About Author:
Rohan Kiran Kohok
M.Sc, Toxicology
University of Surrey, U.K.
rohankohok26@gmail.com
Abstract:-
Xenobiotic is a chemical compound for example a pesticide, drug, and carcinogen that is foreign to living organism’s biological systems. Human poisoning occurs when xenobiotic compound concentration increases beyond the level of human body’s ability to resist (metabolise) it. Natural compounds can also act as a xenobiotic if they are taken up by organisms which are unable to digest and excrete it from the body. Following there are two such reports on human poisoning caused by xenobiotic compounds.
REFERENCE ID: PHARMATUTOR-ART-1810
Case of Amatoxin Poisoning in the State of Texas.
Introduction:-
There are many thousands species of mushrooms in world and among them nearly 50 -100 of them are poisonous to humans. Mushrooms are ubiquitous and they can grow almost everywhere, they can be found in wood, near road side, yards, some of them are displayed in grocery store as well(Broussard et al.,2001, Adenipekun Gbolagade, 2006, Eren et al., 2010).Several cases have been reported in United States in different states, and Amanita species is famous among them. Recent literature suggests that there are more than 200 species of wild mushrooms in number of states of United States and specifically in Texas. Among the different species of Amanita, A. phalloides has the highest toxin content and is the most poisonous as it can be life threatening (Barry JD et al., 2009, Karlson et al., 2003). This case represents mycetismus from mushroom poisoning in Houston, Texas. Later part discusses the mechanism of toxicity and treatment options.
Case:-
In Houston, Texas of United States of America (U.S.A.) a 64 year-old Chinese female was treated for Amatoxin poisoning for 3days. She vomited at home, her vomit was clear in which there was no blood and she also had episodes of watery diarrhoea without blood. She had a history of abdominal pain mostly in lower abdomen. On the basis of these symptoms she was diagnosed with gastroenteritis in nearby local hospital. She was discharged with dosages on ciprofloxacin and loperamide. As this treatment failed to improve her health symptoms, she was brought to the The Methodist Hospital. The patient also had past history of hypertension so she was regularly taking Chinese herbal medicines. Her physical examination was overall fine. But when tests were carried out it was observed that, she had a maximum temperature of 97°F, a blood pressure of 140/70 on sitting and 135/70 on standing, a heart rate of 82, a respiratory rate of 16 and an oxygen ratio of 97%. Her lab session reports concluded negative hepatitis serologies and white blood cell count (WBC) 13.5, alanine aminotransferase (ALT) blood test 231, international normalized ratio (INR)1.3, aspartateaminotransferase test (AST) 375, prothrombin 15.7 levels. Her abdominal ultra sound test was also normal. Then finally upon further investigations of her history it was found that, she and her husband had picked up wild mushroom from the sidewalk of nearby Houston area. She cooked those wild mushrooms for lunch and dinner. As she was admitted to the hospital, for elevation in liver enzymes, she continued to show symptoms of nausea and vomiting. Initially she was started on N-acetylcysteine, and further poison control centre was contacted for patients treatment. They further identified the mushroom from the Amanita species. Due to acute liver injury, as she was admitted to hospital she began to have elevated levels of liver enzymes, and at one point of time, her prothrombin(fig. 1(a)) andinternational normalized ratioINR levels were also elevated during the hospital course (fig. 1 (b)).

Figure 1(a):- Elevation of prothrombin time throughout the hospital course.
(Wei-Chung Chen et al., 2012)
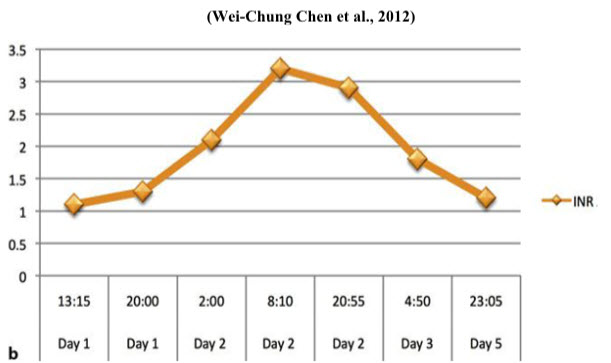
Figure 1 (b):- Elevation ofinternational normalized ratioINR throughout the hospital course. (Wei-Chung Chen et al., 2012)
Her aspartate aminotransferase test (AST) was 1,378 and alanine aminotransferase (ALT) was 1,227 (fig. 2).
