 About Authors:
About Authors:
Satyanand tyagi*, Raghvendra1
*President, Tyagi Pharmacy Association & Scientific Writer,
Chattarpur, New Delhi, India-110074.
Prof. Satyanand Tyagi is a life time member of various pharmacy professional bodies like IPA, APTI and IPGA. He has published various research papers and review articles. His academic works include 45 Publications (37 Review Articles and 08 Research Articles of Pharmaceutical, Medicinal and Clinical Importance, published in standard and reputed National and International Pharmacy journals; Out of 45 publications, 10 are International Publications).
1Department of Pharmaceutics, Aligarh College of Pharmacy,
Aligarh, U.P, India-202001.
*sntyagi9@yahoo.com, +91-9871111375 / 9582025220
ABSTRACT
Tak-875, a new treatment for type-2 diabetes, improves blood sugar control and is equally effective as glimepiride (Sulfonylurea, oral hypoglycaemic agent), but has a significantly lower risk of hypoglycaemia, according to a new study. It works by boosting the release of insulin from pancreatic beta cells when glucose and fatty acids rise in the blood, such as after a meal, which results in a fall in blood glucose levels. TAK-875 is a novel oral medication designed to enhance insulin secretion in a glucose dependent manner, which means that it has no effect on insulin secretion when glucose levels are normal, and as such has the potential to improve the control of blood sugar levels without the risk of hypoglycaemia. The pill belongs to a new class of treatments called GPR40 agonists, which activate a receptor that stimulates and regulates insulin production. New treatments are needed because of “the expected increase in the number of cases of Type 2 diabetes during the next few decades” and because some current drugs have “insufficient effect,” the researchers, led by Charles Burant at the University of Michigan Medical School, wrote in the study. Free fatty acid receptor 1 (FFA1), also known as G protein-coupled receptor 40 (GPR40), plays a vital role in stimulating and regulating the production of insulin. It works by boosting the release of insulin from pancreatic β-cells when glucose and fatty acids rise in the blood, such as after a meal. The release of insulin results in a fall in blood glucose levels. Drugs that activate the FFAR1 receptor have the potential to help diabetics release more insulin and improve control of blood glucose levels. This article gives an overview about this newly introduced drug TAK-875 and its role in treatment for type-2 diabetes.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1445
INTRODUCTION
Diabetes mellitus, or simply diabetes, is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced1. This high blood sugar produces the classical symptoms of polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). There are three main types of diabetes mellitus (DM). Type 1 DM results from the body's failure to produce insulin, and presently requires the person to inject insulin or wear an insulin pump. This form was previously referred to as "insulin-dependent diabetes mellitus" (IDDM) or "juvenile diabetes". Type 2 DM results from insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with an absolute insulin deficiency. This form was previously referred to as non insulin-dependent diabetes mellitus (NIDDM) or "adult-onset diabetes". The third main form, gestational diabetes occurs when pregnant women without a previous diagnosis of diabetes develop a high blood glucose level. It may precede development of type 2 DM.
[adsense:468x15:2204050025]
Other forms of diabetes mellitus include congenital diabetes, which is due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes. All forms of diabetes have been treatable since insulin became available in 1921, and type 2 diabetes may be controlled with medications. Both types 1 and 2 are chronic conditions that cannot be cured. Pancreas transplants have been tried with limited success in type 1 DM; gastric bypass surgery has been successful in many with morbid obesity and type 2 DM. Gestational diabetes usually resolves after delivery. Diabetes without proper treatments can cause many complications. Acute complications include hypoglycaemia, diabetic ketoacidosis, or nonketotic hyperosmolar coma. Serious long-term complications include cardiovascular disease, chronic renal failure, and diabetic retinopathy (retinal damage). Adequate treatment of diabetes is thus important, as well as bloo control and lifestyle factors such as smoking cessation and maintaining a healthy body weight.
Globally, as of 2012, an estimated 346 million people have type 2 diabetes2.
