What is a mammogram?
A mammogram is an x-ray picture of the breast.
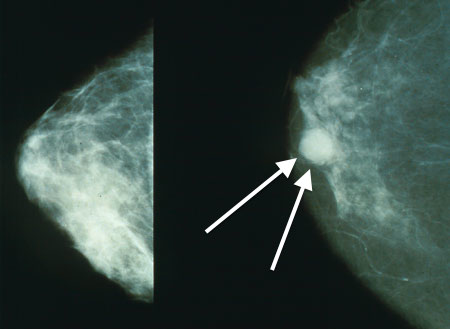
Mammograms can be used to check for breast cancer in women who have no signs or symptoms of the disease. This type of mammogram is called a screening mammogram. Screening mammograms usually involve two x-ray pictures, or images, of each breast. The x-ray images make it possible to detect tumors that cannot be felt. Screening mammograms can also find microcalcifications (tiny deposits of calcium) that sometimes indicate the presence of breast cancer.
Mammograms can also be used to check for breast cancer after a lump or other sign or symptom of the disease has been found. This type of mammogram is called a diagnostic mammogram. Besides a lump, signs of breast cancer can include breast pain, thickening of the skin of the breast, nipple discharge, or a change in breast size or shape; however, these signs may also be signs of benign conditions. A diagnostic mammogram can also be used to evaluate changes found during a screening mammogram or to view breast tissue when it is difficult to obtain a screening mammogram because of special circumstances, such as the presence of breast implants.
[adsense:336x280:8701650588]
How are screening and diagnostic mammograms different?
Diagnostic mammography takes longer than screening mammography because more x-rays are needed to obtain views of the breast from several angles. The technician may magnify a suspicious area to produce a detailed picture that can help the doctor make an accurate diagnosis.
What are the benefits of screening mammograms?
Early detection of breast cancer with screening mammography means that treatment can be started earlier in the course of the disease, possibly before it has spread. Results from randomized clinical trials and other studies show that screening mammography can help reduce the number of deaths from breast cancer among women ages 40 to 74, especially for those over age 50 (1). However, studies to date have not shown a benefit from regular screening mammography in women under age 40 or from baseline screening mammograms (mammograms used for comparison) taken before age 40.
What are some of the potential limitations of screening mammograms?
False-positive results. False-positive results occur when radiologists decide mammograms are abnormal but no cancer is actually present. All abnormal mammograms should be followed up with additional testing (diagnostic mammograms, ultrasound, and/or biopsy) to determine whether cancer is present.
False-positive results are more common for younger women, women who have had previous breast biopsies, women with a family history of breast cancer, and women who are taking estrogen (for example, menopausal hormone therapy).
False-positive mammogram results can lead to anxiety and other forms of psychological distress in affected women. The additional testing required to rule out cancer can also be costly and time consuming and can cause physical discomfort.
Overdiagnosis and overtreatment. Screening mammograms can find cancers and cases of ductal carcinoma in situ (DCIS, a noninvasive tumor in which abnormal cells that may become cancerous build up in the lining of breast ducts) that need to be treated. However, they can also find cancers and cases of DCIS that will never cause symptoms or threaten a woman’s life, leading to "overdiagnosis" of breast cancer. Treatment of these latter cancers and cases of DCIS is not needed and leads to "overtreatment." Overtreatment exposes women unnecessarily to the adverse effects associated with cancer therapy.
Because doctors often cannot distinguish cancers and cases of DCIS that need to be treated from those that do not, they are all treated.
False-negative results. False-negative results occur when mammograms appear normal even though breast cancer is present. Overall, screening mammograms miss about 20 percent of breast cancers that are present at the time of screening.
The main cause of false-negative results is high breast density. Breasts contain both dense tissue (i.e., glandular tissue and connective tissue, together known as fibroglandular tissue) and fatty tissue. Fatty tissue appears dark on a mammogram, whereas fibroglandular tissue appears as white areas. Because fibroglandular tissue and tumors have similar density, tumors can be harder to detect in women with denser breasts.
