{ DOWNLOAD AS PDF }
About Authors:
M.S.Umashankar, K.S.Lakshmi, A.Bharath Kumar*, A.Porselvi
Department of PharmacyPractice SRM College of Pharmacy,SRM University. Kattankulathur.Tamilnadu.India.
abharatpharma@gmail.com*
ABSTRACT : Diabetic nephropathy is a type of progressive kidney disease that may occur in people who have diabetes. It affects people with type 1 and type 2 diabetes and risk increases with the duration of the disease and other risk factors like high blood pressure and a family history of kidney disease.Kidney is made of hundreds of thousands of small units called nephrons.These structures filter the blood and helps to remove waste from the body, and control fluid balance.Clinical conditions we can investigate the symptoms like Persistent albuminuria (>300 mg/d or >200 μg/min) that is confirmed on at least 2 occasions 3-6 months and Progressive decline in the glomerular filtration rate,severe tiredness,headaches,general feeling of illness,frequent voiding, lack of appetite, itchy skin, and leg swelling.Diabetic nephropathy is diagnosed after a routine urinalysis and screening for microalbuminuria and fasting,random blood sugar level,glomeluar filteration rate,serum creatinine,creatinine clearance is used to confirm the disease.Reduction of kidney damage by controlling blood sugar levels,controlling blood pressure through the eating healthy foods and getting regular exercise.The evidence suggest that approaching early treatment,regular Patient follow-up will delays and prevents the onset of diabetic nephropathy.Clinical Pharmacist having significant role in providing education on disease related issues and he work with both the patient and physician to ensure that patient is to achieve optimal blood pressure, blood glucose, and lipid control, and that other risk factors and lifestyle modifications are being addressed.Appropriate control of their diabetes with nephropathy can be influenced through proper education and counselling by the clinical Pharmacists in clinical care.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2503
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 5, Issue 7 Received On: 27/02/2017; Accepted On: 27/03/2017; Published On: 01/07/2017 How to cite this article: Umashankar MS,Lakshmi KS, Kumar AB, Porselvi A;A review on clinical pharmacist care for management of Diabetic Nephropathy in clinical practice; PharmaTutor; 2017; 5(7); 7-15 |
INTRODUCTION
Nephropathy means kidney disease or damage. Diabetic nephropathy is damage to your kidneys caused by diabetes. In severe cases it can lead to kidney failure. Diabetic nephropathy, also known as Kimmelstiel-Wilson syndrome or nodular diabetic glomerulosclerosis or intercapillary glomerulonephritis, is a clinical syndrome characterized by albuminuria (>300 mg/day or >200 mcg/min) confirmed on at least two occasions 3-6 months apart, permanent and irreversible decrease in glomerular filtration rate[1].
Diabetic nephropathy is a condition that occurs in diabetes patients when the kidneys are damaged. During the early stages there are no symptoms and this allows patients to remain undiagnosed for years. The earliest sign of disease is associated with low but abnormal levels of protein in the urine.
Diabetic nephropathy is a type of progressive kidney disease that may occur in people who have diabetes. It affects people with type 1 and type 2 diabetes and risk increases with the duration of the disease and other risk factors like high blood pressure and a family history of kidney disease.
Diabetes is the leading cause of ESRD because diabetic nephropathy develops in 30 to 40% of patients.
Diabetic nephropathy is a clinical syndrome characterized by the occurrence of persistent microalbuminuria in concomitance with insulin or non–insulin-dependent diabetes.This nephropathy has a long natural history in type 1 diabetes.Initially, the patient shows hyperfiltration, represented by high values of GFR, approximately doubling of the normal value, and occasional occurrence of microalbuminuria[2].
Multigenetic predisposition contributes in the development of diabetic nephropathy, thus supporting that many factors are involved in the pathogenesis of the disease. Hyperglycemia induces renal damage directly or through hemodynamic modifications. It induces activation of protein kinase , increased production of advanced glycosylation end products, and diacylglycerol synthesis. In addition, it is responsible for hemodynamic alterations such as glomerular hyperfiltration, shear stress, and microalbuminuria. These alterations contribute to an abnormal stimulation of resident renal cells.
Diabetic nephropathy is also associated with an increased risk of vascular disease and patient mortality. Aggressive management of hypertension to reduce micro albuminuria, together with tight glycaemic control are important therapeutic strategies for renal and vascular disease prevention in type2 diabetes mellitus.
