 About Authors:
About Authors:
Mr. Satyanand Tyagi*, Patel Chirag J1, Asheesh Singh2
*President, Tyagi Pharmacy Association & Scientific Writer (pharmacy), Chattarpur, New Delhi, India-110074.
Prof. Satyanand Tyagi is a life time member of various pharmacy professional bodies like IPA, APTI and IPGA. He has published various research papers and review articles. His academic works include 52 Publications (44 Review Articles and 08 Research Articles of Pharmaceutical, Medicinal and Clinical Importance, published in standard and reputed National and International Pharmacy journals; Out of 52 publications, 11 are International Publications).
He has published his papers almost in different specialization of Pharmacy field...His research topics of interest are neurodegenerative disorders, diabetes mellitus, cancer, rare genetic disorders, psycho-pharmacological agents as well as epilepsy.
1Department of Pharmaceutics, Maharishi Arvind Institute of Pharmacy, Mansarovar, Jaipur, Rajasthan, India-302020.
2Research Associate, Center for Research and Development, Ipca Laboratories Ltd Ratlam, Madhya Pradesh, India-457114.
*sntyagi9 @yahoo.com, +91-9871111375 / 9582025220
ABSTRACT:
Prior studies have suggested that depressed people with evidence of high inflammation are less likely to respond to traditional treatments for the disorder, including anti-depressant medications and psychotherapy. This study was designed to see whether blocking inflammation would be a useful treatment for either a wide range of people with difficult-to-treat depression or only those with high levels of inflammation. The study employed infliximab, one of the new biologic drugs used to treat autoimmune and inflammatory diseases such as rheumatoid arthritis and inflammatory bowel disease. A biologic drug copies the effects of substances naturally made by the body's immune system. In this case, the drug was an antibody that blocks tumour necrosis factor (TNF), a key molecule in inflammation that has been shown to be elevated in some depressed individuals. Study participants all had major depression and were moderately resistant to conventional antidepressant treatment. Each participant was assigned either to infliximab or to a non-active placebo treatment. When investigators looked at the results for the group as a whole, no significant differences were found in the improvement of depression symptoms between the drug and placebo groups. However, when the subjects with high inflammation were examined separately, they exhibited a much better response to infliximab than to placebo.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1493
INTRODUCTION
Inflammation is a protective tissue response to injury or destruction of tissues, which serves to destroy, dilute, or wall off both the injurious agent and the injured tissues. Inflammation may be acute or chronic. Its cardinal signs are redness (rubor), heat (calor), swelling (tumor), and pain (dolor), often accompanied by loss of function. The process begins with a transitory vasoconstriction, and then is followed by a brief increase in vascular permeability. The second stage is prolonged and consists of sustained increase in vascular permeability, exudation of fluids from the vessels, clustering of leukocytes along the vessel walls, phagocytosis of microorganisms, deposition of fibrin in the vessel, disposal of the accumulated debris by macrophages, and finally migration of fibroblasts to the area and development of new, normal cells. The severity, timing, and local character of any particular inflammatory response depend on the cause, the area affected, and the condition of the host. Histamine, kinins, and various other substances mediate the inflammatory process. Defining inflammation according to clinical signs and symptoms has major limitations, as in most cases the cellular processes and signals that underlie the cardinal signs occur at a sub clinical level and do not give rise to any heat, redness, swelling, or pain [1]. For example, the inflammation of delayed onset muscular soreness may cause tenderness on palpation or mild discomfort [2], but no redness or swelling. Broadening the definition of inflammation to include one or a subset of the cardinal signs is not a solution, as areas of swelling, pain, and tenderness may have a wide variety of non-inflammatory causes. For example, regions of muscle spasm (sometimes called “myositis”) and many cases of tendinosis (often called “tendinitis”[3]) are often confused with inflammation, because of the local pain and swollen nature of the tissue.Depression is a medical illness that causes a persistent feeling of sadness and loss of interest.
Depression can cause physical symptoms, too. Also called major depression, major depressive disorder and clinical depression, it affects how person feel, think and behave. Depression can lead to a variety of emotional and physical problems. Person may have trouble doing normal day-to-day activities, and depression may make feel as if life isn't worth living. Depression is an extremely common psychiatric condition, about which a variety of neurochemical theories exist, and for which a corresponding variety of different types of drug are used in treatment.