False-negative results occur more often among younger women than among older women because younger women are more likely to have dense breasts. As a woman ages, her breasts usually become more fatty, and false-negative results become less likely. False-negative results can lead to delays in treatment and a false sense of security for affected women.
Some of the cancers missed by screening mammograms can be detected by clinical breast exams (physical exams of the breast done by a health care provider).
Finding cancer early does not always reduce a woman’s chance of dying from breast cancer. Even though mammograms can detect malignant tumors that cannot be felt, treating a small tumor does not always mean that the woman will not die from the cancer. A fast-growing or aggressive cancer may have already spread to other parts of the body before it is detected. Women with such tumors live a longer period of time knowing that they likely have a fatal disease.
In addition, screening mammograms may not help prolong the life of a woman who is suffering from other, more life-threatening health conditions.
Radiation exposure. Mammograms require very small doses of radiation. The risk of harm from this radiation exposure is extremely low, but repeated x-rays have the potential to cause cancer. The benefits of mammography, however, nearly always outweigh the potential harm from the radiation exposure. Nevertheless, women should talk with their health care providers about the need for each x-ray. In addition, they should always let their health care provider and the x-ray technician know if there is any possibility that they are pregnant, because radiation can harm a growing fetus.
Where can I find current recommendations for screening mammography?
Many organizations and professional societies, including the United States Preventive Services Task Force (which is convened by the Agency for Healthcare Research and Quality, a federal agency), have developed guidelines for mammography screening. All recommend that women should talk with their doctor about the benefits and harms of mammography, when to start screening, and how often to be screened.
Although NCI does not issue guidelines for cancer screening, it conducts and facilitates basic and translational research that informs standard clinical practice and medical decision making that other organizations may use to develop their guidelines.
[adsense:468x15:2204050025]
What is the best method of detecting breast cancer as early as possible?
Getting a high-quality screening mammogram and having a clinical breast exam on a regular basis are the most effective ways to detect breast cancer early.
Checking one’s own breasts for lumps or other unusual changes is called a breast self-exam, or BSE. This type of exam cannot replace regular screening mammograms or clinical breast exams. In clinical trials, BSE alone was not found to help reduce the number of deaths from breast cancer.
Although regular BSE is not specifically recommended for breast cancer screening, many women choose to examine their own breasts. Women who do so should remember that breast changes can occur because of pregnancy, aging, or menopause; during menstrual cycles; or when taking birth control pills or other hormones. It is normal for breasts to feel a little lumpy and uneven. Also, it is common for breasts to be swollen and tender right before or during a menstrual period. If a woman notices any unusual changes in her breasts, she should contact her health care provider.
What is the Breast Imaging Reporting and Database System (BI-RADS®)?
The American College of Radiology (ACR) has established a uniform way for radiologists to describe mammogram findings. The system, called BI-RADS, includes seven standardized categories, or levels. Each BI-RADS category has a follow-up plan associated with it to help radiologists and other physicians appropriately manage a patient’s care.
Breast Imaging Reporting and Database System (BI-RADS)
| Category | Assessment | Follow-up |
|---|---|---|
| 0 | Need additional imaging evaluation | Additional imaging needed before a category can be assigned |
| 1 | Negative | Continue regular screening mammograms (for women over age 40) |
| 2 | Benign (noncancerous) finding | Continue regular screening mammograms (for women over age 40) |
| 3 | Probably benign | Receive a 6-month follow-up mammogram |
| 4 | Suspicious abnormality | May require biopsy |
| 5 | Highly suggestive of malignancy (cancer) | Requires biopsy |
| 6 | Known biopsy-proven malignancy (cancer) | Biopsy confirms presence of cancer before treatment begins |
What should women with breast implants do about screening mammograms?