The increasing number of people with diabetes has had a major impact on the prevalence of diabetic nephropathy Diabetic nephropathy,which occurs in 20% to 40% of all patients with type 2 diabetes mellitus is a metabolic disorder with high morbidity and mortality and is the leading cause of end-stage renal disease (ESRD).The overall burden for people with diabetic nephropathy is extremely high because of the strong associations of diabetic nephropathy and cardiovascular disease (CVD) with ESRD.
Diabetic nephropathy is the leading cause of kidney disease in patients starting renal replacement therapy and affects 40% of type 1 and type 2 diabetic patients. It increases the risk of death, mainly from cardiovascular causes, and is defined by increased urinary albumin excretion (UAE) in the absence of other renal diseases. Diabetic nephropathy is categorized into stages: microalbuminuria (UAE >20 μg/min and ≤199 μg/min) and macroalbuminuria (UAE ≥200 μg/min). Hyperglycemia, increased blood pressure levels, and genetic predisposition are the main risk factors for the development of diabetic nephropathy.
The kidneys are two bean-shaped organs that extract waste from blood, balance body fluids, form urine, and aid in other important functions of the body.
They reside against the back muscles in the upper abdominal cavity. They sit opposite each other on either side of the spine. The right kidney sits a little bit lower than the left to accommodate the liver[3].
When it comes to components of the urinary system, the kidneys are multi-functional powerhouses of activity.
Some of the core actions of the kidneys include:
• Waste excretion: There are many things your body doesn’t want inside of it. The kidneys filter out toxins, excess salts, and urea, a nitrogen-based waste created by cell metabolism. Urea is synthesized in the liver and transported through the blood to the kidneys for removal.
• Water level balancing: As the kidneys are key in the chemical breakdown of urine, they react to changes in the body’s water level throughout the day. As water intake decreases, the kidneys adjust accordingly and leave water in the body instead of helping excrete it.
• Blood pressure regulation: The kidneys need constant pressure to filter the blood. When it drops too low, the kidneys increase the pressure. One way is by producing a blood vessel-constricting protein (angiotensin) that also signals the body to retain sodium and water. Both the constriction and retention help restore normal blood pressure.
• Red blood cell regulation: When the kidneys don’t get enough oxygen, they send out a distress call in the form of erythropoietin, a hormone that stimulates the bone marrow to produce more oxygen-carrying red blood cells.
• Acid regulation: As cells metabolize, they produce acids. Foods we eat can either increase the acid in our body or neutralize it. If the body is to function properly, it needs to keep a healthy balance of these chemicals[4].
Epidemiology
Diabetes and its costs are a problem of enormous importance in the United States today.Costs of caring for the complications of diabetes account for 90% of the direct and indirect costs of diabetes care. Diabetic nephropathy accounts for 35% of ESRD in the United States today and costs approximately $50,000 per patient per year.
Types of kidney failure
Acute kidney injury
Acute kidney injury is sudden damage to the kidneys. In many cases it will be short term but in some people it may lead to long-term chronic kidney disease.
The main causes are:
• Damage to the actual kidney tissue caused by a drug, severe infection or radioactive dye
Chronic kidney disease
More often, kidney function worsens over a number of years. This is known as chronic kidney disease. Sometimes it can progress to end stage kidney disease, which requires dialysis or a kidney transplant to keep you alive.
There are different causes of chronic kidney disease, the key ones being :
• damaged blood vessels to the kidneys due to high blood pressure and diabetes
• Attacks on the kidney tissue by disease or the immune system (glomerulonephritis)
• The growth of cysts on the kidneys (polycystic kidney disease)
• damage due to backward flow of urine into the kidneys (reflux nephropathy)
• congenital abnormalities of the kidney or urinary tract
Kidney disease or kidney damage often occurs over time in people with diabetes. This type of kidney disease is called diabetic nephropathy.It is characterized by nephrotic syndrome and diffuse scarring of the glomeruli. It is due to longstanding diabetes mellitus, and is a prime reason for dialysis in many developed countries. Diabetic nephropathy is characterised by an increased urinary albumin excretion in the absence of other renal diseases. It is a common and often devastating complication of both type 1 and type 2 diabetes and is associated with increased cardiovascular mortality and a reduction in quality of life[5].
