mind body therapy and used to lower the symptoms of chronic pain, emotional stress, anxiety and depression (Kim et al. 2005, Kakigi et al., 2005). It has potential effect as therapeutic intervention in various chronic disease conditions. Yogic breathing is a unique method for balancing the autonomic nervous system and influencing psychologic and stress-related disorders (Mel, 2002). These practice of yoga is carried in prodromal stage and not in resolution and postdromal stage (John et al 2007).
Other Supplement Treatments:
Some of the vitamins as well as mineral supplements are responsible in treatment of migraine which is observed in scientific studies that potentiates the treatment.
Riboflavin: It is vitamin B2, which is important for energy metabolism. The rationale for using riboflavin is that it helps in boost brain metabolism. It is taken about 400 mg per day.
Melatonin: It is used as homeopathic sleep aid and to help with jet lag, but no significant studies in treating migraine or other headache, useful in treating sleep disturbances. It is taken 3-6 mg at bedtime.
Magnesium: Magnesium has wide function in our body, fluctuations in levels of magnesium results in triggers of migraine. It is given about 300-500 mg per day.
Co-Enzyme Q10: It is very essential constituent of cells that involves metabolism. In migraine triggers it is used to increase Q10 levels that increase brain metabolism. It is given about 300-600 mg per day (hartp.neurology.ucla.edu).
Feverfew: 1 CAPSULE 3-4 times per day for 1 month if effective the dosage may slowly have reduced. Avoid during pregnancy and with NSAIDS (hartp.neurology.ucla.edu).
Lifestyle Modifications: Lifestyle impacts the severity and frequency of migraine can be understand and useful for successful prevention of migraine.
Sleep: Maintain consistent sleep patterns, including weekend and holidays
Exercise: A routine of 20-40 minutes of aerobic exercise can relieve stress and maintain balance internal physiology.
Eating: Maintain regular meals and take good diet.
Reduce stress and increase posture: Reduce stress with yoga, meditation and maintain posture that imparts migraine triggers
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Pharmacological Treatment:
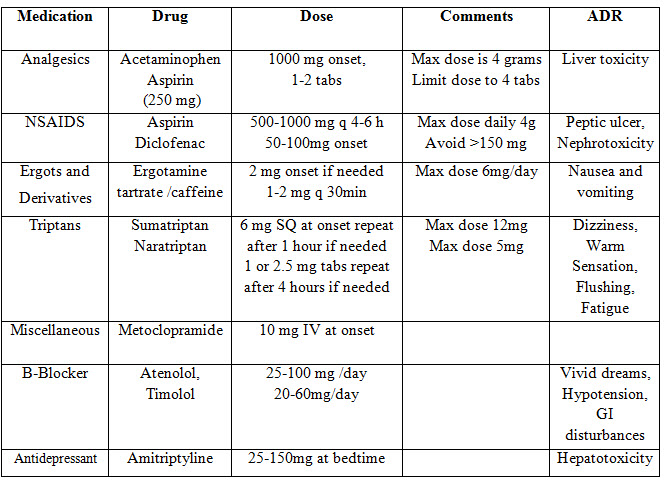
Pharmacologic treatment of migraine includes simple analgesics and NSAIDs for acute to moderate migraine attacks (Silberstein 1999, Stewart 2000, Lipton et al 2001). NSAIDs appear to prevent neurologically mediated inflammation in trigeminovascular system through inhibition of prostaglandin synthesis (Dalessio, 1994). Combination therapy with prokinetics such as Metoclopramide and Domperidone increases the absorption of NSAIDs and analgesics and alleviate migraine related nausea and vomiting (Bartleson 1994). Over the counter combinations of acetaminophen, caffeine and aspirin was approved for treating migraine in US due to its efficacy in relieving migraine pain and its associated symptom more than simple analgesics (Fettes 1999, Weitzel, 1999) see in Table No. 3 below.