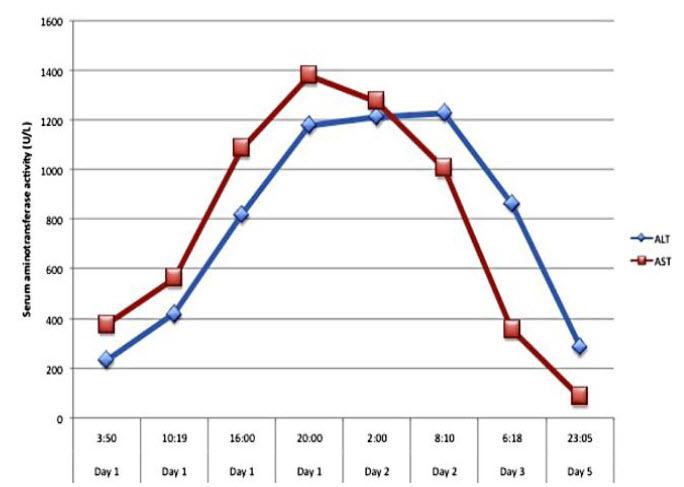
Figure 2:- Increase in level of liver enzymes which indicates liver injury.
(Wei-Chung Chen et al., 2012)
Due to liver injury she was transferred to intensive care unit for observation and care. Her husband was also admitted to hospital as he showed similar symptoms. But he only showed slight increase in liver enzymes as he did not eat much. Hence he only required supportive care throughout hospital treatment, later on he was discharged. For lady the hepatology department was consulted for acute liver injury. And she was given penicillin G, as later on her liver enzymes test continued to improve. In a few days after treatment she and her husband were discharged (Wei-Chung Chen et al., 2012).
Mechanism of Action:-
Mycetismus from mushroom can be life threatening. Ingestion of wild species like Amanita can lead to acute liver injury or hepatic failure which results in hepatorenal syndrome, encephalopathy and death (Broussard et al., 2001). Amanita poisoning occurs mainly in 3 stages. In the first phase, called as incubation phase, it usually occur 6 to 12 hrs after ingestion. Here, the person may or may not show any symptoms. The second phase called the gastrointestinal phase takes 6-18 hrs after ingestion of mushroom. In this patients develop nausea,vomiting ,diarrhea and abdominal pain for up to 24 hours. The last phase is called the cytotoxic stage and it occurs in 24 -48 hrs. In this phase the patients starts to show signs of liver damages as there is a complete elevation in liver enzymes, ammonia levels and prothrombin time (Madhok et al., 2007). There are different amatoxins isolated alpha, beta gammas (amanitins). Among them, alpha amanitin is mainly responsible and famous for toxicity. After ingestion of Amanita mushroom in humans this toxin is absorbed across the intestine and 60% of it is excreted via bile. Compared to other poisonous toxins, amatoxins has a prolonged enterohepatic circulation, which can result in acute liver injury or failure (Madhok et al., 2006). In liver it is (recirculation) absorbed by hepatocytes. It causes inhibition of mRNA synthesis as it interrupts functions of structural proteins and it also inhibits RNA polymerase II, leading to necrosis of liver. In many severe cases liver transplantation is necessary for survival. (Broussard et al., 2001)
Treatment:-
There are considerable treatment options available for amatoxins poisoning. Commonly used is the activated charcoal as it (toxin) has high affinity for charcoal; it slows down the absorption of toxin through intestine (Khuu L et al., 1993). Another widely used option is Penicillin G; it slows the rapid progression of encephalopathy. It also competes with binding of amatoxin on binding sites for the structural serum proteins which prevents liver hepatocytes uptake (French LK et al., 2011). Beta- lactum antibiotic ceftazidime is administered 4.5 g intravenously (i.v.) every 2 hrs. It is found to be more useful in comparison with penicillin G. A cytochrome P450 inhibitor cimetidine is an antioxidant agent is given with penicillin G at a dose of 300 mg intravenously (i.v.) every 8 hrs. Vitamin C is used as a hepatocyte protector in treatment of mushroom poisoning as it inhibits lipids peroxidation. Thioctic acid gives therapeutic effect on amatoxin poisoning by acting as a free radical scavenger (French LK et al., 2011, Nouguier-Soule, et al., 2002). But in many severe cases of liver transplant is necessary for survival.
Conclusion:-
New cases of Amanita poisoning are emerging, so health care providers should increase collaboration with poison control units to better diagnose patients with poisoning. There should be better awareness of the serious health issues from mushroom poisoning, such that immediate action plan can be provided for these patients.
Acute Liver Failure Due to Metastatic
Medullary Thyroid Cancer: a case report.
Introduction
Many Acute liver failures (ALF) have been reported due to liver metastases. But these are largely confined to lung, breast, gastric, cancers and non-Hodgkin’s lymphoma and Hodgkin’s disease (D. Rowbotham et al., 1998, P. Rajvanshi et al., 2007). This case represents metastasis of lesions and might be the first case in which Medullary thyroid cancer (MTC) resulted in acute liver failure.