The structural abnormalities include hypertrophy of the kidney, increase in glomerular basementmembrane thickness, nodular and diffuse glomerulosclerosis tubularatrophy, and interstitial fibrosis.
Here are five stages in the development of diabetic nephropathy
Stage I :
• Hypertrophic hyper filtration. In this stage,GFR is either normal or increased.
• Stage I lasts approximately five years from the onset of the disease.
• The size of the kidneys is increased by approximately 20% and renal plasma flow is increased by 10%-15%, while albuminuria and blood pressure remain within the normal range.
Stage II
• The quiet stage. This stage starts approximately two years after the onset of the disease and is characterized by kidney damage with basement membrane thickening and mesangial proliferation.
• There are still no clinical signs of the disease. GFR returns to normal values. Many patients remain in this stage until the end of their life.
Stage III :
• The microalbuminuria stage (albumin 30-300 mg/dU) or initial nephropathy. This is the first clinically detectable sign of glomerular damage. It usually occurs five to ten years after the onset of the disease. Blood pressure may be increased or normal.
• Approximately 40% of patients reach this stage.
Stage IV :
• Chronic kidney failure (CKF) is the irreversible stage.
• Proteinuria develops (albumin > 300 mg/dU), GFR decreases below 60 mL/min/1.73 m and blood pressure increases above normal values.
Stage V :
• Terminal kidney failure (TKF) (GFR < 15 mL/min/1.73 m).
• Approximately 50% of the patients with TKF require kidney re placement therapy (peritoneal dialysis, hemodialysis, kidney transplantation).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Stages of chronic kidney disease
|
Stage |
Description |
GFR (mL/min) |
|
1 |
Kidney damage with normal or raised GFR |
≥90 |
|
2 |
Kidney damage with mild decrease in GFR |
60-89 |
|
3 |
Moderate decrease in GFR |
30-59 |
|
4 |
Severe decrease in GFR |
15-29 |
|
5 |
Kidney Failure |
<15 |
Diagnosis
Diabetic nephropathy is diagnosed using tests that check for a protein (albumin) in the urine, which points to kidney damage. An albumin urine test can detect very small amounts of protein in the urine that cannot be detected by a routine urine test, allowing early detection of nephropathy. Early detection is important, to prevent further damage to the kidneys. The results of two tests, done within a 3- to 6-month period, are needed to diagnose nephropathy[7,8].
Microalbuminuria urine test
A microalbuminuria urine test checks for albumin in your urine. Normal urine does not contain albumin, so the presence of the protein in your urine is a sign of kidney damage.
BUN blood test
A BUN blood test checks for the presence of urea nitrogen in your blood. Urea nitrogen forms when protein is broken down.
Serum creatinine blood test
• A serum creatinine blood test measures creatinine levels in blood.
• creatinine level to estimate glomerular filtration rate (eGFR), which helps to determine effectiveness of renal system.
Kidney biopsy
|
Albumin testing |
|
|
Type of diabetes |
When to begin yearly testing |
|
Type 1 diabetes |
After you have had diabetes for 5 years |
|
Type 2 diabetes |
When you are diagnosed with diabetes |
|
Diabetes present during childhood |
After age 10 and after the child has had diabetes for 5 years |
Laboratory Evaluation of Persons with Diabetic Nephropathy
|
Test |
Significant results |
|---|---|
|
Albumin in a 24-hour urine sample (mg of albumin per 24 hours) |
Microalbuminuria: 30 to 300 mg |