Table No. 3: (Peter, 2010)
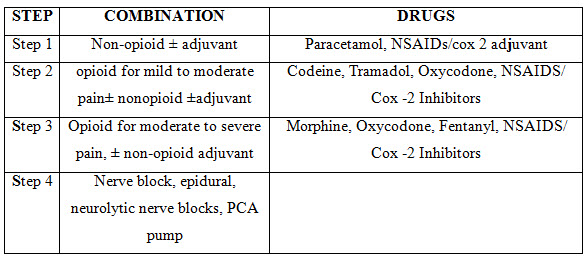
Opiates analgesics:
Narcotic analgesic drugs like oxycodone, butorphanol, meperidine, hydromorphone is effective but generally should be reserved for medications in treating severe infrequent headache in whose conventional therapies are contraindicated or as rescue medications after patients have failed to conventional therapies, opioid therapy should be supervised closely (Weitzel 1999) shown in Table No. 4 below.
Table No. 4: WHO analgesic ladder (Phillips et al, 1998)
ANTI -EMETICS:
Adjunctive antiemetic therapy is useful for combating the nausea and vomiting that accompany migraine headache and medication used to treat acute attacks eg: ergotamine tartrate, dihydroergotamine and ergotamine are useful in treating moderate to severe attacks of migraine (Silberstein 2000). Dihydroergotamine in injectable form is more effective than nasal spray but with more side effects. A single dose of anti-emetics such as metoclopramide, chlorpromazine administered 15-30 minutes before ingestion of oral absorptive migraine medication is often sufficient. Metaclopramide used to reverse gastroparesis and improve absorption from gastro- intestinal tract during severe attacks. Dopamine antagonist drugs have successfully used as monotherapy for treating intractable headache. Drowsiness and dizziness were occasionally reported in migraineurs with the use of dopamine antagonist (Matchar, 2000).
Triptans:
Triptans or serotonin receptor agonists have a significant advance in migraine pharmacotherapy; this class includes sumatriptan, zolmitriptan, naratriptan, etc. Relief of migraine headache results with three key actions i.e., vasoconstriction of intracranial blood vessels, inhibition of vasoactive neuropeptides, interruption of pain signal transmission in trigeminal nuclei through stimulation of 5 HT ID receptors (Ferrari 1998,Hargreaves 1999). The triptans are first line therapy for patients with moderate to severe migraine or rescue therapy when non-specific medications are ineffective, as compared to first generation (sumatriptan), second generation triptan (naratriptan) shows high bioavailability and longer half life (Tfelt et al 2000, Deleu, 2000). First generation triptans (44%) shows more recurrence than second generation triptans (17%) (Mathew et al 2000, Stark 2000). Triptans are contraindicated in patients with history of ischemic heart disease, uncontrolled hypertension, cerebrovascular diseases and they are also contraindicated in patients with hemiplegic and basilar migraine. Concomitant therapy with Selective Serotonin Reuptake Inhibitors (SSRI) should be carefully monitored because of isolated reports of serotonin syndrome in sumatriptan treated patients. This drugs have revolutionized many lives of severe migraine and act as powerful option for migraine attack .These are available various dosage forms like sprays, tablets, injections and suppositories ( Goadsby et al. 2002). Sumatriptan is contraindicated in pregnancy and lactation as it is less teratogenic but with high preterm births (Evans, 2008) and even excreted in breast milk (Horton et al. 1996). Almotriptan 12.5 mg has shown to abate migraine attack effectively when given in early phase of attack within 1 hour (Goadsby, 2008).
Prophylactic Treatment:
β - blockers are widely used drugs for migraine prophylaxis with intrinsic sympathomimetic activity are ineffective for migraine prophylaxis. β blockers are used with caution in patients with cardiovascular diseases and asthma. They reduce the brain cell activities which are involved in migraine. These are generally available in tablets and capsules forms (migrainetrust.org).
Amitriptyline is anti-depressant used in migraine prophylaxis it reduces frequency, severity and duration of migraine attacks (Ramadan, 2000). Other tricyclic anti-depressants have shown beneficial effects in small doses in treating migraine prophylaxis. They acts as antagonist of 5-HT2 receptor or suppresses serotonergic neuronal activity in brain stem (Silberstein 2000, 2002).
Anticonvulsants (valproic acid and divalproex sodium) 1:1 can reduce frequency of headaches by atleast 50% in up to 65% of migraineurs. Its mechanism is unclear in migraine (Silberstein 2002).