Diabetes Mellitus type 2(formerly non-insulin-dependent diabetes mellitus; NIDDM) or adult-onset diabetes
Diabetes mellitus type 2 is a metabolic disorder that is characterized by high blood glucose in the context of insulin resistance and relative insulin deficiency. This is in contrast to diabetes mellitus type 1 in which there is only dumb insulin deficiency due to destruction of islet cells in the pancreas. The classic symptoms are excess thirst, frequent urination, and constant hunger. Type 2 diabetes makes up about 90% of cases of diabetes with the other 10% due primarily to diabetes mellitus type 1 and gestational diabetes. Obesity is thought to be the primary cause of type 2 diabetes in people who are genetically predisposed to the disease. Type 2 diabetes is initially managed by increasing exercise and dietary modification. If blood glucose levels are not adequately lowered by these measures, medications such as metformin or insulin may be needed. In those on insulin there is typically the requirement to routinely check blood sugar levels. Rates of diabetes have increased markedly over the last 50 years in parallel with obesity. As of 2010 there are approximately 285 million people with the disease compared to around 30 million in 1985. Long-term complications from high blood sugar can include heart, strokes, diabetic retinopathy where eyesight is affected, kidney failure which may require dialysis, and poor circulation of limbs leading to amputations. The acute complication of ketoacidosis, a feature of type 1 diabetes, is uncommon3. However, nonketotic hyperosmolar coma may occur.
The development of type 2 diabetes is caused by a combination of lifestyle and genetic factors4, 5.While some are under personal control such as diet and obesity others such as increasing age, female gender, and genetics are not. A lack of sleep has been linked to type 2 diabetes6. This is believed to act through its effect on metabolism6. The nutritional status of a mother during fetal development may also play a role with one proposed mechanism being that of altered DNA methylation7.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to PharmaTutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Genetic causes and Pathophysilogy of diabetes mellitus type 2
Most cases of diabetes involve many genes with each being a small contributor to an increased probability of becoming a type 2 diabetic. If one identical twin has diabetes the chance of the other developing diabetes within their lifetime is greater than 90% while the rate for non-identical siblings is 25-50%. As of 2011, more than 36 genes have been found that contribute to the risk of type 2 diabetes8. All of these genes together still only account for 10% of the total heritable component of the disease. The TCF7L2 allele for example increases the risk of developing diabetes by 1.5 times and is the greatest risk of the common genetic variants. Most of the genes links to diabetes are involved in beta cell functions. There are a number of rare cases of diabetes that arise due to an abnormality in a single gene (known as monogenic forms of diabetes or "other specific types of diabetes"). These include maturity onset diabetes of the young (MODY), Donohue syndrome, and Rabson-Mendenhall syndrome, among others. Maturity onset diabetes of the young constitutes 1–5 % of all cases of diabetes in young people.
Type 2 diabetes is due to insufficient insulin production from beta cells in the setting of insulin resistance. Insulin resistance, which is the inability of cells to respond adequately to normal levels of insulin, occurs primarily within the muscles, liver and fat tissue. In the liver, insulin normally suppresses glucose release. However in the setting of insulin resistance, the liver inappropriately releases glucose into the blood. The proportion of insulin resistance versus beta cell dysfunction differs among individuals with some having primarily insulin resistance and only a minor defect in insulin secretion and others with slight insulin resistance and primarily a lack of insulin secretion. Other potentially important mechanisms associated with type 2 diabetes and insulin resistance include: increased breakdown of lipids within fat cells, resistance to and lack ofincretin, high glucagon levels in the blood, increased retention of salt and water by the kidneys, and inappropriate regulation of metabolism by the central nervous system. However not all people with insulin resistance develop diabetes, since an impairment of insulin secretion by pancreatic beta cells is also required2.
Medications for Type 2 Diabetes mellitus
There are several classes of anti-diabetic medications available. Metformin is generally recommended as a first line treatment as there is some evidence that it decreases mortality4. A second oral agent of another class may be used if metformin is not sufficient9. Other classes of medications include: sulfonylureas, nonsulfonylurea secretagogues, alpha glucosidase inhibitors, thiazolidinediones, glucagon-like peptide-1 analog, and dipeptidyl peptidase-4 inhibitors4, 10. Metformin should not be used in those with severe kidney or liver problems11. Injections of insulin may either be added to oral medication or used alone. Most people do not initially need insulin. When it is used, a long-acting formulation is typically added at night, with oral medications being continued. Doses are then increased to effect (blood sugar levels being well controlled).
When nightly insulin is insufficient twice daily insulin may achieve better control. The long acting insulins, glargine and detemir, do not appear much better than neutral protamine Hagedorn (NPH) insulin but have a significantly greater cost making them, as of 2010, not cost effective12. In those who are pregnant insulin is generally the treatment of choice.