Women with breast implants should continue to have mammograms. (A woman who had an implant following a mastectomy should ask her doctor whether a mammogram of the reconstructed breast is necessary.) It is important to let the mammography facility know about breast implants when scheduling a mammogram. The technician and radiologist must be experienced in performing mammography on women who have breast implants. Implants can hide some breast tissue, making it more difficult for the radiologist to detect an abnormality on the mammogram. If the technician performing the procedure is aware that a woman has breast implants, steps can be taken to make sure that as much breast tissue as possible can be seen on the mammogram. A special technique called implant displacement views may be used.
What is digital mammography? How is it different from conventional (film) mammography?
Digital and conventional mammography both use x-rays to produce an image of the breast; however, in conventional mammography, the image is stored directly on film, whereas, in digital mammography, an electronic image of the breast is stored as a computer file. This digital information can be enhanced, magnified, or manipulated for further evaluation more easily than information stored on film.
Because digital mammography allows a radiologist to adjust, store, and retrieve digital images electronically, digital mammography may offer the following advantages over conventional mammography:
-
Health care providers can share image files electronically, making long-distance consultations between radiologists and breast surgeons easier.
-
Subtle differences between normal and abnormal tissues may be more easily noted.
-
Fewer follow-up procedures may be needed.
-
Fewer repeat images may be needed, reducing the exposure to radiation.
To date, there is no evidence that digital mammography helps to reduce a woman’s risk of dying from breast cancer compared with film mammography. Results from a large NCI-sponsored clinical trial that compared digital mammography with film mammography found no difference between digital and film mammograms in detecting breast cancer in the general population of women in the trial; however, digital mammography appeared to be more accurate than conventional film mammography in younger women with dense breasts (2). A subsequent analysis of women aged 40 through 79 who were undergoing screening in U.S. community-based imaging facilities also found that digital and film mammography had similar accuracy in most women. Digital screening had higher sensitivity in women with dense breasts (3).
Some health care providers recommend that women who have a very high risk of breast cancer, such as those with a known mutation in either the BRCA1 or BRCA2 gene or extremely dense breasts, have digital mammograms instead of conventional mammograms; however, no studies have shown that digital mammograms are superior to conventional mammograms in reducing the risk of death for these women.
Digital mammography can be done only in facilities that are certified to practice conventional mammography and have received FDA approval to offer digital mammography. The procedure for having a mammogram with a digital system is the same as with conventional mammography.
What is 3D mammography?
Three-dimensional (3D) mammography, also known as breast tomosynthesis, is a type of digital mammography in which x-ray machines are used to take pictures of thin slices of the breast from different angles and computer software is used to reconstruct an image. This process is similar to how a computed tomography (CT) scanner produces images of structures inside of the body. 3D mammography uses very low dose x-rays, but, because it is generally performed at the same time as standard two-dimensional (2D) digital mammography, the radiation dose is slightly higher than that of standard mammography. The accuracy of 3D mammography has not been compared with that of 2D mammography in randomized studies. Therefore, researchers do not know whether 3D mammography is better or worse than standard mammography at avoiding false-positive results and identifying early cancers.
What other technologies are being developed for breast cancer screening?
NCI is supporting the development of several new technologies to detect breast tumors. This research ranges from methods being developed in research labs to those that are being studied in clinical trials. Efforts to improve conventional mammography include digital mammography, magnetic resonance imaging (MRI), positron emission tomography (PET) scanning, and diffuse optical tomography, which uses light instead of x-rays to create pictures of the breast.
Selected References
-
Mandelblatt JS, Cronin KA, Bailey S, et al. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Annals of Internal Medicine 2009;151(10):738-747.
-
Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. New England Journal of Medicine 2005; 353(17):1773-1783.
-
Kerlikowske K, Hubbard RA, Miglioretti DL, et al. Comparative effectiveness of digital versus film-screen mammography in community practice in the United States: a cohort study. Annals of Internal Medicine 2011;155(8):493-502.
Credit: The National Cancer Institute, US