Calcium channel blockers, among this class verapamil is a drug of choice for prevention of migraine it is generally considered as second or third-line prophylactic agent with established clinical benefit are ineffective or contraindicated (Silberstein 2000, Goadsby 2000) and flunarizine (sibelium) which is generally prescribed by specialist. These drugs reduce calcium entry into neurons making them less excitable and blocks dopamine receptors in brain. (migrainetrust.org)
New developments in migraine therapy:
Botulinum toxin type A: (onabotulinum toxin A; BTA) It inhibits the release of acetylcholine at motor nerve terminals (Simpson, 1981). This action led to its use in the treatment of movement disorders, such as dystonia, post-stroke spasticity and hyperhidrosis (Jankovic, 2004) and neuropathic pain, lower back pain, myofascial pain, bladder pain (migrainetrust.org). Its cosmetic use suggests the potential benefits in headache. Basic experimental studies showed anti-nociceptive properties in some standard models, such as rats with formalin-induced pain, (Cui et al., 2004) which provided the rationale for its development in headache prevention (Aoki, 2005). According to rami burstein, botulinum toxin inhibits pain in chronic migraine by reducing expression of certain pain pathways involving nerve cells in trigeminovascular system that plays a key role in the headache phase of migraine attack.
Neuromodulation: Neuromodulatory approaches are currently focusing on the stimulation of the Greater Occipital Nerve (GON). The targeted synapses and neurons are located in the trigeminocervical complex and receive convergent input from the GON as well as from the trigeminal nerve (Doare et al, 2006). The functional imaging studies have shown that central processing of migraine pain signals in the thalamus could be modified by GON stimulation (Matharu et al, 2004). The use of occipital nerve stimulation for the treatment of intractable head pain in human beings was first proposed in 1999, when a series of cases of intractable occipital neuralgia responding to occipital nerve stimulation were reported (Weiner et al, 1999) these device (gamma core) a trans cutaneous vagus nerve stimulator is placed on the sides of neck where the stimulation is increased slowly and muscles contractions are felt under skin. It is held about 90 seconds.
• Pain relief in 20 % of patients within 2 hours of use
• Recovery from disability caused by migraine
• Relief of sickness, photophobia and phonophobia.( migrainetrust.org)
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
PREVALENCE:
Migraine is neurological disorder that affects 10% of adult population in the United States (18% women and 6% men). Below the age of 12, migraine is common in boys than girls and after puberty (Silberstein, Lipton 2002), prevalence increases 2-3 times in women than men. The questionnaire was returned by 1883 subjects (83.5%). Transformed migraine was diagnosed in 45 (50.6%) of subjects with chronic headache and 2.4% of all subjects (Jestis et al, 1999). The global burden of disease study 2010 (GBD2010) found tension type headache and migraine to be the 2nd and 3rd most prevalent disorders worldwide (Vos et al., 2012).
CONCLUSION:
Migraine is most common type of primary headache. If diagnosed earlier we can reduce the co- morbidities and enhance the quality of life. Both non-pharmacologic and pharmacologic therapy has a great impact in reducing the migraine attack. Advance in therapy of migraine like SSRI’s, triptans, neuromodulation in acute attack’s reduce the burden on patient. Providing awareness about migraine is essential for good results and great impact in prevention of migraine.
REFERENCES:
1.Alvin Lake, Joseph Rainey, James D Papsdorf. Biofeedback and Rational-Emotive therapy in the management of migraine headache. Journal of Applied Behavior Analysis. 1979; 12:127-140.
2.Aoki KR. Review of a proposed mechanism for the antinociceptive action of botulinum toxin type A. Neurotoxicology 2005; 26: 785–93.
3.Andrasik F.behavioural management of migraine headache .biomed pharmacotherapy 1996;50:52-57.
4.Bakal DA, Demejen S, Kaganov JA. Cognitive behavioural treatment of headache. Headache. 1981; 21:81-86.
5.Bartleson JD. Treatment of migraine headache. Mayo Clin Proc. 1999; 74:702-708.
6.Cui M, Khanijou S, Rubino J, Aoki KR. Subcutaneous administration of botulinum toxin A reduces formalin-induced pain. Pain 2004; 107: 125–33.
7.Dalessio DJ. Diagnosing the severe headache. Neurology. 1994; 44(3);s6-s12.