|
Macroalbuminuria: > 300 mg |
|
|
Estimated glomerular filtration rate |
Glomerular filtration rate hyperfiltration, with elevated glomerular filtration rate in early stages followed by linear decline until end-stage renal disease |
|
Random spot albumin/creatinine ratio (mg of albumin per g of creatinine) |
Microalbuminuria: 30 to 300 mg |
|
Macroalbuminuria: > 300 mg |
|
|
Renal biopsy (if unclear etiology) |
Light microscopy: glomerular sclerosis with nodular mesangial expansion and proliferation (Kimmelstiel-Wilson nodules) |
|
Electron microscopy: glomerular basement membrane thickening |
Risk factors :
Several factors may increase your risk of diabetic nephropathy, including:
• Diabetes, type 1 or 2
• High blood sugar (hyperglycemia) that's difficult to control
• High blood pressure (hypertension) that's difficult to control
• Being a smoker and having diabetes
• High blood cholesterol and having diabetes
• A family history of diabetes and kidney disease
• Genetics
• susceptibilityRace
• Elevated Blood pressure
• Elevated Blood sugar
• Hyperfiltration
• Age
• Male
• Gender
• Dyslipidemia
Pathophysiology
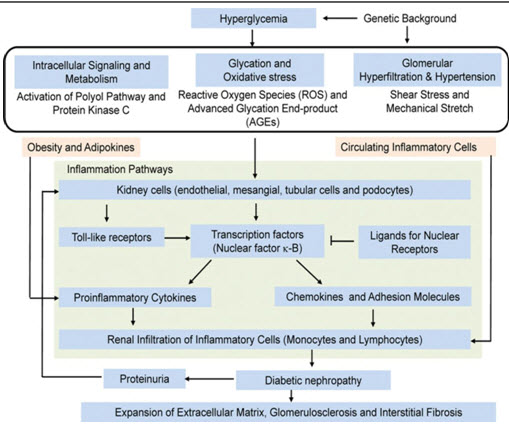
Fig 1 : Pathophysiology of diabetic nephropathy
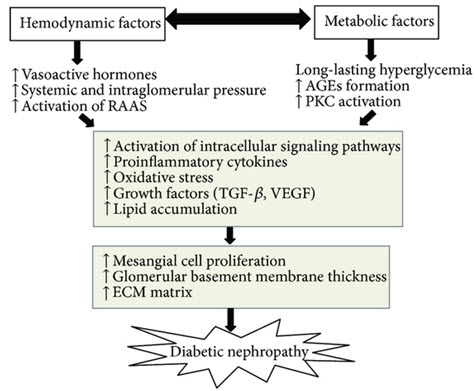
Fig 2 : Pathophysiology of diabetic nephropathy
Histopathological studies about diabetic nephropathy
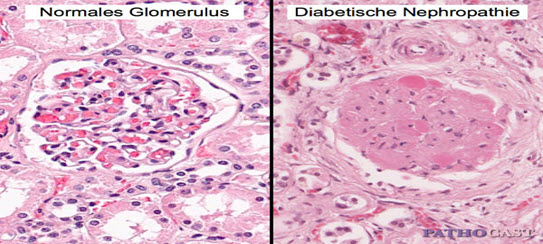
Fig 3: comparision of Histopathological studies about normal and diabetic nephropathy
People who have more severe and long-term (chronic) kidney disease may have symptoms such as :
Symptoms
In the early stages of diabetic nephropathy includes :
• Swelling of feet, ankles, hands or eyes
• Increased need to urinate
• Loss of appetite
• Persistent itching
• Fatigue
• Protein in the urine
• Albumin or protein in the urine
• High blood pressure
• High levels of blood urea nitrogen (BUN) and serum creatinine
• Morning sickness, nausea, and vomiting
• Weakness, paleness, and anemia
• Protein in the urine
• Confusion
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Complications
Complications of diabetic nephropathy may develop gradually over months or years.
They may include:
• Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema).
• A sudden rise in potassium levels in your blood (hyperkalemia).
• Heart and blood vessel disease (cardiovascular disease), possibly leading to stroke.
• Damage to the blood vessels of the retina (diabetic retinopathy).
• Anemia
• Foot sores, erectile dysfunction, diarrhea and other problems related to damaged nerves and blood vessels[9]
• Pregnancy complications that carry risks for the mother and the developing fetus.
Preventing kidney damage approaches
Here are some tips that can help you to prevent kidney damage :
• Good sugar control with diet and lifestyle.
• Following medication including insulin (if needed) is the most important.
• Monitoring of HbA1c (glycosylated hemoglobin) should be done every 3 months Monitor your blood pressure on a regular basis, and keep it under control.
• Keep cholesterol levels under control.
• Avoid tobacco in any form (smoking, chewing, etc..).
• Keep your weight under check.
• Avoid self medication, especially painkillers.
Management of Nephropathy
The management of nephropathy in diabetes should be multifaceted, advocating a healthy lifestyle and targeting all the individual renal and cardiovascular risk factors. The goal of the management is to reduce the risk of renal disease progression, as well as the risk of cardiovascular morbidities[10].