It is a field in which therapeutic empiricism has led the way, with mechanistic understanding tending to lag behind, part of the difficulty being that animal models cannot address the mood change that defines the human condition. Depression is a state of low mood and aversion to activity that can have a negative effect on a person's thoughts, behavior, feelings, world view and physical well-being. Depressed people may feel sad, anxious, empty, hopeless, worried, helpless, worthless, guilty, irritable, hurt, or restless. They may lose interest in activities that once were pleasurable; experience loss of appetite or overeating; have problems concentrating, remembering details, or making decisions; and may contemplate or attempt suicide. Insomnia, excessive sleeping, fatigue, loss of energy, or aches, pains or digestive problems that are resistant to treatment may be present [4]. Depressed mood is not necessarily a psychiatric disorder. It is a normal reaction to certain life events, a symptom of some medical conditions, and a side effect of some medical treatments. Depressed mood is also a primary or associated feature of certain psychiatric syndromes such as clinical depression. Depression is the most common of the affective disorders (defined as disorders of mood rather than disturbances of thought or cognition); it may range from a very mild condition, bordering on normality, to severe (psychotic) depression accompanied by hallucinations and delusions. Worldwide, depression is a major cause of disability and premature death. In addition to the significant suicide risk, depressed individuals are more likely to die from other causes, such as heart disease or cancer. The symptoms of depression include emotional and biological components.
SYMPTOMS OF DEPRESSION
[adsense:468x15:2204050025]
Emotional symptoms:
* misery, apathy and pessimism
* low self-esteem: feelings of guilt, inadequacy and ugliness
* Indecisiveness, loss of motivation.
Biological symptoms:
*retardation of thought and action
* loss of libido
* sleep disturbance and loss of appetite.
A number of psychiatric syndromes feature depressed mood as a main symptom. The mood disorders are a group of disorders considered to be primary disturbances of mood. These include major depressive disorder (MDD, commonly called major depression or clinical depression) where a person has at least two weeks of depressed mood or a loss of interest or pleasure in nearly all activities; and dysthymia, a state of chronic depressed mood, the symptoms of which do not meet the severity of a major depressive episode. Another mood disorder, bipolar disorder, features one or more episodes of abnormally elevated energy levels, cognition and mood, but may also involve one or more depressive episodes [5]. When the course of depressive episodes follows a seasonal pattern, the disorder (major depressive disorder, bipolar disorder, etc) may be described as a seasonal affective disorder. Outside the mood disorders: borderline personality disorder commonly features depressed mood; adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode [6]; and posttraumatic stress disorder, an anxiety disorder that sometimes follows trauma, is commonly accompanied by depressed mood [7].
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Depression and Inflammation
Inflammation in the body is common to many diseases, including high blood pressure, coronary artery disease, and diabetes. Depression has also been linked to an inflammation marker in blood called C-reactive protein (CRP). Dr. William Copeland at Duke University Medical Center and his colleagues tested the direction of association between depression and CRP in a large sample of adolescent and young adult volunteers. By following the children into young adulthood, they were able to assess the changes over time in both their CRP levels and any depressive symptoms or episodes. They found that elevated levels of CRP did not predict later depression, but the number of cumulative depressive episodes was associated with increased levels of CRP. "Our results support a pathway from childhood depression to increased levels of CRP, even after accounting for other health-related behaviours that are known to influence inflammation.
We found no support for the pathway from CRP to increased risk for depression," said Copeland. These findings suggest that, by this measure, depression is more likely to contribute to inflammation in the body as opposed to arise as a consequence of inflammation in the body. The highest levels of CRP were found in those who had endured the wear and tear of multiple depressive episodes. This suggests the possibility that long-term emotional distress, beginning in childhood, may lay the foundation for inflammatory processes that lead, in middle age, to cardiovascular disease and diabetes. "Depression is a recurring disorder for many people. Thus the finding that repeated episodes of depression contribute to inflammation in the body highlights a potentially important role for untreated depression as a contributor to a range of serious medical problems," commented Dr. John Krystal, Editor ofBiological Psychiatry; “These data add to growing evidence of the medical importance of effectively treating depression” [8, 9].