8.Deleu D, Hanseens Y. Current and emerging second generation triptans in acute migraine therapy: a comparative review. J Clin Pharmacol. 2000; 40:687-700.
9.Deshmukh SB,Meyer JS:cyclic changes in platelet dynamics and the pathogenesis and prophylaxis of migraine .Headache 17:101-108,1977.
10.Elliott KJ. Taxonomy and Mechanisms of Neuropathic Pain. Semin Neurol. 1994; (14)3:195-205.
11.E.P. Calandre, Jhidalgo J., Garci A Lieva.Trigger point evaluation in migraine patients: an indication of peripheral sensitization linked to migraine predisposition? European Journal of Neurology. 2006; 13:244-249.
12.Evans EW, Lorber KC. Use of 5-HT11 agonists in pregnancy. Ann Pharmacother 2008; 42: 543–49.
13.Fettes I. Migraine in Menopause. Neurology. 1999; 53(1):s29-s33.
14.Ferrari MD. Migraine. Lancet. 1998; 351:1043-1051.
15.Glover V ,Littlewood J ,Sandler M,peatfield R ,et al.why is platelet monoamine oxidase activity low in some headache patients ?in Rose FC (ed) :Advances in migraine research and therapy .New York ,Raven press ,1982 ,pp 127-132.
16.Goadsby PJ, Zanchin G, Geraud G, et al. Early vs. non-early intervention in acute migraine—‘Act when Mild (AwM)’. A double-blind, placebo-controlled trial of almotriptan. Cephalalgia 2008; 28: 383–91. 74
17.Goadsby PJ, Lipton RB, Ferrari MD. Migraine—current understanding and treatment. N Engl J Med 2002; 346: 257–70.
18.Hargreaves RJ, Shepheard SL. Pathophysiology of migraine-new insights. Can J Neurol Sci. 1999; 26 (l3):S12-S19.
19.Jankovic J. Botulinum toxin in clinical practice. J Neurol Neurosurg Psychiatry 2004; 75: 951–57.
20.Jestis castilo,MD et al.Epidemology of chronic daily headache in the general population.Headache 1999;39,190-t 96.
21.Kakigi R, Nakata H, Inui K, et al. Intracerebral pain processing in a yoga master who claims not to feel pain during meditation. Eur J Pain. 2005;9:581-589.
22.Kim DH, Moon YS, Kim HS, et al. Meditation and yoga reduce emotional stress of chronic pain. Prog NeuropsychopharmacolBiolPsychiatry.2005;29:327331.
23.Krymchantowski AV.acute treatment of migraine .Breaking the paradigm of momotherapy .BMC Neurol 2004; 4:4.DOL 10.1186/1474-2377-4
24.Landy S.Migraine throughout the life cycle .Treatment through the ages .neurology 2004:62(suppl 2):S2-8.
25.Lipton RB, Diamond S, Reed ML, et al. Migraine diagnosis and treatment: results of the American migraine study. Headache. 2001; 41:538-645.
26.Le Doare K, Akerman S, Holland PR, et al. Occipital aff erent activation of second order neurons in the trigeminocervical complex in rat. Neurosci Lett 2006; 403: 73–77 .
27.Matchar DB, Young WB, Rosenberg JA, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks .the USheadache consortium, accessed at www.aan.com/professional/practice /guidelines,2000.
28.Mathew N, Kailasam J, Gentry P, Chernyshev O. Treatment of non responders to oral sumatriptan with zolmitriptan and rizatriptan: a comparative open trial. Headache. 2000; 40:464-465.
29.Matharu MS, Bartsch T, Ward N, Frackowiak RSJ, Weiner RL, Goadsby PJ. Central neuromodulation in chronic migraine patients with suboccipital stimulators: a PET study. Brain 2004; 127: 220–30.
30.Mel R. Respiration. In: A Physiological Handbook for Teachers of Yogasana. Tucson, Arizona: Fenestra Books; 2002;373-382.
31.Olesen J et al, Headache classification committee of the international headache society .the international classification of headache disorders,2nd ed .cephalalgia 2004;24( 1 ):1-151.
32.Olesen J ;Migraine and regional cerebral blood flow ,Trends Neurolsci 8:318-321,1985.