Introduction about TAK-875
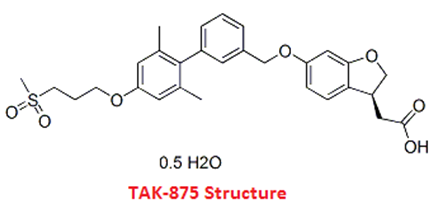
A study published Online First in The Lancet, states that TAK-87513(Structure is shown below), a new medicine used for treating type 2 diabetes, is a safe way to improve the control of blood sugar and is said to have minimal risk of low blood sugar. However, there are some side effects. TAK-875, which is an oral drug and is glucose-dependent, works by boosting insulin secretion. This makes it possible for the drug to help control blood sugar levels, without affecting insulin secretion if the levels of glucose are normal. Therefore, there is no risk of hypoglycaemia (low blood sugar)
G protein-coupled receptor 40 (GPR40), or free fatty acid receptor 1 (FFA1), is a vital component for keeping insulin levels regular. FFA1 jump starts the release of insulin from pancreatic β-cells when fatty acids and glucose are higher in the blood. For example, when a person eats their glucose and fatty acid levels rise. When the insulin in released, the glucose levels are lowered. Medicines that start the FFAR1 receptor may be effective in controlling blood sugar levels. During their study, Charles Burant, from the University of Michigan Medical School Michigan, USA, and his time recruited 426 patients living with type 2 diabetes, all of whom were having trouble maintaining normal blood sugar levels with the use of diet, exercise, or metformin treatment. 303 of the patients were given 1 of 5 doses of the TAK-875, 61 were given a placebo, and 62 were given glimepride. At the beginning of the study, glycosylated haemoglobin levels had already changed and by week 12, all of the people who had taken the TAK-875 had HbA1c levels that were lower than the levels of those who had taken the placebo. HbA1c levels among the patients who had taken glimepride were also lowered.
When the dose of TAK-875 was at least 25 mg, the people who had taken it were twice as likely to meet the American Diabetics Association's goal of HbA1c, about 33-48%, than those who were given the placebo, which was 19%. 40% of the patients who had taken glimepride had levels that met the American Diabetics Association's goal. Side effects due to treatment were the same for the TAK-875 group and the placebo group - 49% in all of the TAK-875 groups, and 48% in the placebo group. The side effects were more prevalent in the glimepride group at 61%; this was because of the greater risk of hypoglycaemia.
New drug targets have been under research in order to explore alternative drugs to promote insulin secretion in patients with type-2 diabetes mellitus14. One of the most researched targets amongst these is the G-protein coupled receptor-40 (GPCR-40) or free-fatty acid receptor-1 (FFAR1). GPCR-40 or the FFAR1 is found in the pancreatic β-cells, which secrete insulin. The FFAR1 receptors are activated by short and long-chain free fatty acids. Thus, they are activated when the free fatty acid levels in the blood are high, for example, after a meal. The activation results in insulin secretion. The FFAR1 receptors have been explored as a target for the treatment of diabetes. A phase-2 clinical trial was recently completed which assessed the potential of TAK-875 in achieving control of blood glucose levels without causing hypoglycaemia or low sugar levels TAK-875 brings about its action by the activation of FFAR1 receptors. Four hundred and twenty six patients with type-2 diabetes mellitus were included in this study. These were patients who did not respond to diet or metformin. The patients were divided randomly into three study groups: the first group which received TAK-875, the second group received glimepiride 4 mg once daily and the third group received placebo for over a period of twelve weeks. The achievement of glycaemic control was measured using the gylcosylated haemoglobin percentage (HbA1c) from the baseline till the end of the study.
A significant reduction in HbA1c was observed by the researchers in the group receiving TAK-875. The researchers also observed that hypoglycemic events were reported to be higher in the group receiving glimepiride as compared to placebo or TAK-875. The researchers thus concluded that activation of FFAR1 is a viable therapeutic target for the treatment of type 2 diabetes mellitus. Free fatty acid receptor 1 (FFA1), also known as G protein-coupled receptor 40 (GPR40), plays a vital role in stimulating and regulating the production of insulin. It works by boosting the release of insulin from pancreatic β-cells when glucose and fatty acids rise in the blood, such as after a meal. The release of insulin results in a fall in blood glucose levels. Drugs that activate the FFAR1 receptor have the potential to help diabetics release more insulin and improve control of blood glucose levels. About 2 percent of those receiving TAK-875 in the trial developed hypoglycaemia, a complication in which blood sugar is lowered too much, compared with 19 percent of those receiving glimepiride, the researchers wrote. About half of the TAK-875 group experienced an adverse side effect of any kind, compared with 61 percent of those in the glimepiride group15. Authors write that they are “excited about the potential of TAK-875 and are eager to conduct larger trials to find out how well this drug works, how safe it is and what its place is in the treatment of diabetes.”