Glucose Control Regarding glycaemic control, the evidence for renoprotection of good glycaemic control is far stronger in the early stages of nephropathy, especially in the prevention of microalbuminuria. There is, however, supporting evidence to reach recommended HbA1c targets also in subjects with chronic kidney disease[7].
Renin-Angiotensin Inhibition In individuals with albuminuria, usage of an ACE-I or ARB is recommended even though the person is normotensive,thereby slowing the progression of renal disease and reducing the risk of end-stage renal disease. The benefits of ACE-I and ARBs increase as the levels of albuminuria rise.
Blood Pressure As in the prevention of nephropathy, blood pressure treatment is essential also in the later stages of nephropathy to reduce the risk of progression. The target blood pressure in subjects with diabetes and chronic kidney disease is <130/80 mmHg.Lowering of the systolic blood pressure even further might be of benefit, especially for subjects with high levels of albuminuria,but levels below 110 mmHg should, however, be avoided[11].
Dietary Protein Intake Protein intake might have an effect on progression of nephropathy and high-protein diets should be avoided. The optimal amount of protein intake is, however, debated. The American Diabetes Association does not recommend restricting protein intake below usual intake, but recognizes that some subjects with advancing kidney disease might benefit from protein restriction [12]. The guidelines of the National Kidney Foundation, on the other hand, recommend protein restriction to less than 0.8 g/kg bodyweight daily.
Hyperlipidemia There is suggestion that elevation in lipid levels may contribute to the development of glomerulosclerosis in chronic renal failure.
Approaches in Management of Diabetic Nephropathy
• Control of bloodsugar
• PrePrandial glucose:80-120mg/dL(wholeblood)90-130mg/dL (plasma)
• Bedtimeglucose:100-140mg/dL(wholeblood)110-150 mg/dL(plasma)
• Glycosylated hemoglobin:<7%
• Control of Blood Pressure(ADA, NKF Targets)<130/80mmHg in patients with proteinuria <1g/day.<125/75 mmHg in patients with proteinuria
• Control of Blood Lipids(ADATargets)
• LDL cholesterol <100mg/dL(firstpriority)
• HDLcholesterol>45mg/dL(secondpriority)
• Triglycerides <200mg/dL(secondpriority)[13]
|
Factor |
Prevention |
Management |
|
Glucose control |
HbA1c target ≤ 52 mmol/mol (7.0%). Less stringent goals if severe hypoglycaemia, cardiovascular disease or other co-morbidities, or short life expectancy. |
HbA1c target ≤ 52 mmol/mol (7.0%). Consider dose adjustments of glucose medication when eGFR declines. |
|
Blood pressure |
Anti-hypertensive treatment in all subjects if blood pressure >140/80-85 mmHg, or if albuminuria present. Target <140/80-85 mmHg. |
Anti-hypertensive treatment in all subjects. Target <130/80 mmHg. Consider dose adjustments of medication when GFR declines. |
|
ACE-I/ARBs |
In all subjects with blood pressure >140/80-85 mmHg and/or albuminuria. |
In all subjects, even if normotensive. |
|
Protein intake |
- |
Avoid high-protein intake. |
PREVENTION AND TREATMENT STRATEGIES
Significant progress has been made in recent years in understanding the pathophysiology, prevention, and treatment of diabetic nephropathy.
Newer therapeutic trends in management of diabetic nephropathy
Despite maximal RAS inhibition and other measures to control blood pressure and hyperglycemia, DN progression to ESRD remains intractable in many patients. Renewed understanding of the pathophysiology of DN has fueled the development of several potentially promising novel therapeutic options, and these are summarized below.
Pleotropic renoprotective effects of anti-diabetic drugs beyond glycemic control
Certain hypoglycemic agents have been shown to confer independent renoprotective effects beyond their hypoglycemic action. For instance, peroxisome proliferator activator receptor-gamma (PPAR-γ) agonists, also known as thiazolidinediones (TZD), have direct renoprotective effects in experimental models.
Glucagon-like peptide 1, an incretin which promotes insulin and suppresses glucagon release, is produced by the gut when food is ingested and it is degraded by dipeptidyl peptidase-4 (DPP-4).A novel group of hypoglycemic agents in the form of DPP-4 inhibitors have emerged in the treatment paradigm of DM and experimental models have indicated possible renoprotective benefits.