Case:-
A 59 year old male without any previous medical history was admitted in Rochester in United States of America (USA), complained for 4 months history of neck pain. The patient was a school teacher without any habit of alcohol, tobacco, or illicit drug useas well as without any history of recent travel, occupational or chemical exposure.The biopsies with immuno histochemical staining consistently showed Medullary thyroid cancer (MTC).There was no family history of thyroid cancer or any prior neck and head radiation. Screening report endocrine gene mutation was negative. His computerized tomography (CT) scan of neck region showed heterogeneous volume of mass in the isthmus and the right lobe of the thymus. His carcinoembryonic antigen (CEA) was elevated up to 9,483 ng/mL(normal range: 0–5 ng/mL) , calcitonin was at 4,402pg/ml(normal range: 0–19 pg/mL) and thyroid stimulating hormone (TSH) was 2.5 μU/mL (normal range: 0.4–5 μU/mL).Multiple hypo dense lesions were observed in liver as abdominal computerized tomography (CT) scan was taken (Fig 1).
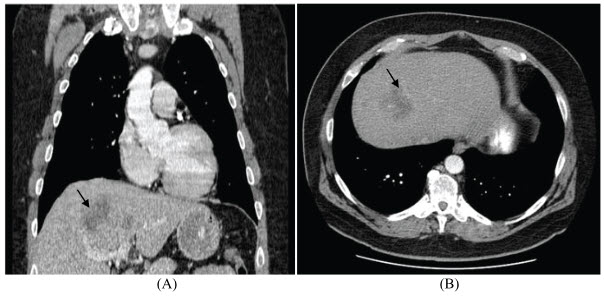
Figure 1:- Lesions in liver seen in abdominal CT scan (shown by arrow)
Source:-J. Badamas et al., 2011
His biochemical tests were completely normal. The Positron emission tomography (PET) scan technique three- dimensional image showed foci of acute uptake of radiopharmaceutical F-18 Fluoro-2-Deoxyglucose (F-18 FDG) in the chest, neck and liver regions. Among them largest focus was observed in the right hepatic lobe, same area was identified in the computerized tomography (CT) scan (figure 2).
The local hospital confirmed the Medullary thyroid cancer (MTC) from the histopathological examination of thyroid specimens. The carcinoma extended as it involved adjacent adipose tissues and muscles, as all dissected cervical lymph nodes were positive for metastases. After three weeks before the planned chemotherapy operation, suddenly the patient developed confusion, jaundice, fever. As there was concern of acute liver failure, he was immediately transferred to Saint Marys Hospital in United States of America (USA).The patient was awake but disoriented. There was no bipedal edema, flank. His biochemical liver enzymes tests were modestly elevated than normal. Blood cultures from the other hospital and the test for the autoimmune diseases, hepatitis were negative. His medications were fentanyl 25mcg patch and multivitamin. Ultra sound test with Doppler evaluation showed elevation of focal lesions in liver with heterogeneity and constant progression of liver metastases. No evidence was observed for bile transport obstruction, hepatic occlusion or other gall bladder diseases (J. Badamas et al., 2011).
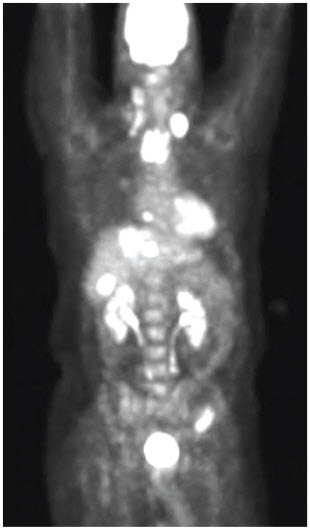
Figure 2:- Positron emission tomography (PET)
scan showing acute uptake in the neck,
chest and liver.(Shown by arrows)
Source:-J. Badamas et al.,2011
Later on he was treated with aggressive antibiotic coverage like rifaximin administration, but still his mental and physical condition was deteriorating. His condition started to get worse in spite of medication there was no positive response from the body. So in the view of this situation the family decided to proceed with palliation and end-of-life care support. The patient then suffered shock, hepatic coma, and multi organ failure. He expired on day 4 when he was admitted to Saint Marys Hospital. Post-mortem examination was declined by the members of the family.