TARGETING INFLAMMATION TO TREAT DEPRESSION
Researchers at Emory University have found that a medication that inhibits inflammation may offer new hope for people with difficult-to-treat depression. The study was published Sept. 3 in the online version of Archives of General Psychiatry. "Inflammation is the body's natural response to infection or wounding, says Andrew H. Miller, MD, senior author for the study and professor of Psychiatry and Behavioural Sciences at Emory University School of Medicine; “However when prolonged or excessive, inflammation can damage many parts of the body, including the brain”. Prior studies have suggested that depressed people with evidence of high inflammation are less likely to respond to traditional treatments for the disorder, including anti-depressant medications and psychotherapy. This study was designed to see whether blocking inflammation would be a useful treatment for either a wide range of people with difficult-to-treat depression or only those with high levels of inflammation. The study employed infliximab, one of the new biologic drugs used to treat autoimmune and inflammatory diseases such as rheumatoid arthritis and inflammatory bowel disease.
Infliximab is a monoclonal antibody against tumor necrosis factor alpha (TNF-α) used to treat autoimmune diseases. Infliximab was approved by the U.S. Food and Drug Administration (FDA) for the treatment of psoriasis, Crohn's disease, ankylosing spondylitis, psoriatic arthritis, rheumatoid arthritis, and ulcerative colitis. Infliximab won its initial approval by the FDA for the treatment of Crohn's disease in August 1998.Infliximab works by binding to tumor necrosis factor alpha.
TNF-α is a chemical messenger (cytokine) and a key part of the autoimmune reaction. Originally, the action of infliximab (in rheumatoid arthritis) was assumed to work by blocking the action of TNF-α by preventing it from binding to its receptor in the cell. This still seems to be true. However, another TNF-α-neutralizing medication, etanercept (Enbrel), is worse than a placebo in Crohn's disease, so TNF-α-neutralization is not responsible for its powerful action in the latter disease [10]. Infliximab causes programmed cell death of TNF-α-expressing activated T lymphocytes, an important cell type mediating inflammation, but etanercept does not have this activity; now, resolution of activated T cells by infliximab is generally assumed to explain its efficacy in Crohn's disease [11].
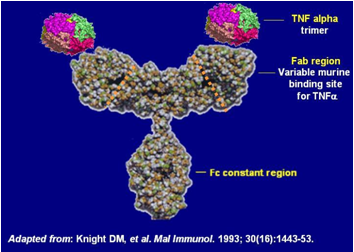
STRUCTURE OF INFLIXIMAB
A biologic drug copies the effects of substances naturally made by the body's immune system. In this case, the drug was an antibody that blocks tumour necrosis factor (TNF), a key molecule in inflammation that has been shown to be elevated in some depressed individuals. Study participants all had major depression and were moderately resistant to conventional antidepressant treatment. Each participant was assigned either to infliximab or to a non-active placebo treatment. When investigators looked at the results for the group as a whole, no significant differences were found in the improvement of depression symptoms between the drug and placebo groups. However, when the subjects with high inflammation were examined separately, they exhibited a much better response to infliximab than to placebo.
Inflammation in this study was measured using a simple blood test that is readily available in most clinics and hospitals and measures C-reactive protein or CRP; The higher the CRP, the higher the inflammation, and the higher the likelihood of responding to the drug [12]. "The prediction of an antidepressant response using a simple blood test is one of the holy grails in psychiatry," says Miller. "This is especially important because the blood test not only measured what we think is at the root cause of depression in these patients, but also is the target of the drug." "This is the first successful application of a biologic therapy to depression," adds Charles L. Raison, MD, first author of the study; “The study opens the door to a host of new approaches that target the immune system to treat psychiatric diseases” [13].
RELATED ASPECTS
Past studies have shown that there appears to be a correlation between chronic depression and the likelihood of dementia in the later years. Likewise, there are studies which indicate that inflammatory changes in the brain are pathological features of both depression and dementia. These findings have caused rheumatologists to forever be looking over their shoulders: Does the inflammation of the inflammatory diseases rheumatologists treat play a role in depression (and for that matter, dementia)? Perhaps the dysphoria experienced by so many patients with chronic illness is not due simply to the condition of being burdened with a chronic illness, but precipitated by the physiological processes which caused the disease itself. Recently, a Japanese team's findings on this subject were published in the journal, "Psychosomatic Medicine". Over 200 patients with rheumatoid arthritis were studied. They found that C-reactive protein (CRP), a marker of inflammation, was associated with elevated depression and pain scores; inflammation and depression were found to have an independent effect on patient-reported pain.