Vitamin D receptor activators
Vitamin D receptor (VDR) activators demonstrated anti-inflammatory and anti-proteinuric effects in animal models of Diabetic retinaopthy.Vitamin D Receptor Activation with Paricalcitol for Reduction of Albuminuria in Patients with Type 2 Diabetes) trial indicate that adjuvant paricalcitol at 2 μg/day lowers residual albuminuria in DN However, 42% of patients needed a reduced dose of paricalcitol due to poor tolerance, not to mention the additional drawback of the high cost of treatment. Therefore, concrete evidence demonstrating the successful use of VDR activators to retard the progression of DN is still awaited.
Sodium-glucose cotransporter 2 inhibition
Apart from their ability to enhance urinary glucose excretion and aid glycemic control, SGLT-2 inhibitors appear to also promote an attractive cardiovascular risk reduction.
Selective C-C chemokine receptor type 2 antagonism
Monocyte chemoattractant protein-1 (MCP-1), also called C-C chemokine ligand 2 (CCL2), one of the ligands for C-C chemokine receptor type 2 (CCR2), has been implicated not only in insulin resistance but also in progressive renal injury, and has been suggested to be a potential marker of renal disease.
Patient Counseling Points For Diabetic Nephropathic Patients
• Pharmacists are key in preventing these complications by educating patients on the significance of blood glucose monitoring, the use of blood glucose monitors, and the importance of achieving their blood glucose goals.
• Pharmacists should highlight the importance of strict compliance with their medications, as tight glucose control has been shown to prevent nephropathy.
• For both oral hypoglycemic agents and insulin, focusing on administration times and dosing schedules is an important way to ensure tight glucose control.
• It is crucial that pharmacists work with both the patient and physician to ensure that the patient is achieving optimal blood pressure,blood glucose,lipid control and that other cardiovascular risk factors such as obesity, smoking, and sedentary lifestyle are being addressed.
CONCLUSION Diabetes is a metabolic disorder which is characterized by abnormal insulin production.The prevention of diabetic nephropathy includes tight glycemic control,blood pressure control and use of medications like ACE inhibitors,statins,angiotensin receptor blocker will helpful for the Patients.Treating microalbuminuria with the use of ACE inhibitors and lowering blood pressure is the most important factor in saving the diabetic kidney from the downward path to End stage renal disease.clinical Pharmacist having significant role in providing education on disease related issues and he work with both the patient and physician to ensure that patient is achieving optimal control,lifestyle modifications are being addressed.Appropriate control of their diabetes with nephropathy can be influenced through proper education and counselling by the Pharmacists in clinical care.
REFERENCES
1. Foster, M.C., et al., Cross-classification of microalbuminuria and reduced glomerular filtration rate: associations between cardiovascular disease risk factors and clinical outcomes. Arch Intern Med, 2007. 167(13): p. 1386-92.
2. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet, 1998. 352(9131): p. 837-53.
3. American Diabetes Association,Standards of medical care in diabetes-2014. Diabetes Care, 2014. 37 Suppl 1: p. S14-80.
4. National Kidney Foundation, KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis, 2012. 60(5): p. 850-86.
5. Gaede, P., et al., Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med, 2003. 348(5): p. 383-93.
6. Dunkler, D., et al., Diet and kidney disease in high-risk individuals with type 2 diabetes mellitus. JAMA Intern Med, 2013. 173(18): p. 1682-92.
7. Lalau, J.D., et al.,Metformin and other antidiabetic agents in renal failure patients. Kidney Int, 2014.
8. Agarwal SK, Dash.Spectrum of Renal Disease in Indian Adults. JAPI 2000; 48: 594 -6.
9. Chugh KS, Kumar R, Sakhuja V, Pereira BJ, Gupta A.Nephropathy in type 2 diabetes mellitus in Third World Countries. Chandigarh Study. Int. J. Artif. Organs 1989;12: 299.
10. screening, Diagnosis, and Management of Diabetes-related Complications. In: Unger J. Diabetes Management in Primary Care. Philadelphia: Lippincott Williams & Wilkins; 2007:563-7.
11. Evans TC. American Diabetes Association. Standards of Medical Care in Diabetes-2008. Diabetes Care 2008;31:S12-54.
12. American Diabetes Association. Diabetic Nephropathy. Diabetes Care 2002;25:S86-88.
13. American Diabetes Association. Diabetic Nephropathy. Diabetes Care 2003;26:S94-98.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