33.Pasero C, Paice JA, McCaffery M. Basic mechanisms underlying the causes and effects of pain. In: McCaffery M, Pasero C, eds. Pain. St. Louis, Mosby, 1999:15–34
34.Peter J Goadsby,Neil H .Raskin. Headache. Harrison’s priniciples of internal medicine, 17th edition.
35.Peter J Goadsby, Till sprenger. Current practice and future directions in the prevention and acute management of migraine. lancet neurol. 2010; 9:285-98.
36.P.J. John et al. Effectiveness of Yoga Therapy in the Treatment of Migraine Without Aura: A Randomized Controlled Trial, (Headache 2007;47:654-661)
37.Pryse-Phillips, Dodick, Edmeads, et al.Guidelines for the nonpharmacologic management of migraine in clinical practice . CMAJ 1998;159:47-54
38.Ramadan NM, Silberstein SD, Freitag FG, et al. Evidence based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine .accessed at www.aan.com/professional/practice /guidelines,2000.
39.Richardson GM, Mcgrath PJ. Cognitive behavioural therapy for migraine headaches :a minial therapist contact approach. Headache. 1989; 29:352-357.
40.Rydzewski W,Wachowicz B:adenosine nucleotides in platelets in and between migraine attacks .in Greene (ed):current concepts in migraine research .New York ,Raven press ,1978,pp 153 -158.
41.Saito A ,Lee TJF .Serotonin as an alternative transmitter in large cerebral arteries of the rabbit .Circ Res 60:220-228,1987.
42.Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population based study. Pain 2003; 106: 81–89
43.Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. J Neurol Neurosurg Psychiatry. 1960, 23:23-32.
44.Silberstein CGH. Current concepts of migraine and its treatment. Neurologia. 1999; 14:67-77.
45.Silberstein SD. Practice Parameter: Evidence based guidelines for migraine headache (an evidence based review). Neurology. 2000; 55:754-763.
46.Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalagia 2002; 22:491-512.
47.Silberstein SD ,lipton RB,goadsby PJ .Headache in clinical practice.london ,martin Dunitz ,2002:21-33,69-128.
48.Silberstein SD, Goadsby PJ, Lipton RB. Management of migraine: An algorithmic approach. Neurology. 2000; 55(2):S46–52.
49.Simpson LL. The origin, structure, and pharmacological activity of botulinum toxin. Pharmacol Rev 1981; 33: 155–88.
50.Sorbi M, Tellegen B. Multimodal migraine treatment. does thermal biofeedback add to the outcomes? Headache. 1984; 24:249-255.
51.Stewartwf, Liptonrb, Celentanodd, et al. Prevalence of migraine headache in the United States, relation to age, income, race and other sociodemographic factors. JAMA. 1992; 267:64-69.
52.Stark S, Spiering E, Mc Neal et al. Naratriptan efficacy in migraineurs who respond poorly to oral sumatriptan. Headache. 2000; 40:513-520.
53.Terry J. Baumann. Pain Management. Pharmacotherapeutics- A Pathophysiologic Approach, 6th Edition, The McGraw-Hill Companies, Inc. United States, 2005; 1089-1104.
54.Tfelt Hansen P, De Vries P, Saxena PR. Triptans in migraine: A comparative review of pharmacology, pharmacokinetics and efficacy. Drugs. 2000; 60(6):1259-1287.
55.Vos T,Flaxman AD et al .years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010:A systematic analysis for the Global burden of disease study 2010.Lancet.2012;380:2163-2196.
56.www.migraine.org.uk/triggers
57. www.migrainetrust.org
58.www.i-h-s.org /2004.
59.www.hartp.neurology.ucla.edu
60.Warner G, Lance JW. Relaxation therapy in migraine and tension headache. Med J Aust. 1975; 1:298-301.
61.Weitzel KW, Thomas ML, Small RE, Goode JV. Migraine: A comprehensive review of new treatment options. Pharmacotherapy. 1999; 19(8):957-973.
62.Weiner RL, Reed K. Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation 1999; 2: 217–21.
63.Wojnar-Horton RE, Hackett LP, Yapp P, Dusci LJ, Paech M, Ilett KF. Distribution and excretion of sumatriptan in human milk. Br J Clin Pharmacol 1996; 41: 217–21.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