It appears that the relationship between inflammation and pain and depression is a complex one: Central and peripheral nervous system pain processing, hypothalamic-pituitary-adrenal interactions, and psychosocial factors all have important roles in the psychological response to inflammation. Rheumatologists may find themselves addressing these complex interactions as part of the clinical care given their patients. Many patients have continued disability, even after the use of the potent immune-suppressing drugs used to treat illnesses such as rheumatoid arthritis. Researchers will have to isolate and target the inflammatory mediators of depression, and not just those thought to cause swollen and painful joints.
And clinicians will require the skills and empathy to recognize depression, as a study published in "Biological Psychiatry" last year found that there was actually a decrease in inflammation in depressed patients treated with anti-depressants. Inflammation, pain and depression are a part of the tangled web in which so many patients are trapped. Let's hope further research can untangle some of the mysteries of that inscrutable mind-body nexus [14].
CONCLUSION
Targeting inflammation in the brain could help to treat those with depression that do not respond to standard medications. This is the finding of a new study at Emory University, which claims to have found a treatment to inhibit inflammation. The investigation follows on from previous research that suggests high levels of information are likely to reduce the likelihood of responding to treatment for people with depression. Using infliximab, a biologic drug used to treat autoimmune and inflammatory disease, Emory scientists were able to block tumor necrosis factor, which is a molecule in inflammation shown to be elevated in depressed patients. If confirmed in further studies, the drug could prove vital in targeting those that become unresponsive to treatment and may lead to further research on the role of inflammation in depression.
ACKNOWLEDGEMENT
The corresponding author, Prof. Satyanand Tyagi is highly thankful to his Parents, Teachers, wife Pooja, and daughter Tanisha for their moral support and encouragement. Last but not the least, support of all my students and the one above all of us, the omnipresent God, for answering my prayers for giving me the strength to plod on despite my constitution wanting to give up and throw in the towel, thank you so much Dear Lord.
REFERENCES
1. Gallin JI, Snyderman R. Overview. In: Gallin JI, Snyderman R, eds. Inflammation: basic principles and clinical correlates. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, 1–4.
2. MacIntyre DL, Reid WD, McKenzie DC, Delayed muscle soreness. The inflammatory response to muscle injury and its clinical implications, Sports Med, 1995, 20, 24–40.
3. Khan KM, Cook JL, Overuse tendon injuries: where does the pain come from? Sports Med Arthrosc Rev, 2000, 8, 17–31.
4. “Depression”. National Institute of Mental Health. 2009-09-23.
5. Gabbard, Glen O, Treatment of Psychiatric Disorders. 2 (3rd ed.). Washington, DC: American Psychiatric Publishing. p. 1296.
6. American Psychiatric Association 2000a, p. 355
7. Vieweg WV, Julius DA, Fernandez A, Beatty-Brooks M, Hettema JM, Pandurangi AK, “Posttraumatic stress disorder: clinical features, pathophysiology, and treatment", Am. J. Med, 2006, 119 (5), 383–90.
8. William E. Copeland, Lilly Shanahan, Carol Worthman, Adrian Angold, E. Jane Costello, Cumulative Depression Episodes Predict Later C - reactive protein Levels: A Prospective Analysis, Biological Psychiatry, 2012, 71 (1), 15.
9. sciencedaily.com/releases/2012/01/120105112235.htm
10. Van Den Brande JM, Peppelenbosch MP, Van Deventer SJ, Treating Crohn’s disease by inducing T lymphocyte apoptosis, Ann. N. Y. Acad. Sci., 2002,973, 166-180.
11. Van Den Brande JM, "Infliximab but not etanercept induces apoptosis in lamina propria T-lymphocytes from patients with Crohn's disease", Gastroenterology, 2003, 124 (7), 1774–1785.
12. Raison CL, Rutherford RE, Woolwine BJ, et al, A Randomized Controlled Trial of the Tumor Necrosis Factor Antagonist Infliximab for Treatment-Resistant Depression: The Role of Baseline Inflammatory Biomarkers, Archives of General Psychiatry, 2012, 10, 1-11.
13. sciencedaily.com/releases/2012/09/120903221132.htm
14. psychologytoday.com/blog/overcoming-pain/201001/matter-over-mind- inflammation-and-depression
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