Conclusion
It may be concluded that TAK-875, a new treatment for type 2 diabetes, improves blood sugar control and is equally effective as glimepiride, but has a significantly lower risk of creating a dangerous drop in blood sugar, called hypoglycaemia, according to a new study. TAK-875 is a novel oral medication designed to enhance insulin secretion in a glucose-dependant manner, which means that it has no effect on insulin secretion when glucose levels are normal, and as such has the potential to improve the control of blood sugar levels without the risk of hypoglycaemia. The drug targets cells in the pancreas that stimulate the production of insulin, without the risk of hypoglycaemia. Compared to the popular diabetes drug, glimepiride, patients studied had less risk of developing low blood sugar. If levels are normal, TAK-875 has no effect. Results of a Phase 2 clinical trial, published in the journal Lancet, found the drug worked well to lower HbA1C levels in patients with Type 2 diabetes who failed to keep the disease under control with diet, exercise or the diabetes drug metformin.
TAK-875 is a potent, selective and orally bioavailable GPR40 agonist with an EC50 of 0.072 μM. TAK-875 is a new agent applied in the treatment of type 2 diabetes. TAK-875 not only elevated the levels of intra-cellular inositol monophosphate as well as calcium contents in rat insulinoma INS-1 833/15 cells but also improved the tolerance of glucose and amplified insulin secretion when orally administered in tolerance test. However, TAK-875 didn’t increase the secretion of insulin and cause hypoglycaemia when 30 mg/kg dosage of TAK-875 was given in fasted normal Sprague Dawley rats. Conversely, TAK-875 with a dosage of 10 mg/kg (p.o.) not only significantly improved plasma insulin levels but also decreased fasting hyperglycemia in male Zucker diabetic fatty rats16, 17.
REFERENCES
1. David G. Gardner, Dolores (2011): Greenspan's basic & clinical endocrinology: McGraw Hill Medical Publishers, New York, Edn 9, Chapter 17.
2. Wild S, Roglic G, Green A, Sicree R, King H (2004): "Global prevalence of diabetes: estimates for 2000 and projections for 2030", Diabetes Care, 27 (5),1047– 1053
3. Fasanmade OA, Odeniyi IA, Ogbera AO (2008): "Diabetic ketoacidosis: diagnosis and management", African journal of medicine and medical sciences, 37 (2), 99–105.
4. Ripsin CM, Kang H, Urban RJ (2009): "Management of blood glucose in type 2 diabetes mellitus", Am Fam Physician, 79 (1), 29–36.
5. Risérus U, Willett WC, Hu FB (2009): "Dietary fats and prevention of type 2 diabetes", Progress in Lipid Research, 48 (1), 44–51.
6. Touma C, Pannain S (2011): "Does lack of sleep cause diabetes? Cleveland Clinic journal of medicine, 78 (8), 549–58.
7. Christian P, Stewart CP (2010): "Maternal micronutrient deficiency, fetal development, and the risk of chronic disease", The Journal of nutrition, 140 (3), 437–45.
8. Herder C, Roden M (2011): "Genetics of type 2 diabetes: pathophysiologic and clinical relevance", European journal of clinical investigation, 41 (6), 679–92.
9. Qaseem A, Humphrey LL, Sweet DE, M Shekelle P, Clinical Guidelines Committee of the American College of Physicians (2012): “Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians, Annals of Internal Medicine, 156(3), 218-231.
10. American Diabetes, Association (2012): "Standards of medical care in diabetes--2012", Diabetes Care, 35 Suppl 1, S11–63.
11. Vijan S (2010): “Type 2 diabetes”, Annals of internal medicine, 152(5), ITC31-15; quiz ITC 316.
12. Waugh N, Cummins E, Royle P, Clar C, Marien M, Richter B, Philip S (2010): "Newer agents for blood glucose control in type 2 diabetes: systematic review and economic evaluation", Health technology assessment (Winchester, England), 14 (36), 1–248.
13. medicalnewstoday.com/articles/242201.php
14. medindia.net/news/healthinfocus/tak-875-versus-placebo-or-glimepiride-in-type-2-diabetes-mellitus-99014-1.htm
15. Prof Charles F Burant, Prabhakar Viswanathan, John Marcinak, Charlie Cao, et al (2012): TAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomized, double-blind, placebo-controlled trial, The Lancet, 379(9824), 1403-1411.
16. clinicaltrials.gov/ct2/show/NCT00949091
17. Diabetes Drug Improves Glucose Control without increasing Risk of Hypoglycaemia (2012), Pharma Times, 44(8), 33.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to PharmaTutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