Discussion:-
In a series of incidences in patients with Acute liver failure (ALF) at Kings College Hospital overall mortality rate was 94 %( D. Rowbotham et al., 1998). This case represents a rare unusual situation of metastasis of Medullary thyroid cancer (MTC), which caused hepaticcoma, jaundice, encephalopathy which resulted in Acute liver failure (ALF). Usually increase of aminotransferase levels and alkaline phosphatase are used as markers of metastatic liver diseases. In this case as there are no other etiologies of acute liver failure (ALF) and elevated calcitonin levels only points out that metastases in liver is due to Medullary thyroid cancer (MTC). There have been cases in which neoplastic lesions are responsible which have been correlated with modestly elevated liver enzymes test (P. Rajvanshi et al., 2007). Based on the experiences of slightly related cases there might be following reasons behind it: 1) nonocclusive liver ischemia due to shock from circulatory dysfunction, sepsis. 2) Loss of important hepatic liver cells and there replacement by metastatic tumour cells.3) formation of non occlusive tumour thrombi (H. B. Harrison et al., 1981, P. Rajvanshi et al., 2007). Patient was not having any family history of thyroid or any other cancer and there was no chemical exposure. The causes of the cancerous lesions are still unknown. It might be from any known or unknown xenobiotic compound as well. However sporadic Medullary thyroid cancer (MTC) may arise from occasional somatic mutations. Sometimes macroscopic liver metastases may also be missed as the lesions patterns might be difficult trace under radiographic detection (D. W. Ball, 2007). Early occurrences and tumours distant metastases with only sign of elevation in calcitonin levels may produce harmful consequences (G. Tsvetov et al., 2007).
Conclusion:-
This case represents unusual acute liver failure due to Medullary thyroid cancer (MTC). It strongly represents that Medullary thyroid cancer (MTC) can cause acute liver failure and it should also be studied and included in list of possible causes of Acute liver failure (ALF).
References
Adenipekun, C.O. and J. S. Gbolagade, 2006. Nutritional requirements of Pleurotus florida (Mont.) singer, a Nigerian mushroom. Pak. J. Nutr., 5: 597-600.
Barbee GA, Berry-Cabán CS, Barry JD, et al: Analysis of mushroom exposures in Texas requiring hospitalization, 2005–2006. J Med Toxicol 2009; 5:59–62.
Broussard CN, Aggarwal A, Lacey SR, Post AB, Gramlich T, Henderson JM, Younossi ZM: Mushroom poisoning – from diarrhea to liver transplantation. Am J Gastroenterol 2001; 96:3195–3198.
D. Rowbotham, J. Wendon, and R. Williams, “Acute liver failure secondary to hepatic infiltration: a single centre experienceof 18 cases,” Gut, vol. 42, no. 4, pp. 576–580, 1998.
D. W. Ball, “Medullary thyroid cancer: monitoring and therapy,”Endocrinology and Metabolism Clinics of North America,vol. 36, no. 3, pp. 823–837, 2007.
Emmanuel C. Gorospe , Jemilat Badamas. (28 December 2011). Acute Liver Failure Secondary to Metastatic Medullary Thyroid Cancer. Case Reports in Hepatology. 2011 (4), 4-8.
Enjalbert F, Rapior S, Nouguier-Soule, et al: Treatment of amatoxin poisoning: 20-year retrospective analysis. J Toxicol Clin Toxicol 2002; 40:715–757.
Eren, S.H., Y. Demirel, S. Ugurlu, I. Kormaz, C. Aktas and F.M.K. Guven , 2010. Mushroom
Poisoning: Retrospective analysis of 294 cases. Clinics, 65: 491-496.
French LK, Hendrickson RG, Horowitz BZ: Amanita phalloides poisoning. Clin Toxicol 2011; 49:128–129.
Karlson-Stiber C, Persson H: Cytotoxic fungi – an overview. Toxicon 2003; 42:339–349.
Madhok M: Amanita bisporigera: ingestion and death from mistaken identity. Minn Med 2007; 90:48–50.
Madhok M, Scalzo AJ, Blume CM, Neuschwander-Tetri BA, Weber JA, Thompson MW: Amanita bisporigera ingestion: mistaken identity, dose-related toxicity, and improvement despite severe hepatotoxicity. Pediatr Emerg Care 2006; 22:177–180.
O’Brien BL, Khuu L: A fatal Sunday brunch: Amanita mushrooms poisoning in a Gulf Coast family. Am J Gastroenterol 1996; 91:581–583.
P. Rajvanshi, K. V. Kowdley,W. K.Hirota, J. B. Meyers, and E.B. Keeffe, “Fulminant hepatic failure secondary to neoplasticinfiltration of the liver,” Journal of Clinical Gastroenterology,vol. 39, no. 4, pp. 339–343, 2005.
S. Grozinsky-Glasberg, C. A. Benbassat, G. Tsvetov et al., “Medullary thyroid cancer: a retrospective analysis of a cohorttreated at a single tertiary care center between 1970 and 2005,”Thyroid, vol. 17, no. 6, pp. 549–556, 2007.
Wei-Chung Chen, Mahwash Kassi, Umair Saeed Catherine T. Frenette b. (June 7 2012). A Rare Case of Amatoxin Poisoning in the State of Texas. Case Reports in Gastroenterology. Vol. 6 (1), 350–357.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









